(June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION and WHY
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Advanced Interpretation of Adult Vital Signs in Trauma William D
Advanced Interpretation of Adult Vital Signs in Trauma William D. Hampton, DO Emergency Physician 26 March 2015 Learning Objectives 1. Better understand vital signs for what they can tell you (and what they can’t) in the assessment of a trauma patient. 2. Appreciate best practices in obtaining accurate vital signs in trauma patients. 3. Learn what teaching about vital signs is evidence-based and what is not. 4. Explain the importance of vital signs to more accurately triage, diagnose, and confidently disposition our trauma patients. 5. Apply the monitoring (and manipulation of) vital signs to better resuscitate trauma patients. Disclosure Statement • Faculty/Presenters/Authors/Content Reviewers/Planners disclose no conflict of interest relative to this educational activity. Successful Completion • To successfully complete this course, participants must attend the entire event and complete/submit the evaluation at the end of the session. • Society of Trauma Nurses is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. Vital Signs Vital Signs Philosophy: “View vital signs as compensatory to the illness/complaint as opposed to primary.” Crowe, Donald MD. “Vital Sign Rant.” EMRAP: Emergency Medicine Reviews and Perspectives. February, 2010. Vital Signs Truth over Accuracy: • Document the true status of the patient: sick or not? • Complete vital signs on every patient, every time, regardless of the chief complaint. • If vital signs seem misleading or inaccurate, repeat them! • Beware sending a patient home with abnormal vitals (especially tachycardia)! •Treat vital signs the same as any other diagnostics— review them carefully prior to disposition. The Mother’s Vital Sign: Temperature Case #1 - 76-y/o homeless ♂ CC: 76-y/o homeless ♂ brought to the ED by police for eval. -

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -

Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019
Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019 Centers for Medicare & Medicaid Services PRA Disclosure Statement According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is x. The time required to complete this information collection is estimated to average 0.3 minutes per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. This estimate does not include time for training. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850. *****CMS Disclaimer*****Please do not send applications, claims, payments, medical records or any documents containing sensitive information to the PRA Reports Clearance Office. Please note that any correspondence not pertaining to the information collection burden approved under the associated OMB control number listed on this form will not be reviewed, forwarded, or retained. If you have questions or concerns regarding where to submit your documents, please contact Joan Proctor National Coordinator, Home Health Quality Reporting Program Centers for Medicare & Medicaid. OASIS-D Guidance Manual Table of Contents Page -

GUIDELINES for WRITING SOAP NOTES and HISTORY and PHYSICALS
GUIDELINES FOR WRITING SOAP NOTES and HISTORY AND PHYSICALS by Lois E. Brenneman, M.S.N, C.S., A.N.P, F.N.P. © 2001 NPCEU Inc. all rights reserved NPCEU INC. PO Box 246 Glen Gardner, NJ 08826 908-537-9767 - FAX 908-537-6409 www.npceu.com Copyright © 2001 NPCEU Inc. All rights reserved No part of this book may be reproduced in any manner whatever, including information storage, or retrieval, in whole or in part (except for brief quotations in critical articles or reviews), without written permission of the publisher: NPCEU, Inc. PO Box 246, Glen Gardner, NJ 08826 908-527-9767, Fax 908-527-6409. Bulk Purchase Discounts. For discounts on orders of 20 copies or more, please fax the number above or write the address above. Please state if you are a non-profit organization and the number of copies you are interested in purchasing. 2 GUIDELINES FOR WRITING SOAP NOTES and HISTORY AND PHYSICALS Lois E. Brenneman, M.S.N., C.S., A.N.P., F.N.P. Written documentation for clinical management of patients within health care settings usually include one or more of the following components. - Problem Statement (Chief Complaint) - Subjective (History) - Objective (Physical Exam/Diagnostics) - Assessment (Diagnoses) - Plan (Orders) - Rationale (Clinical Decision Making) Expertise and quality in clinical write-ups is somewhat of an art-form which develops over time as the student/practitioner gains practice and professional experience. In general, students are encouraged to review patient charts, reading as many H/Ps, progress notes and consult reports, as possible. In so doing, one gains insight into a variety of writing styles and methods of conveying clinical information. -

Chief Complaint: "Swelling of Tongue and Difficulty Breathing and Swallowing"
Chief Complaint: "swelling of tongue and difficulty breathing and swallowing" History of Present Illness: 77 y o woman in NAD with a h/o CAD, DM2, asthma and HTN on altace for 8 years awoke from sleep around 2:30 am this morning of a sore throat and swelling of tongue. She came immediately to the ED b/c she was having difficulty swallowing and some trouble breathing due to obstruction caused by the swelling. She has never had a similar reaction ever before and she did not have any associated SOB, chest pain, itching, or nausea. She has not noticed any rashes, and has been afebrile. She says that she feels like it is swollen down in her esophagus as well. In the ED she was given 25mg benadryl IV, 125 mg solumedrol IV and pepcid 20 mg IV. This has helped the swelling some but her throat still hurts and it hurts to swallow. Nothing else was able to relieve the pain and nothing make it worse though she has not tried to drink any fluids because of trouble swallowing. She denies any recent travel, recent exposure to unusual plants or animals or other allergens. She has not started any new medications, has not used any new lotions or perfumes and has not eaten any unusual foods. Patient has not taken any of her oral medications today. Surgical History: s/p vaginal wall operation for prolapse 2006 s/p Cardiac stent in 1999 s/p hystarectomy in 1970s s/p kidney stone retrieval 1960s Medical History: +CAD w/ Left heart cath in 2005 showing 40% LAD, 50% small D2, 40% RCA and 30% large OM; 2006 TTE showing LVEF 60-65% with diastolic dysfunction, LVH, mild LA dilation +Hyperlipidemia +HTN +DM 2, last A1c 6.7 in 9/2005 +Asthma/COPD +GERD +h/o iron deficiency anemia Social History: Patient lives in _______ with daughter _____ (919) _______. -

Emergency Department Chief Complaint and Diagnosis Data to Detect Influenza-Like Illness with an Electronic Medical Record
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Emergency Department Chief Complaint and Diagnosis Data to Detect Influenza-Like Illness with an Electronic Medical Record Permalink https://escholarship.org/uc/item/9gq782tz Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 11(1) ISSN 1936-900X Authors May, Larissa S Griffin, Beth Ann Bauers, Nicole Maier et al. Publication Date 2010 License https://creativecommons.org/licenses/by-nc/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Original research Emergency Department Chief Complaint and Diagnosis Data to Detect Influenza-Like Illness with an Electronic Medical Record Larissa S. May, MD, MS* * The George Washington University, Department of Emergency Medicine, Beth Ann Griffin, PhD† Washington, D.C Nicole Maier Bauers, MS‡ † RAND Corporation, Center for Domestic and International Health Security, Arvind Jain, MS† Arlington VA Marsha Mitchum, MS, MPHҰ ‡ The George Washington University School of Public Health, Washington, D.C. Neal Sikka, MD* Ұ The George Washington University School of Medicine, Washington, D.C. Marianne Carim, MDҰ € Georgetown University School of Nursing and Health Studies Michael A. Stoto, PhD€ Supervising Section Editor: Scott E. Rudkin, MD, MBA Submission history: Submitted August 28, 2009; Revision Received July 22, 2009; Accepted July 22, 2009 Reprints available through open access at http://escholarship.org/uc/uciem_westjem Background: The purpose of syndromic surveillance is early detection of a disease outbreak. Such systems rely on the earliest data, usually chief complaint. The growing use of electronic medical records (EMR) raises the possibility that other data, such as emergency department (ED) diagnosis, may provide more specific information without significant delay, and might be more effective in detecting outbreaks if mechanisms are in place to monitor and report these data. -

The Oral Presentation Nersi Nikakhtar, M.D
Guidelines for the Oral Presentation Nersi Nikakhtar, M.D. University of Minnesota Medical School !1 Table of Contents The Oral Presentation: An Introduction ..................................3 Why Worry About the Oral Presentation? ...............................4 Presenting the New Patient .....................................................5 The Opening Statement ......................................................5 History of Present Illness ....................................................5 Past Medical History ...........................................................6 Medications/Allergies ..........................................................7 Social and Family History ...................................................7 Review of Systems ..............................................................7 Vitals .....................................................................................8 Physical Exam .....................................................................8 Labs and Studies .................................................................8 Summary Statement ............................................................8 Assessment and Plan ..........................................................9 The Follow Up (or Daily) Presentation: What's Different? ...................................................................11 The Outpatient (Known Patient) Presentation: What's Different? ...................................................................12 !2 The Oral Presentation: An Introduction The -

Chief Compaint/HPI History
PULMONOLOGY ASSOCIATES OF TEXAS 6860 North Dallas Pkwy, Ste 200, Plano, TX 75024 Tel: 469-305-7171 Fax: 469-212-1548 Patient Name: Thomas Cromwell Patient DOB: 02-09-1960 Patient Sex: Male Visit Date: 03-06-2016 Chief Compaint/HPI Chief Complaint: Shortness of Breath History of Present Illness: he patient is an 56-year-old male. From the last few days, he is not feeling well. Complains of fatigue, tiredness, weakness, nausea, no vomiting, no hematemesis or melena. The patient relates to have some low-grade fever. The patient came to the emergency room. Initially showed atrial fibrillation with rapid ventricular response. It appears that the patient has chronic atrial fibrillation. As per the medications, they are not very clear. He denies any specific chest pain. Her main complaint is shortness of breath and symptoms as above Pulmonary symptoms: cough, sputum, no hemoptysis, dyspnea and wheezing. History Past Medical History: Pulmonary history includes pneumonia and sleep apnea. Cardiac history includes atrial fibrillation and congestive heart failure. Remainder of PMH is non-significant. Surgical History: appendectomy in 2007. Medications: Pulmonary medications are albuterol and Spiriva; Cardiac medications include: atenolol and digoxin; Family History: Father is deceased at age 80. Father PMH remarkable for CHF, hypertension and MI; Mother is alive. Mother PMH remarkable for alzheimers, diabetes and hypertension; Cancer history in family: No Lung disease in the family: No Social History: Current every day smoker - 1 pack / day Alcohol consumption: social Marital status: lives alone Exposure History: Occupation: farmer. Asbestos exposure: None. No exposure to Ground Zero. Immunization History: Patient has an immunization history of flu shot, H1N1shot and pneumococcal shot. -

The Patient Interview
CHAPTER 1 The Patient Interview Sneha Baxi Srivastava, PharmD, BCACP LEARNING OBJECTIVES • Explain the basic communication skills needed when performing a patient interview. • Describe the components of the patient interview. • Conduct a thorough medication history. • Compare and contrast the different patient interview approaches in various clinical settings. • Adapt the interview technique based on the needs of the patient. KEY TERMS • Active Listening • Pertinent Positive • Rapport • Pertinent Negative • Empathy • Past History • Open-Ended Questions • Medication History • Leading Questions • Family History • Probing Questions • Personal and Social History • Nonverbal Communication • Review of Systems • Chief Complaint • Physical Exam • History of Present Illness • QuEST/SCHOLAR-MAC INTRODUCTION The patient interview is the primary way of obtaining comprehensive information about the patient in order to provide effective patient-centered care, and the medica- tion history component is the pharmacist’s expertise. A methodological approach is used to obtain information from the patient, usually starting with determining the patient’s chief complaint, also known as the reason for the healthcare visit, and then 2 CHAPTER 1 / The Patient Interview delving further into an exploration of the patient’s specific complaint and problem. A comprehensive patient interview includes inquiring about the patient’s medical, medication, social, personal, and family history, as well as a thorough review of systems and possibly a physical examination. The medication history is the part of the patient interview that provides the pharmacist the opportunity to utilize his or her expertise by precisely collecting each component of the medication history (however, a medication history may also be collected independent of a comprehensive patient interview). -

Medical Terminology Information Sheet
Medical Terminology Information Sheet: Medical Chart Organization: • Demographics and insurance • Flow sheets • Physician Orders Medical History Terms: • Visit notes • CC Chief Complaint of Patient • Laboratory results • HPI History of Present Illness • Radiology results • ROS Review of Systems • Consultant notes • PMHx Past Medical History • Other communications • PSHx Past Surgical History • SHx & FHx Social & Family History Types of Patient Encounter Notes: • Medications and medication allergies • History and Physical • NKDA = no known drug allergies o PE Physical Exam o Lab Laboratory Studies Physical Examination Terms: o Radiology • PE= Physical Exam y x-rays • (+) = present y CT and MRI scans • (-) = Ф = negative or absent y ultrasounds • nl = normal o Assessment- Dx (diagnosis) or • wnl = within normal limits DDx (differential diagnosis) if diagnosis is unclear o R/O = rule out (if diagnosis is Laboratory Terminology: unclear) • CBC = complete blood count o Plan- Further tests, • Chem 7 (or Chem 8, 14, 20) = consultations, treatment, chemistry panels of 7,8,14,or 20 recommendations chemistry tests • The “SOAP” Note • BMP = basic Metabolic Panel o S = Subjective (what the • CMP = complete Metabolic Panel patient tells you) • LFTs = liver function tests o O = Objective (info from PE, • ABG = arterial blood gas labs, radiology) • UA = urine analysis o A = Assessment (Dx and DDx) • HbA1C= diabetes blood test o P = Plan (treatment, further tests, etc.) • Discharge Summary o Narrative in format o Summarizes the events of a hospital stay -
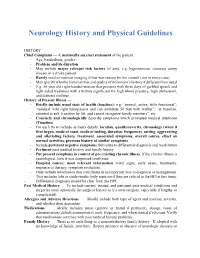
Neurology History and Physical Guidelines
Neurology History and Physical Guidelines HISTORY Chief Complaint — A maximally succinct statement of the patient: - Age, handedness, gender - Problem and its duration - May include major relevant risk factors (if any), e.g. hypertension, coronary artery disease in a stroke patient. - Rarely need to mention imaging if that was reason for the consult (not in every case) - May specify who the historian was and quality of informant’s history if different from usual - E.g: 56 year old right-handed woman that presents with three days of garbled speech and right sided weakness with a history significant for high blood pressure, high cholesterol, and diabetes mellitus History of Present Illness — - Briefly include usual state of health (baseline): e.g: “normal, active, fully functional”; “residual mild right hemiparesis and can ambulate 50 feet with walker”; “at baseline, oriented to self, transfers by lift, and cannot recognize family members”, etc. - Concisely and chronologically describe symptoms which prompted medical attentions (Timeline) - For each try to include as many details: location, quality/severity, chronology (when it first began, mode of onset, mode of ending, duration, frequency), setting, aggravating and alleviating factors, treatment, associated symptoms, overall course, effect on normal activities, previous history of similar symptoms - Include pertinent negative symptoms that relate to differential diagnosis and localization - Pertinent past medical history and family history - Put present symptoms in context of pre-existing chronic illness. If the chronic illness is neurological, how it was diagnosed/confirmed - Hospital course: most relevant information (vital signs, early exam, treatments, response to therapy, symptom evolution) - Only include information that contributes in an important way to diagnosis or management. -
The AOA Guide
The AOA Guide: How to Succeed in the Third-Year Clerkships Example Notes for the MSIII 2017 Preface This guide was created as a way of assisting you as you start your clinical training. For the rest of your professional life, you will write various notes. Although they will eventually become second nature to you, it is often challenging at first to figure out what information is pertinent to a particular specialty/rotation.This book is designed to help you through that process. In this book you will find samples of SOAP notes for each specialty and a complete History and Physical. Each of these notes represents very typical patients you will see on the rotation. Look at the way the notes are phrased and the information they contain. We have included an abbre- viations page at the end of this book so that you can refer to it for the short-forms with which you are not yet familiar. Pretty soon you will be using these abbrevia- tions without a problem! These notes can be used as a template from which you can adjust the information to apply to your patient. It is important to remember that these notes are not all inclusive, of course, and other physicians will give sugges- tions that you should heed. If you are ever having trouble, us fourth year medical students are always willing to help! ***NOTE: Many note-writing practices at Jefferson may change as the hospital transitions from paper notes to EMR.*** Table of Contents Internal Medicine Progress Note (SOAP) ............................................................3 Neurology Progress Note (SOAP) ......................................................................