Evaluation & Management Revisions for 2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -

Practical Cardiac Auscultation
LWW/CCNQ LWWJ306-08 March 7, 2007 23:32 Char Count= Crit Care Nurs Q Vol. 30, No. 2, pp. 166–180 Copyright c 2007 Wolters Kluwer Health | Lippincott Williams & Wilkins Practical Cardiac Auscultation Daniel M. Shindler, MD, FACC This article focuses on the practical use of the stethoscope. The art of the cardiac physical exam- ination includes skillful auscultation. The article provides the author’s personal approach to the patient for the purpose of best hearing, recognizing, and interpreting heart sounds and murmurs. It should be used as a brief introduction to the art of auscultation. This article also attempts to illustrate heart sounds and murmurs by using words and letters to phonate the sounds, and by presenting practical clinical examples where auscultation clearly influences cardiac diagnosis and treatment. The clinical sections attempt to go beyond what is available in standard textbooks by providing information and stethoscope techniques that are valuable and useful at the bedside. Key words: auscultation, murmur, stethoscope HIS article focuses on the practical use mastered at the bedside. This article also at- T of the stethoscope. The art of the cardiac tempts to illustrate heart sounds and mur- physical examination includes skillful auscul- murs by using words and letters to phonate tation. Even in an era of advanced easily avail- the sounds, and by presenting practical clin- able technological bedside diagnostic tech- ical examples where auscultation clearly in- niques such as echocardiography, there is still fluences cardiac diagnosis and treatment. We an important role for the hands-on approach begin by discussing proper stethoscope selec- to the patient for the purpose of evaluat- tion and use. -

Mosby: Mosby's Nursing Video Skills
Mosby: Mosby's Nursing Video Skills Procedural Guideline for Assessing Apical Pulse Procedure Steps 1. Verify the health care provider’s orders. 2. Gather the necessary equipment and supplies. 3. Perform hand hygiene. 4. Provide for the patient’s privacy. 5. Introduce yourself to the patient and family if present. 6. Identify the patient using two identifiers. 7. Assess for factors that can affect the apical pulse rate and rhythm, such as medical history, disease processes, age, exercise, position changes, medications, temperature, or sympathetic stimulation. 8. Gloves are only worn if nurse will be in contact with bodily fluids or the patient is in protective precautions. 9. Help the patient into a supine or sitting position, and expose the sternum and the left side of the chest. 10. Locate the point of maximal impulse (PMI, or apical impulse). To do this, find the angle of Louis, which feels like a bony prominence just below the suprasternal notch. 11. Slide your fingers down each side of the angle to find the second intercostal space (ICS). Carefully move your fingers down the left side of the sternum to the fifth intercostal space and over to the left midclavicular line. 12. Feel the PMI as a light tap about 1 to 2 centimeters in diameter, reflecting the apex of the heart. 13. If the PMI is not where you would expect, as in a patient whose left ventricle is enlarged, inch your fingers along the fifth intercostal space until you feel the PMI. 14. Remember where you felt the PMI: over the apex of the heart in the fifth intercostal space at the left midclavicular line. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Review of Systems – Return Visit Have You Had Any Problems Related to the Following Symptoms in the Past Month? Circle Yes Or No
REVIEW OF SYSTEMS – RETURN VISIT HAVE YOU HAD ANY PROBLEMS RELATED TO THE FOLLOWING SYMPTOMS IN THE PAST MONTH? CIRCLE YES OR NO Today’s Date: ______________ Name: _______________________________ Date of Birth: __________________ GENERAL GENITOURINARY Fatigue Y N Blood in Urine Y N Fever / Chills Y N Menstrual Irregularity Y N Night Sweats Y N Painful Menstrual Cycle Y N Weight Gain Y N Vaginal Discharge Y N Weight Loss Y N Vaginal Dryness Y N EYES Vaginal Itching Y N Vision Changes Y N Painful Sex Y N EAR, NOSE, & THROAT SKIN Hearing Loss Y N Hair Loss Y N Runny Nose Y N New Skin Lesions Y N Ringing in Ears Y N Rash Y N Sinus Problem Y N Pigmentation Change Y N Sore Throat Y N NEUROLOGIC BREAST Headache Y N Breast Lump Y N Muscular Weakness Y N Tenderness Y N Tingling or Numbness Y N Nipple Discharge Y N Memory Difficulties Y N CARDIOVASCULAR MUSCULOSKELETAL Chest Pain Y N Back Pain Y N Swelling in Legs Y N Limitation of Motion Y N Palpitations Y N Joint Pain Y N Fainting Y N Muscle Pain Y N Irregular Heart Beat Y N ENDOCRINE RESPIRATORY Cold Intolerance Y N Cough Y N Heat Intolerance Y N Shortness of Breath Y N Excessive Thirst Y N Post Nasal Drip Y N Excessive Amount of Urine Y N Wheezing Y N PSYCHOLOGY GASTROINTESTINAL Difficulty Sleeping Y N Abdominal Pain Y N Depression Y N Constipation Y N Anxiety Y N Diarrhea Y N Suicidal Thoughts Y N Hemorrhoids Y N HEMATOLOGIC / LYMPHATIC Nausea Y N Easy Bruising Y N Vomiting Y N Easy Bleeding Y N GENITOURINARY Swollen Lymph Glands Y N Burning with Urination Y N ALLERGY / IMMUNOLOGY Urinary -

Bradycardia; Pulse Present
Bradycardia; Pulse Present History Signs and Symptoms Differential • Past medical history • HR < 60/min with hypotension, acute • Acute myocardial infarction • Medications altered mental status, chest pain, • Hypoxia / Hypothermia • Beta-Blockers acute CHF, seizures, syncope, or • Pacemaker failure • Calcium channel blockers shock secondary to bradycardia • Sinus bradycardia • Clonidine • Chest pain • Head injury (elevated ICP) or Stroke • Digoxin • Respiratory distress • Spinal cord lesion • Pacemaker • Hypotension or Shock • Sick sinus syndrome • Altered mental status • AV blocks (1°, 2°, or 3°) • Syncope • Overdose Heart Rate < 60 / min and Symptomatic: Exit to Hypotension, Acute AMS, Ischemic Chest Pain, Appropriate NO Acute CHF, Seizures, Syncope, or Shock Protocol(s) secondary to bradycardia Typically HR < 50 / min YES Airway Protocol(s) AR 1, 2, 3 if indicated Respiratory Distress Reversible Causes Protocol AR 4 if indicated Hypovolemia Hypoxia Chest Pain: Cardiac and STEMI Section Cardiac Protocol Adult Protocol AC 4 Hydrogen ion (acidosis) if indicated Hypothermia Hypo / Hyperkalemia Search for Reversible Causes B Tension pneumothorax 12 Lead ECG Procedure Tamponade; cardiac Toxins Suspected Beta- IV / IO Protocol UP 6 Thrombosis; pulmonary Blocker or Calcium P Cardiac Monitor (PE) Channel Blocker Thrombosis; coronary (MI) A Follow Overdose/ Toxic Ingestion Protocol TE 7 P If No Improvement Transcutaneous Pacing Procedure P (Consider earlier in 2nd or 3rd AVB) Notify Destination or Contact Medical Control Revised AC 2 01/01/2021 Any local EMS System changes to this document must follow the NC OEMS Protocol Change Policy and be approved by OEMS 1 Bradycardia; Pulse Present Adult Cardiac Adult Section Protocol Pearls • Recommended Exam: Mental Status, HEENT, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro • Identifying signs and symptoms of poor perfusion caused by bradycardia are paramount. -
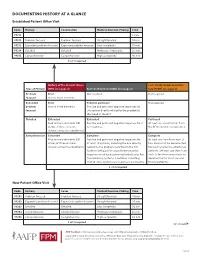
Documenting History at a Glance
DOCUMENTING HISTORY AT A GLANCE Established Patient Office Visit Code History Examination Medical Decision-Making Time 99211 — — — 5 min. 99212 Problem focused Problem focused Straightforward 10 min. 99213 Expanded problem focused Expanded problem focused Low complexity 15 min. 99214 Detailed Detailed Moderate complexity 25 min. 99215 Comprehensive Comprehensive High complexity 40 min. 2 of 3 required History of the Present Illness Past, Family and/or Social His- Type of History (HPI) (see page 2) Review of Systems (ROS) (see page 2) tory (PFSH) (see page 2) Problem Brief Not required Not required focused One to three elements Expanded Brief Problem pertinent Not required problem One to three elements Positive and pertinent negative responses for focused the system directly related to the problem(s) identified in the HPI. Detailed Extended Extended Pertinent Four or more elements (OR Positive and pertinent negative responses for 2 At least one specific item from status of three or more to 9 systems. the PFSH must be documented. chronic or inactive conditions) Comprehensive Extended Complete Complete Four or more elements (OR Positive and pertinent negative responses for At least one item from each of status of three or more at least 10 systems, including the one directly two areas must be documented chronic or inactive conditions) related to the problem identified in the HPI. for most services to established Systems with positive or pertinent negative patients. (At least one item from responses must be documented individually. For each of the three areas must be the remaining systems, a notation indicating documented for most services that all other systems are negative is permissible. -

Arrhythmia What Is It?
Arrhythmia What is it? Most of us have felt our heart race or skip a beat. It’s fairly normal every once and a while. But for some people, it’s a sign of arrhythmia – a disorder of your heart rate or rhythm – that needs to be checked out by a specialist. If you have an arrhythmia (there are multiple types), your heart either beats: • too fast • too slow or • with an irregular pattern Did You Know? This change in your heart rhythm is usually caused by a “glitch” Our heart beats an average of in your heart’s electrical activity, which tells the heart when to 70 to 80 times a minute and contract and pump blood to the body. Your heart doesn’t beat over 100,000 times a day! It’s with the regularity of a Swiss watch, and many factors can cause no wonder millions of people an irregularity. notice palpitations such as skipping a beat, fluttering or a Some of these factors include: racing heart. • having had a heart attack • having heart failure • blood chemistry imbalances • abnormal hormone levels • alcohol, caffeine and other substances or medicines • a variety of inherited abnormalities 8 Tips for Staying Heart Healthy with Arrhythmias Living with an arrhythmia varies tremendously from one person to the next. It will depend on the type of arrhythmia you have, how serious it is and the recommended treatment. Some people can take a single medication to correct their heart’s rhythm; others undergo electrophysiology studies or require a pacemaker or implantable defibrillator. No matter what kind of arrhythmia you have, there are things you can do to keep your heart healthy and ticking as it should. -

5 Precordial Pulsations
Chapter 5 / Precordial Pulsations 113 5 Precordial Pulsations CONTENTS MECHANICS AND PHYSIOLOGY OF THE NORMAL APICAL IMPULSE PHYSICAL PRINCIPLES GOVERNING THE FORMATION OF THE APICAL IMPULSE NORMAL APICAL IMPULSE AND ITS DETERMINANTS ASSESSMENT OF THE APICAL IMPULSE LEFT PARASTERNAL AND STERNAL MOVEMENTS RIGHT PARASTERNAL MOVEMENT PULSATIONS OVER THE CLAVICULAR HEADS PULSATIONS OVER THE SECOND AND/OR THIRD LEFT INTERCOSTAL SPACES SUBXIPHOID IMPULSE PRACTICAL POINTS IN THE CLINICAL ASSESSMENT OF PRECORDIAL PULSATIONS REFERENCES In this chapter the pulsations of the precordium will be discussed in relation to their identification, the mechanisms of their origin, and their pathophysiological and clinical significance. Precordial pulsations include the “apical impulse,” left parasternal movement, right parasternal movement, pulsations of the clavicular heads, pulsations over the second left intercostal space, and subxiphoid impulses. MECHANICS AND PHYSIOLOGY OF THE NORMAL APICAL IMPULSE Since during systole the heart contracts, becoming smaller and therefore moving away from the chest wall, why should one feel a systolic outward movement (the apical impulse) at all? Logically speaking there should not be an apical impulse. Several different methods of recording the precordial motion have been used to study the apical impulse going back to the late 19th century (1,2). Among the more modern methods, the notable ones are the recordings of the apexcardiogram (3–17), the impulse cardiogram (18), and the kinetocardiogram (19–21). While apexcardiography records the relative displacement of the chest wall under the transducer pickup device, which is often held by the examiner’s hands, the proponents of the impulse cardiography and kinetocardiography point out that these methods allow the recording of the absolute movement of the chest wall because the pickup device is anchored to a fixed point held 113 114 Cardiac Physical Examination in space away from the chest. -

Jugular Venous Pressure
NURSING Jugular Venous Pressure: Measuring PRACTICE & SKILL What is Measuring Jugular Venous Pressure? Measuring jugular venous pressure (JVP) is a noninvasive physical examination technique used to indirectly measure central venous pressure(i.e., the pressure of the blood in the superior and inferior vena cava close to the right atrium). It is a part of a complete cardiovascular assessment. (For more information on cardiovascular assessment in adults, see Nursing Practice & Skill ... Physical Assessment: Performing a Cardiovascular Assessment in Adults ) › What: Measuring JVP is a screening mechanism to identify abnormalities in venous return, blood volume, and right heart hemodynamics › How: JVP is determined by measuring the vertical distance between the sternal angle and the highest point of the visible venous pulsation in the internal jugular vein orthe height of the column of blood in the external jugular vein › Where: JVP can be measured in inpatient, outpatient, and residential settings › Who: Nurses, nurse practitioners, physician assistants, and treating clinicians can measure JVP as part of a complete cardiovascular assessment What is the Desired Outcome of Measuring Jugular Venous Pressure? › The desired outcome of measuring JVP is to establish the patient’s JVP within the normal range or for abnormal JVP to be identified so that appropriate treatment may be initiated. Patients’ level of activity should not be affected by having had the JVP measured ICD-9 Why is Measuring Jugular Venous Pressure Important? 89.62 › The JVP is -

Sleep Medicine Curriculum for Neurology Residents
Sleep Medicine Curriculum for Neurology Residents This curriculum, developed in collaboration with the AAN Consortium of Neurology Program Directors and Graduate Education Subcommittee, provides a comprehensive outline of the relevant educational goals for the future generation of adult neurologists learning sleep medicine during residency. The clinical scope of this curriculum is common and uncommon sleep disorders encountered in typical neurology practices. While the all-encompassing scope of this outline covers more than is expected to be learned by neurology residents on a given subspecialty rotation, the measurable objectives are included to provide program directors and other rotation developers the means of evaluating whether a minimum competence in sleep was attained in any combination of specific areas. Finally, as sleep medicine is a cross-disciplinary neurologic subspecialty, the curriculum ends with a table highlighting overlapping conditions between major sleep disorder categories and neurologic subspecialities. Authors: Lead Author Logan Schneider, MD [email protected] Stanford/VA Alzheimer’s Center Alon Avidan, MD, MPH, FAAN David Geffen School of Medicine at UCLA Muna Irfan, MD University of Minnesota Meena Khan, MD The Ohio State University Created: January 2020 Effective: February 2020 to February 2021 Approved by the American Academy of Neurology’s Graduate Education Subcommittee Sleep Medicine Curriculum for Neurology Residents Part I. General Clinical Approach Clinical evaluation: History Efficiently obtains a complete, relevant, and organized neurologic history Performs comprehensive review of systems pertinent to ICSD-3 sleep-wake disorder categories (sleep-related disordered breathing, hypersomnias, insomnias, parasomnias, sleep-related movement disorders, circadian disorders) Performs comprehensive review of systems probing medical conditions that are known to impact sleep-wake disorders (e.g. -

Review of Systems Health History Sheet Patient: ______DOB: ______Age: ______Gender: M / F
603 28 1/4 Road Grand Junction, CO 81506 (970) 263-2600 Review of Systems Health History Sheet Patient: _________________ DOB: ____________ Age: ______ Gender: M / F Please mark any symptoms you are experiencing that are related to your complaint today: Allergic/ Immunologic Ears/Nose/Mouth/Throat Genitourinary Men Only Frequent Sneezing Bleeding Gums Pain with Urinating Pain/Lump in Testicle Hives Difficulty Hearing Blood in Urine Penile Itching, Itching Dizziness Difficulty Urinating Burning or Discharge Runny Nose Dry Mouth Incomplete Emptying Problems Stopping or Sinus Pressure Ear Pain Urinary Frequency Starting Urine Stream Cardiovascular Frequent Infections Loss of Urinary Control Waking to Urinate at Chest Pressure/Pain Frequent Nosebleeds Hematologic / Lymphatic Night Chest Pain on Exertion Hoarseness Easy Bruising / Bleeding Sexual Problems / Irregular Heart Beats Mouth Breathing Swollen Glands Concerns Lightheaded Mouth Ulcers Integumentary (Skin) History of Sexually Swelling (Edema) Nose/Sinus Problems Changes in Moles Transmitted Diseases Shortness of Breath Ringing in Ears Dry Skin Women Only When Lying Down Endocrine Eczema Bleeding Between Shortness of Breath Increased Thirst / Growth / Lesions Periods When Walking Urination Itching Heavy Periods Constitutional Heat/Cold Intolerance Jaundice (Yellow Extreme Menstrual Pain Exercise Intolerance Gastrointestinal Skin or Eyes) Vaginal Itching, Fatigue Abdominal Pain Rash Burning or Discharge Fever Black / Tarry Stool Respiratory Waking to Urinate at Weight Gain (___lbs) Blood