J. Robin Warren Perth, WA 6000, Australia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nobel Prizes in Physiology Or Medicine with an Emphasis on Bacteriology
J Med Bacteriol. Vol. 8, No. 3, 4 (2019): pp.49-57 jmb.tums.ac.ir Journal of Medical Bacteriology Nobel Prizes in Physiology or Medicine with an Emphasis on Bacteriology 1 1 2 Hamid Hakimi , Ebrahim Rezazadeh Zarandi , Siavash Assar , Omid Rezahosseini 3, Sepideh Assar 4, Roya Sadr-Mohammadi 5, Sahar Assar 6, Shokrollah Assar 7* 1 Department of Microbiology, Medical School, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. 2 Department of Anesthesiology, Medical School, Kerman University of Medical Sciences, Kerman, Iran. 3 Department of Infectious and Tropical Diseases, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran. 4 Department of Pathology, Dental School, Shiraz University of Medical Sciences, Shiraz, Iran. 5 Dental School, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. 6 Dental School, Shiraz University of Medical Sciences, Shiraz, Iran. 7 Department of Microbiology and Immunology of Infectious Diseases Research Center, Research Institute of Basic Medical Sciences, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. ARTICLE INFO ABSTRACT Article type: Background: Knowledge is an ocean without bound or shore, the seeker of knowledge is (like) the Review Article diver in those seas. Even if his life is a thousand years, he will never stop searching. This is the result Article history: of reflection in the book of development. Human beings are free and, to some extent, have the right to Received: 02 Feb 2019 choose, on the other hand, they are spiritually oriented and innovative, and for this reason, the new Revised: 28 Mar 2019 discovery and creativity are felt. This characteristic, which is in the nature of human beings, can be a Accepted: 06 May 2019 motive for the revision of life and its tools and products. -

EDITORIAL Year's Comments for 2005
EDITORIAL INTERNATIONAL MICROBIOLOGY (2005) 8:231-234 Year’s comments for 2005 Ricardo Guerrero Editor-in-Chief, INT. MICROBIOL. E-mail: [email protected] For several years, new sequences of microbial genomes have dogma. Conclusive evidence for a pathogenic role of H. pylori been the highlights of microbiology and a major topic of our came from trials showing that elimination of the bacterium dra- yearly comments. But sequencing has become “routine” and, at matically changed the clinical course of ulcer. This finding was the time this editorial is being written, the complete sequences confirmed by Marshall, who swallowed a broth of H. pylori and of 284 prokaryotic genomes and 40 eukaryotic genomes have soon thereafter developed gastritis, the prelude to ulcers. He been published. This allows us to focus our comments on those recovered from the disease after treatment with antibiotics. events from 2005 that have attracted the attention of both (Warren could not join him in the experiment because he already researchers and the media. These include the Nobel Prize in suffered from peptic ulcer.) Subsequently, the two investigators Physiology or Medicine, which was awarded for the discovery successfully treated other people suffering from ulcers, in the of the role of Helicobacter pylori as the causal agent of gastric process clearly identifying the bacterium as the culprit. In 1994, ulcers; the worldwide effort to fight malaria, a disease that main- H. pylori was the first bacterium, and the second infectious ly affects developing countries; and the global spread of avian organism after hepatitis B virus, to be classified as a class I car- influenza, which is becoming a panzootic. -

ILAE Historical Wall02.Indd 10 6/12/09 12:04:44 PM
2000–2009 2001 2002 2003 2005 2006 2007 2008 Tim Hunt Robert Horvitz Sir Peter Mansfi eld Barry Marshall Craig Mello Oliver Smithies Luc Montagnier 2000 2000 2001 2002 2004 2005 2007 2008 Arvid Carlsson Eric Kandel Sir Paul Nurse John Sulston Richard Axel Robin Warren Mario Capecchi Harald zur Hauser Nobel Prizes 2000000 2001001 2002002 2003003 200404 2006006 2007007 2008008 Paul Greengard Leland Hartwell Sydney Brenner Paul Lauterbur Linda Buck Andrew Fire Sir Martin Evans Françoise Barré-Sinoussi in Medicine and Physiology 2000 1st Congress of the Latin American Region – in Santiago 2005 ILAE archives moved to Zurich to become publicly available 2000 Zonismide licensed for epilepsy in the US and indexed 2001 Epilepsia changes publishers – to Blackwell 2005 26th International Epilepsy Congress – 2001 Epilepsia introduces on–line submission and reviewing in Paris with 5060 delegates 2001 24th International Epilepsy Congress – in Buenos Aires 2005 Bangladesh, China, Costa Rica, Cyprus, Kazakhstan, Nicaragua, Pakistan, 2001 Launch of phase 2 of the Global Campaign Against Epilepsy Singapore and the United Arab Emirates join the ILAE in Geneva 2005 Epilepsy Atlas published under the auspices of the Global 2001 Albania, Armenia, Arzerbaijan, Estonia, Honduras, Jamaica, Campaign Against Epilepsy Kyrgyzstan, Iraq, Lebanon, Malta, Malaysia, Nepal , Paraguay, Philippines, Qatar, Senegal, Syria, South Korea and Zimbabwe 2006 1st regional vice–president is elected – from the Asian and join the ILAE, making a total of 81 chapters Oceanian Region -

Managing Complex Systems 9-13 June 2014
Managing Complex Systems 9-13 June 2014 CONFERENCE COMMITTEE Founding Chair Publications Chair Mo Jamshidi – University of Texas, USA Tim Ferris – University of South Australia, Australia Conference General Co-Chairs Military Liaison Stephen Cook – University of South Australia, Australia Anne-Marie Grisogono - DSTO Vernon Ireland – University of Adelaide, Australia Asia & Pacific Liaisons Program Co-Chairs Saeid Nahavandi – Deakin University, Australia Quoc Do – Frazer Nash, Australia Bob Cavana – Victoria University, NZ Alex Gorod – University of Adelaide, Australia Fei- Yue Wang – Chinese Academy of Sciences, China Ramakrishnan Raman – Honeywell, India Tutorial and Organised Sessions Chair: Yeo Tat Soon, National University of Singapore, Singapore Matthew Joordens – Deakin University, Australia Tim Ferris – University of South Australia, Australia Europe Liaison Michael Henshaw – Loughborough University, UK Special Sessions Chair Roberto Sacile – University of Genova, Italy Saeid Nahavandi – Deakin University, Australia Abdelmadjid Bouabdallah, Technical University of Compiegne, France Mikhail Belov – IBS, Russia Local Arrangements Chair Daniel Drob – Ecole Polytechnique, France Jaci Pratt – DSTO, Australia US Liaison Alex Gorod – University of Adelaide, Australia Industrial Liaisons Mo Jamshidi – University of Texas San Antonio, USA Garry Roedler – Lockheed Martin Corp, USA Paul Rad – Rackspace Open Cloud Company, USA IT Chair Saeid Nahavandi – Deakin University, Australia William Scott – University of South Australia, Australia See -
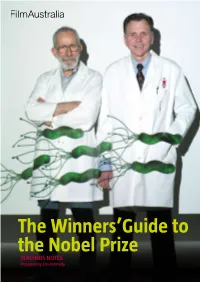
The Winners'guide to the Nobel Prize
The Winners’Guide to the Nobel Prize TEACHERS NOTES Prepared by Cris Kennedy THE WINNERS’ GUIDE TO THE NOBEL PRIZE TEACHERS Notes PAGE 1 Synopsis What does it take to win a Nobel Prize? Guts? Brilliance? Eccentricity? This film travels behind the scenes of the world’s most prestigious prize and into the minds of two of the people who have reached this pinnacle of excellence. In the most isolated capital city in the world, Perth, Western Australia, two scientists are interrupted while enjoying their fish and chips lunch by a phone call from Stockholm, Sweden. They have just been informed that they have been awarded the 2005 Nobel Prize for Medicine and could they make it to the awards ceremony? Australian scientists Barry Marshall and Robin Warren journey to the prize-winners’ podium is more than just a trip to the opposite side of the world to sub-zero temperatures, cultural pomp and extreme Swedish scheduling—it has been a career of trial and error, endless research and Aussie-battler-style stubborn determination. Today, this odd couple of science travel the globe as heroes—ambassadors to the science world—but it was 23 years ago in a modest hospital laboratory in Perth, that Marshall and Warren discovered a bacterium that survived in the human stomach that they called Helicobacter pylori. They believed that this bacterium, not stress, caused gastritis and peptic stomach ulcers, much to the chagrin of the medical world, which at the time scorned them. After years of careful observation, luck and persistence, they finally had the breakthrough they needed, but not before Marshall infected himself, using his own body as a guinea pig to test their theory. -

Nobel Laureates with Their Contribution in Biomedical Engineering
NOBEL LAUREATES WITH THEIR CONTRIBUTION IN BIOMEDICAL ENGINEERING Nobel Prizes and Biomedical Engineering In the year 1901 Wilhelm Conrad Röntgen received Nobel Prize in recognition of the extraordinary services he has rendered by the discovery of the remarkable rays subsequently named after him. Röntgen is considered the father of diagnostic radiology, the medical specialty which uses imaging to diagnose disease. He was the first scientist to observe and record X-rays, first finding them on November 8, 1895. Radiography was the first medical imaging technology. He had been fiddling with a set of cathode ray instruments and was surprised to find a flickering image cast by his instruments separated from them by some W. C. Röntgenn distance. He knew that the image he saw was not being cast by the cathode rays (now known as beams of electrons) as they could not penetrate air for any significant distance. After some considerable investigation, he named the new rays "X" to indicate they were unknown. In the year 1903 Niels Ryberg Finsen received Nobel Prize in recognition of his contribution to the treatment of diseases, especially lupus vulgaris, with concentrated light radiation, whereby he has opened a new avenue for medical science. In beautiful but simple experiments Finsen demonstrated that the most refractive rays (he suggested as the “chemical rays”) from the sun or from an electric arc may have a stimulating effect on the tissues. If the irradiation is too strong, however, it may give rise to tissue damage, but this may to some extent be prevented by pigmentation of the skin as in the negro or in those much exposed to Niels Ryberg Finsen the sun. -
Nobel Laureates in Physiology Or Medicine
All Nobel Laureates in Physiology or Medicine 1901 Emil A. von Behring Germany ”for his work on serum therapy, especially its application against diphtheria, by which he has opened a new road in the domain of medical science and thereby placed in the hands of the physician a victorious weapon against illness and deaths” 1902 Sir Ronald Ross Great Britain ”for his work on malaria, by which he has shown how it enters the organism and thereby has laid the foundation for successful research on this disease and methods of combating it” 1903 Niels R. Finsen Denmark ”in recognition of his contribution to the treatment of diseases, especially lupus vulgaris, with concentrated light radiation, whereby he has opened a new avenue for medical science” 1904 Ivan P. Pavlov Russia ”in recognition of his work on the physiology of digestion, through which knowledge on vital aspects of the subject has been transformed and enlarged” 1905 Robert Koch Germany ”for his investigations and discoveries in relation to tuberculosis” 1906 Camillo Golgi Italy "in recognition of their work on the structure of the nervous system" Santiago Ramon y Cajal Spain 1907 Charles L. A. Laveran France "in recognition of his work on the role played by protozoa in causing diseases" 1908 Paul Ehrlich Germany "in recognition of their work on immunity" Elie Metchniko France 1909 Emil Theodor Kocher Switzerland "for his work on the physiology, pathology and surgery of the thyroid gland" 1910 Albrecht Kossel Germany "in recognition of the contributions to our knowledge of cell chemistry made through his work on proteins, including the nucleic substances" 1911 Allvar Gullstrand Sweden "for his work on the dioptrics of the eye" 1912 Alexis Carrel France "in recognition of his work on vascular suture and the transplantation of blood vessels and organs" 1913 Charles R. -

SWOSU Biology Seniors Showcasing Works on April 22-24
SWOSU Biology Seniors Showcasing Works on April 22-24 04.19.2013 Biology majors in the senior seminar course at Southwestern Oklahoma State University will present posters April 22-24 on the Weatherford campus. The theme of this semester’s posters is “Celebrating 2000-2012 Nobel Laureates in Physiology or Medicine.” The presentations will be held on the second floor of the Old Science Building. Posters will be available for viewing from 9 a.m. through 5 p.m. each day. Student authors will be available from 4-5 p.m. on Monday, April 22. The public is invited and encouraged to attend. Poster topics and presenters are: • 2012, Sir John B. Gurdon, Shinya Yamanaka Nobel Laureates"for the discovery that mature cells can be reprogrammed to become pluripotent" by Melissa Peters, Geary. • 2011, Bruce A. Beutler, Jules A. Hoffmann, Ralph M. Steinman Nobel Laureates "for their discoveries concerning the activation of innate immunity" and the other half to Ralph M. Steinman "for his discovery of the dendritic cell and its role in adaptive immunity" by Maria Ortega, Guymon. • 2010, Robert G. Edwards Nobel Laureate"for the development of in vitro fertilization" by Shannah Rider, Mustang. • 2009, Elizabeth H. Blackburn, Carol W. Greider, Jack W. SzostakNobel Laureates "for the discovery of how chromosomes are protected by telomeres and the enzyme telomerase" by Kimberly Madrid, Lovington (NM). • 2008, HaraldzurHausen, Françoise Barré-Sinoussi, Luc MontagnierNobel Laureates "for his discovery of human papilloma viruses causing cervical cancer", the other half jointly to Françoise Barré-Sinoussi and Luc Montagnier"for their discovery of human immunodeficiency virus"by Kasey McFalls, Okmulgee. -

Nobel Prizes in Physiology & Medicine
Dr. John Andraos, http://www.careerchem.com/NAMED/NobelMed.pdf 1 Nobel Prizes in Physiology & Medicine © Dr. John Andraos, 2002 - 2020 Department of Chemistry, York University 4700 Keele Street, Toronto, ONTARIO M3J 1P3, CANADA For suggestions, corrections, additional information, and comments please send e-mails to [email protected] http://www.chem.yorku.ca/NAMED/ NOBEL PRIZE PHYSIOLOGY AND MEDICINE YEARNAMES OF SCIENTISTS NATIONALITY TYPE OF PHYSIOLOGY/MEDICINE 1901 Behring, Emil Adolf von German disease treatment (diphtheria) 1902 Ross, Sir Ronald British (b. Almara, India) disease treatment (malaria) 1903 Finsen, Niels Ryberg Danish disease treatment (lupus vulgaris) 1904 Pavlov, Ivan Petrovich Russian digestion 1905 Koch, Robert German disease treatment (TB) 1906 Golgi, Camillo Italian nervous system 1906 Cajal, Santiago Ramon y Spanish nervous system 1907 Laveran, Charles Louis Alphonse French disease treatment (protozoa) 1908 Mechnikov, Ilya Ilyich Russian immunity 1908 Ehrlich, Paul German immunity 1909 Kocher, Emil Theodor Swiss metabolism (thyroid gland) 1910 Kossel, Albrecht German proteins/nucleic acids 1911 Gullstrand, Allvar Swedish visual system 1912 Carrel, Alexis French-American blood vessels 1913 Richet, Charles Robert French anaphylaxis 1914 Barany, Robert Austrian vestibular apparatus 1915 no prize awarded N/A N/A 1916 no prize awarded N/A N/A 1917 no prize awarded N/A N/A 1918 no prize awarded N/A N/A 1919 Bordet, Jules Belgian immunity Dr. John Andraos, http://www.careerchem.com/NAMED/NobelMed.pdf 2 1920 Krogh, -

Fifty Years of Neuropsychopharmacology
Z. Lacković Fifty years of neuropsychopharmacology FIFTY YEARS OF NEUROPSYCHOPHARMACOLOGY Zdravko Lacković Laboratory of Molecular Neuropsihopharmacology, Department of Pharmacology & Croatian Brain Research Institute, University of Zagreb School of Medicine In the fi fty years since the fi rst Pula congress a lot of methodology of reverse pharmacology – instead has changed in neuropsychopharmacology. Granted, of a classic approach, nowadays receptors are more the major groups of psychoactive drugs had already and more often synthesized from the human genome been discovered: neuroleptics, antidepressants, ben- followed by search for their endogenous ligands and zodiazepine anxiolitics, psychostimulants... Neu- possibilities of their pharmacological manipulation. rology was using the basic antiepileptics while, for Th rough this, we now have orexines (hypocretins) example, the treatments for vascular and immuno- as key neurotransmitters of wakefulness. By reverse logical diseases were more expectative. At the time pharmacology we have discovered such receptors as of the fi rst Pula congress in 1960 we had only just the new opioid receptor ORL1 and its endogenous discovered that myasthenia gravis is an autoimmune ligand, nociceptin and fi nally, after several decades disease. It is also the year when dopamine defi ciency of diff erent assumptions, the prolactin-stimulating in the brain of Parkinsonian patients was discovered, a factor. What is especially intriguing and motivating fi nding which was to revolutionize understanding and is the fact that there are still hundreds of G-protein treatment of this disease. Th e last fi fty years have also receptors, nuclear receptors and synaptic receptors seen a proliferation of approaches to therapy and the waiting for researchers to discover their function and success of these medical fi elds has grown considerably. -

Immunology & Medic Al Microbiology
MINIREVIEW Helicobacter equorum: prevalence and signi¢cance for horses and humans Hilde Moyaert1, Frank Pasmans2, Annemie Decostere2, Richard Ducatelle2 & Freddy Haesebrouck2 1International Clinical Development, s.a. Alcon-Couvreur n.v., Puurs, Belgium; and 2Department of Pathology, Bacteriology and Avian Diseases, Faculty of Veterinary Medicine, Ghent University, Merelbeke, Belgium Downloaded from https://academic.oup.com/femspd/article/57/1/14/481915 by guest on 24 September 2021 Correspondence: Hilde Moyaert, Abstract International Clinical Development, s.a. Alcon-Couvreur n.v., Rijksweg 14, B-2870 Helicobacter equorum colonizes the caecum, colon and rectum of horses. The agent Puurs, Belgium. Tel.: 132 3 890 2146; is highly prevalent in o 6-month-old foals. In adult horses, the prevalence of H. fax: 132 3 890 2815; e-mail: hilde. equorum seems to be rather low, but these animals may harbour low, subdetectable [email protected] numbers of this microorganism in their intestines. So far, no association could be made between the presence of H. equorum and clinical disease or intestinal lesions Received 5 October 2008; accepted 6 July in adult horses. Further research is necessary to elucidate the pathogenic potential 2009. of this bacterial species towards young foals. Helicobacter equorum DNA was not Final version published online 14 August 2009. detected in human faeces, indicating that this microorganism does not commonly spread from horses towards humans. DOI:10.1111/j.1574-695X.2009.00583.x Editor: Willem van Leeuwen Keywords Helicobacter equorum; horses; humans. rRNA gene was developed. This tool was used to determine Introduction the presence of H. equorum in different horse populations Barry Marshall and Robin Warren, two Australian researchers (Moyaert et al., 2007c, 2009). -

List of Nobel Laureates 1
List of Nobel laureates 1 List of Nobel laureates The Nobel Prizes (Swedish: Nobelpriset, Norwegian: Nobelprisen) are awarded annually by the Royal Swedish Academy of Sciences, the Swedish Academy, the Karolinska Institute, and the Norwegian Nobel Committee to individuals and organizations who make outstanding contributions in the fields of chemistry, physics, literature, peace, and physiology or medicine.[1] They were established by the 1895 will of Alfred Nobel, which dictates that the awards should be administered by the Nobel Foundation. Another prize, the Nobel Memorial Prize in Economic Sciences, was established in 1968 by the Sveriges Riksbank, the central bank of Sweden, for contributors to the field of economics.[2] Each prize is awarded by a separate committee; the Royal Swedish Academy of Sciences awards the Prizes in Physics, Chemistry, and Economics, the Karolinska Institute awards the Prize in Physiology or Medicine, and the Norwegian Nobel Committee awards the Prize in Peace.[3] Each recipient receives a medal, a diploma and a monetary award that has varied throughout the years.[2] In 1901, the recipients of the first Nobel Prizes were given 150,782 SEK, which is equal to 7,731,004 SEK in December 2007. In 2008, the winners were awarded a prize amount of 10,000,000 SEK.[4] The awards are presented in Stockholm in an annual ceremony on December 10, the anniversary of Nobel's death.[5] As of 2011, 826 individuals and 20 organizations have been awarded a Nobel Prize, including 69 winners of the Nobel Memorial Prize in Economic Sciences.[6] Four Nobel laureates were not permitted by their governments to accept the Nobel Prize.