University of Minnesota
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

International Journal of Medical and Health Sciences
International Journal of Medical and Health Sciences Journal Home Page: http://www.ijmhs.net ISSN:2277-4505 Review article Examining the liver – Revisiting an old friend Cyriac Abby Philips1*, Apurva Pande2 1Department of Hepatology and Transplant Medicine, PVS Institute of Digestive Diseases, PVS Memorial Hospital, Kaloor, Kochi, Kerala, India, 2Department of Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India. ABSTRACT In the current era of medical practice, super saturated with investigations of choice and development of diagnostic tools, clinical examination is a lost art. In this review we briefly discuss important aspects of examination of the liver, which is much needed in decision making on investigational approach. We urge the new medical student or the newly practicing physician to develop skills in clinical examination for resourceful management of the patient. KEYWORDS: Liver, examination, clinical skills, hepatomegaly, chronic liver disease, portal hypertension, liver span INTRODUCTION respiration, the excursion of liver movement is around 2 to 3 The liver attains its adult size by the age of 15 years. The cm. Castell and Frank has elegantly described normal liver liver weighs 1.2 to 1.4 kg in women and 1.4 to 1.5 kg in span in men and women utilizing the percussion method men. The liver seldom extends more than 5 cm beyond the (Table 1). Accordingly, the mean liver span is 10.5 cm for midline towards the left costal margin. During inspiration, men and 7 cm in women. During examination, a span 2 to 3 the diaphragmatic exertion moves the liver downward with cm larger or smaller than these values is considered anterior surface rotating to the right. -

The Stethoscope: Some Preliminary Investigations
695 ORIGINAL ARTICLE The stethoscope: some preliminary investigations P D Welsby, G Parry, D Smith Postgrad Med J: first published as on 5 January 2004. Downloaded from ............................................................................................................................... See end of article for Postgrad Med J 2003;79:695–698 authors’ affiliations ....................... Correspondence to: Dr Philip D Welsby, Western General Hospital, Edinburgh EH4 2XU, UK; [email protected] Submitted 21 April 2003 Textbooks, clinicians, and medical teachers differ as to whether the stethoscope bell or diaphragm should Accepted 30 June 2003 be used for auscultating respiratory sounds at the chest wall. Logic and our results suggest that stethoscope ....................... diaphragms are more appropriate. HISTORICAL ASPECTS note is increased as the amplitude of the sound rises, Hippocrates advised ‘‘immediate auscultation’’ (the applica- resulting in masking of higher frequency components by tion of the ear to the patient’s chest) to hear ‘‘transmitted lower frequencies—‘‘turning up the volume accentuates the sounds from within’’. However, in 1816 a French doctor, base’’ as anyone with teenage children will have noted. Rene´The´ophile Hyacinth Laennec invented the stethoscope,1 Breath sounds are generated by turbulent air flow in the which thereafter became the identity symbol of the physician. trachea and proximal bronchi. Airflow in the small airways Laennec apparently had observed two children sending and alveoli is of lower velocity and laminar in type and is 6 signals to each other by scraping one end of a long piece of therefore silent. What is heard at the chest wall depends on solid wood with a pin, and listening with an ear pressed to the conductive and filtering effect of lung tissue and the the other end.2 Later, in 1816, Laennec was called to a young characteristics of the chest wall. -
General Physical Examination Skills for Ahps
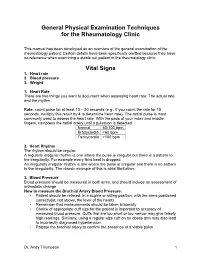
General Physical Examination Techniques for the Rheumatology Clinic This manual has been developed as an overview of the general examination of the rheumatology patient. Certain details have been specifically omitted because they have no relevance when examining a stable out patient in the rheumatology clinic. Vital Signs 1. Heart rate 2. Blood pressure 3. Weight 1. Heart Rate There are two things you want to document when assessing heart rate: The actual rate and the rhythm. Rate: count pulse for at least 15 – 30 seconds (e.g., if you count the rate for 15 seconds, multiply this result by 4 to determine heart rate). The radial pulse is most commonly used to assess the heart rate. With the pads of your index and middle fingers, compress the radial artery until a pulsation is detected. Normal 60-100 bpm Bradycardia <60 bpm Tachycardia >100 bpm 2. Heart Rhythm The rhythm should be regular. A regularly irregular rhythm is one where the pulse is irregular but there is a pattern to the irregularity. For example every third beat is dropped. An irregularly irregular rhythm is one where the pulse is irregular and there is no pattern to the irregularity. The classic example of this is atrial fibrillation. 3. Blood Pressure Blood pressure should be measured in both arms, and should include an assessment of orthostatic change How to measure the Brachial Artery Blood Pressure: • Patient should be relaxed, in a supine or sitting position, with the arms positioned correctly(at, not above, the level of the heart) • Remember that measurements should be taken bilaterally • Choice of appropriate cuff size for the patient is important to accuracy of measured blood pressure. -

Myocardial Hamartoma As a Cause of VF Cardiac Arrest in an Infant a Frampton, L Gray, S Bell
590 CASE REPORTS Emerg Med J: first published as 10.1136/emj.2003.009951 on 26 July 2005. Downloaded from Myocardial hamartoma as a cause of VF cardiac arrest in an infant A Frampton, L Gray, S Bell ............................................................................................................................... Emerg Med J 2005;22:590–591. doi: 10.1136/emj.2003.009951 ardiac arrests in children are fortunately rare and the patients. However a review by Young et al2 found that the presenting cardiac rhythm is often asystole. However, survival to hospital discharge in infants and children Cventricular fibrillation (VF) can occur and may respond presenting with VF/VT was of the order of 30%, compared favourably to defibrillation. with only 5% of patients whose initial presenting rhythm was asystole. VF has also been demonstrated to be relatively more CASE REPORT common in infants than any other paediatric age group A 7 month old girl was sitting in her high chair when she was (p,0.006).1 One study of over 500 000 children presenting to witnessed by her parents to collapse suddenly at 1707 hours. an ED over a period of 5 years found VF to be the third most They attempted cardiopulmonary resuscitation (CPR) and the common presenting cardiac arrhythmia of any origin in ambulance crew arrived 7 minutes later, the cardiac monitor infants below the age of 1 year.1 It has been suggested that a displaying VF. No defibrillation or medications were admi- subgroup of patients (those ,1 year old) that would benefit nistered and she was rapidly transferred to her nearest from early defibrillation can be identified.2 emergency department (ED), arriving at 1723. -

New Patient Medical History Form
NEW PATIENT MEDICAL HISTORY FORM Full Name: Date: Birth Date: Age: ALLERGIES o NO ALLERGIES ALLERGY ALLERGIC REACTION MEDICATIONS MEDICATIONS DOSE TIMES PER DAY (Please list ALL) (Mg., pill, etc.) If you need more room to list medications, please write them on a blank sheet of paper with the required information HEALTH MAINTENANCE SCREENING TEST HISTORY CHolesterol Date: Facility/Provider: Abnormal Result? Y N Colonoscopy/SIGMOID Date: Facility/Provider: Abnormal Result? Y N Mammogram Date: Facility/Provider: Abnormal Result? Y N PAP SMEAR Date: Facility/Provider: Abnormal Result? Y N BONE density Date: Facility/Provider: Abnormal Result? Y N VACCINATION HISTORY Last Tetanus Booster or TdaP: Last Pnuemovax (Pneumonia): Last Flu Vaccine: Last Prevnar: Last Zoster Vaccine (Shingles): PERSONAL MEDICAL HISTORY DISEASE/CONDITION CURRENT PAST COMMENTS Alcoholism/Drug Abuse Asthma Cancer (type:_________________________________) Depression/Anxiety/Bipolar/Suicidal Diabetes (type:_______________________________) Emphysema (COPD) Heart Disease High Blood Pressure (hypertension) High Cholesterol Hypothyroidism/Thyroid Disease Renal (kidney) Disease Migraine Headaches Stroke Other: Other: SURGERIES TYPE (specify left/right) Date Location/Facility WOMEN’S HEALTH HISTORY Date of Last Menstrual Cycle: Age of First Menstruation: _____ Age of Menopause: _____ Total Number of Pregnancies: Number of Live Births: Pregnancy Complications: Patient Name: DOB: family MEDICAL HISTORY o NO Significant Family History IS KNOWN 4 CHECK ALL THat apply Stroke Cancer -

Approach to Cyanosis in a Neonate.Pdf
PedsCases Podcast Scripts This podcast can be accessed at www.pedscases.com, Apple Podcasting, Spotify, or your favourite podcasting app. Approach to Cyanosis in a Neonate Developed by Michelle Fric and Dr. Georgeta Apostol for PedsCases.com. June 29, 2020 Introduction Hello, and welcome to this pedscases podcast on an approach to cyanosis in a neonate. My name is Michelle Fric and I am a fourth-year medical student at the University of Alberta. This podcast was made in collaboration with Dr. Georgeta Apostol, a general pediatrician at the Royal Alexandra Hospital Pediatrics Clinic in Edmonton, Alberta. Cyanosis refers to a bluish discoloration of the skin or mucous membranes and is a common finding in newborns. It is a clinical manifestation of the desaturation of arterial or capillary blood and may indicate serious hemodynamic instability. It is important to have an approach to cyanosis, as it can be your only sign of a life-threatening illness. The goal of this podcast is to develop this approach to a cyanotic newborn with a focus on these can’t miss diagnoses. After listening to this podcast, the learner should be able to: 1. Define cyanosis 2. Assess and recognize a cyanotic infant 3. Develop a differential diagnosis 4. Identify immediate investigations and management for a cyanotic infant Background Cyanosis can be further broken down into peripheral and central cyanosis. It is important to distinguish these as it can help you to formulate a differential diagnosis and identify cases that are life-threatening. Peripheral cyanosis affects the distal extremities resulting in blue color of the hands and feet, while the rest of the body remains pinkish and well perfused. -

Advanced Interpretation of Adult Vital Signs in Trauma William D
Advanced Interpretation of Adult Vital Signs in Trauma William D. Hampton, DO Emergency Physician 26 March 2015 Learning Objectives 1. Better understand vital signs for what they can tell you (and what they can’t) in the assessment of a trauma patient. 2. Appreciate best practices in obtaining accurate vital signs in trauma patients. 3. Learn what teaching about vital signs is evidence-based and what is not. 4. Explain the importance of vital signs to more accurately triage, diagnose, and confidently disposition our trauma patients. 5. Apply the monitoring (and manipulation of) vital signs to better resuscitate trauma patients. Disclosure Statement • Faculty/Presenters/Authors/Content Reviewers/Planners disclose no conflict of interest relative to this educational activity. Successful Completion • To successfully complete this course, participants must attend the entire event and complete/submit the evaluation at the end of the session. • Society of Trauma Nurses is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. Vital Signs Vital Signs Philosophy: “View vital signs as compensatory to the illness/complaint as opposed to primary.” Crowe, Donald MD. “Vital Sign Rant.” EMRAP: Emergency Medicine Reviews and Perspectives. February, 2010. Vital Signs Truth over Accuracy: • Document the true status of the patient: sick or not? • Complete vital signs on every patient, every time, regardless of the chief complaint. • If vital signs seem misleading or inaccurate, repeat them! • Beware sending a patient home with abnormal vitals (especially tachycardia)! •Treat vital signs the same as any other diagnostics— review them carefully prior to disposition. The Mother’s Vital Sign: Temperature Case #1 - 76-y/o homeless ♂ CC: 76-y/o homeless ♂ brought to the ED by police for eval. -

Central Venous Pressure Venous Examination but Underestimates Ultrasound Accurately Reflects the Jugular
Ultrasound Accurately Reflects the Jugular Venous Examination but Underestimates Central Venous Pressure Gur Raj Deol, Nicole Collett, Andrew Ashby and Gregory A. Schmidt Chest 2011;139;95-100; Prepublished online August 26, 2010; DOI 10.1378/chest.10-1301 The online version of this article, along with updated information and services can be found online on the World Wide Web at: http://chestjournal.chestpubs.org/content/139/1/95.full.html Chest is the official journal of the American College of Chest Physicians. It has been published monthly since 1935. Copyright2011by the American College of Chest Physicians, 3300 Dundee Road, Northbrook, IL 60062. All rights reserved. No part of this article or PDF may be reproduced or distributed without the prior written permission of the copyright holder. (http://chestjournal.chestpubs.org/site/misc/reprints.xhtml) ISSN:0012-3692 Downloaded from chestjournal.chestpubs.org at UCSF Library & CKM on January 21, 2011 © 2011 American College of Chest Physicians CHEST Original Research CRITICAL CARE Ultrasound Accurately Refl ects the Jugular Venous Examination but Underestimates Central Venous Pressure Gur Raj Deol , MD ; Nicole Collett , MD ; Andrew Ashby , MD ; and Gregory A. Schmidt , MD , FCCP Background: Bedside ultrasound examination could be used to assess jugular venous pressure (JVP), and thus central venous pressure (CVP), more reliably than clinical examination. Methods: The study was a prospective, blinded evaluation comparing physical examination of external jugular venous pressure (JVPEXT), internal jugular venous pressure (JVPINT), and ultrasound collapse pressure (UCP) with CVP measured using an indwelling catheter. We com- pared the examination of the external and internal JVP with each other and with the UCP and CVP. -

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -

Practical Cardiac Auscultation
LWW/CCNQ LWWJ306-08 March 7, 2007 23:32 Char Count= Crit Care Nurs Q Vol. 30, No. 2, pp. 166–180 Copyright c 2007 Wolters Kluwer Health | Lippincott Williams & Wilkins Practical Cardiac Auscultation Daniel M. Shindler, MD, FACC This article focuses on the practical use of the stethoscope. The art of the cardiac physical exam- ination includes skillful auscultation. The article provides the author’s personal approach to the patient for the purpose of best hearing, recognizing, and interpreting heart sounds and murmurs. It should be used as a brief introduction to the art of auscultation. This article also attempts to illustrate heart sounds and murmurs by using words and letters to phonate the sounds, and by presenting practical clinical examples where auscultation clearly influences cardiac diagnosis and treatment. The clinical sections attempt to go beyond what is available in standard textbooks by providing information and stethoscope techniques that are valuable and useful at the bedside. Key words: auscultation, murmur, stethoscope HIS article focuses on the practical use mastered at the bedside. This article also at- T of the stethoscope. The art of the cardiac tempts to illustrate heart sounds and mur- physical examination includes skillful auscul- murs by using words and letters to phonate tation. Even in an era of advanced easily avail- the sounds, and by presenting practical clin- able technological bedside diagnostic tech- ical examples where auscultation clearly in- niques such as echocardiography, there is still fluences cardiac diagnosis and treatment. We an important role for the hands-on approach begin by discussing proper stethoscope selec- to the patient for the purpose of evaluat- tion and use. -

Bates' Pocket Guide to Physical Examination and History Taking
Lynn S. Bickley, MD, FACP Clinical Professor of Internal Medicine School of Medicine University of New Mexico Albuquerque, New Mexico Peter G. Szilagyi, MD, MPH Professor of Pediatrics Chief, Division of General Pediatrics University of Rochester School of Medicine and Dentistry Rochester, New York Acquisitions Editor: Elizabeth Nieginski/Susan Rhyner Product Manager: Annette Ferran Editorial Assistant: Ashley Fischer Design Coordinator: Joan Wendt Art Director, Illustration: Brett MacNaughton Manufacturing Coordinator: Karin Duffield Indexer: Angie Allen Prepress Vendor: Aptara, Inc. 7th Edition Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2009 by Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2007, 2004, 2000 by Lippincott Williams & Wilkins. Copyright © 1995, 1991 by J. B. Lippincott Company. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appear- ing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at Two Commerce Square, 2001 Market Street, Philadelphia PA 19103, via email at [email protected] or via website at lww.com (products and services). 9 8 7 6 5 4 3 2 1 Printed in China Library of Congress Cataloging-in-Publication Data Bickley, Lynn S. Bates’ pocket guide to physical examination and history taking / Lynn S. -

(June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION and WHY
DRAFT EVALUATION & MANAGEMENT DOCUMENTATION GUIDELINES (June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION AND WHY IS IT IMPORTANT? Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history including past and present illnesses, examinations, tests, treatments, and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high quality care. The medical record facilitates: · the ability of the physician and other health care professionals to evaluate and plan the patient's immediate treatment, and to monitor his/her health care over time. · communication and continuity of care among physicians and other health care professionals involved in the patient's care; · accurate and timely claims review and payment; · appropriate utilization review and quality of care evaluations; and · collection of data that may be useful for research and education. An appropriately documented medical record can reduce many of the "hassles" associated with claims processing and may serve as a legal document to verify the care provided, if necessary. WHAT DO PAYERS WANT AND WHY? Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate: · the site of service; · the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or · that services provided have been accurately reported. II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION The principles of documentation listed below are applicable to all types of medical and surgical Pg. 1 services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status.