"Survival Guide" to the Clinics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -

Cardiac Amyloidosis
Cardiac Amyloid: Contemporary Approach to Diagnosis and Advances in Treatment Cardiac Nursing Symposium October 17, 2019 Dana Miller AGPCNP-BC, CHFN The University of Kansas Medical Center Heart Failure Nurse Practitioner Oc Octob Learning objectives • Describe the different types of cardiac amyloidosis (Disease) • Recognize clinical manifestations of cardiac amyloidosis • Implement strategies for diagnosis of cardiac amyloidosis (Diagnosis) • Utilize recent clinical evidence for decisions about treatment of cardiac amyloidosis (Drugs and devices) What is the disease amyloidosis? • First described by Rudolf Virchow in 1858 describing the reaction of tissue deposits with iodine and sulfuric acid. • A disorder of misfolded proteins • Proteins circulate in the bloodstream and perform many functions in the body • Should be dissolved, in other words, liquid • In amyloid they become solid and deposit in organs and tissues in the body and cause problems Red flags for Cardiac Amyloidosis • Echocardiography • Low voltage on ECG and thickening of the septum/posterior wall>1.2 cm (unexplained increase in thickness) • Thickening of the RV free wall, valves Intolerance to bet blockers or ACEI Low normal BP inpatients with a previous history of HTN Donnelly and Hanna, 2017 JACC 2014 Red flags for AL • HFpEF + Nephrotic syndrome • Macroglossia and/or periorbital purpura • Orthostatic hypotension • Peripheral neuropathy • MGUS • Donnelly and Hanna, 2017 Red flags for ATTR • White male age>60 with HFpEF + history of carpal tunnel syndrome and or/spinal -

Recent Advances in the Diagnosis and Management of Amyloid Cardiomyopathy
Faculty Opinions Faculty Reviews 2021 10:(31) Recent advances in the diagnosis and management of amyloid cardiomyopathy Petra Nijst 1,2 W.H. Wilson Tang 3* 1 Department of Cardiology, Ziekenhuis Oost-Limburg, Genk, Belgium 2 Biomedical Research Institute, Faculty of Medicine and Life Sciences, Hasselt University, Diepenbeek, Belgium 3 Department of Cardiovascular Medicine, Heart and Vascular Institute, Cleveland Clinic, Cleveland, OH, USA Abstract Amyloidosis is a disorder characterized by misfolded precursor proteins that form depositions of fibrillar aggregates with an abnormal cross-beta-sheet conformation, known as amyloid, in the extracellular space of several tissues. Although there are more than 30 known amyloidogenic proteins, both hereditary and non-hereditary, cardiac amyloidosis (CA) typically arises from either misfolded transthyretin (ATTR amyloidosis) or immunoglobulin light-chain aggregation (AL amyloidosis). Its prevalence is more common than previously thought, especially among patients with heart failure and preserved ejection fraction (HFpEF) and aortic stenosis. If there is a clinical suspicion of CA, focused echocardiography, laboratory screening for the presence of a monoclonal protein (serum and urinary electrophoresis with immunofixation and serum free light-chain ratio), and cardiac scintigraphy with 99mtechnetium-labeled bone-tracers are sensitive and specific initial diagnostic tests. In some cases, more advanced/invasive techniques are necessary and, in the last several years, treatment options for both AL CA and ATTR CA have rapidly expanded. It is important to note that the aims of therapy are different. Systemic AL amyloidosis requires treatment targeted against the abnormal plasma cell clone, whereas therapy for ATTR CA must be targeted to the production and stabilization of the TTR molecule. -
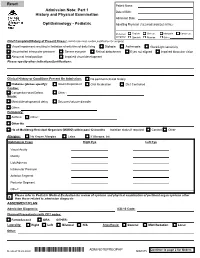
Adm Notepreophp
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

Transthyretin Amyloid Cardiomyopathy (ATTR-CM)—
BIOEQUIVALENCE / VYNDALINK / REFS When you’ve decided VYNDAMAX is appropriate for your patient, VyndaLink may be able to help ATTR-CM is a progressive, fatal Enroll your patients in VyndaLink for support or send prescriptions directly to an in-network Specialty Pharmacy disease—recognize the signs The VyndaLink team can: and symptoms to diagnose and treat 2,3 Conduct a benefits verification to Determine payer requirements and Identify Specialty Pharmacy options based your appropriate patients determine your patient’s coverage provide information about the prior on your patient’s insurance coverage. Transthyretin amyloid for VYNDAMAX, including out-of- authorization process and appeals VYNDAMAX is available through multiple pocket costs. process as needed.* Specialty Pharmacies in our defined distribution network. VYNDAMAX—once-daily, oral medication for patients with wild-type or hereditary ATTR-CM *Please note where a PA is required, the physician must submit required information directly to the patient’s insurer. cardiomyopathy (ATTR-CM)— Get started at www.VyndaLink.com a disease that may be present in Download the enrollment form. Completed form can be sent online at www.VyndaLinkPortal.com or Proven to reduce mortality and 1 AM PM patients with heart failure faxed to 1-888-878-8474. Call 1-888-222-8475 (Monday-Friday, 8 -8 ET) with any questions. CV-related hospitalization Consider prescribing oral VYNDAMAX for References: 1. Nativi-Nicolau J, Maurer MS. Amyloidosis cardiomyopathy: update in the diagnosis and treatment of the most common types. Curr Opin Cardiol. 2018;33(5):571-579. 2. Sipe JD, Benson MD, Buxbaum JN, et al. Amyloid bril proteins and amyloidosis: chemical identication and clinical classication International Society of Amyloidosis 2016 Nomenclature Guidelines. -

(June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION and WHY
DRAFT EVALUATION & MANAGEMENT DOCUMENTATION GUIDELINES (June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION AND WHY IS IT IMPORTANT? Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history including past and present illnesses, examinations, tests, treatments, and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high quality care. The medical record facilitates: · the ability of the physician and other health care professionals to evaluate and plan the patient's immediate treatment, and to monitor his/her health care over time. · communication and continuity of care among physicians and other health care professionals involved in the patient's care; · accurate and timely claims review and payment; · appropriate utilization review and quality of care evaluations; and · collection of data that may be useful for research and education. An appropriately documented medical record can reduce many of the "hassles" associated with claims processing and may serve as a legal document to verify the care provided, if necessary. WHAT DO PAYERS WANT AND WHY? Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate: · the site of service; · the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or · that services provided have been accurately reported. II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION The principles of documentation listed below are applicable to all types of medical and surgical Pg. 1 services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. -

A Guide to Transthyretin Amyloidosis
A Guide to Transthyretin Amyloidosis Authored by Teresa Coelho, Bo-Goran Ericzon, Rodney Falk, Donna Grogan, Shu-ichi Ikeda, Mathew Maurer, Violaine Plante-Bordeneuve, Ole Suhr, Pedro Trigo 2016 Edition Edited by Merrill Benson, Mathew Maurer What is amyloidosis? Amyloidosis is a systemic disorder characterized by extra cellular deposition of a protein-derived material, known as amyloid, in multiple organs. Amyloidosis occurs when native or mutant poly- peptides misfold and aggregate as fibrils. The amyloid deposits cause local damage to the cells around which they are deposited leading to a variety of clinical symptoms. There are at least 23 different proteins associated with the amyloidoses. The most well-known type of amyloidosis is associated with a hematological disorder, in which amyloid fibrils are derived from monoclonal immunoglobulin light-chains (AL amyloidosis). This is associated with a clonal plasma cell disorder, closely related to and not uncommonly co-existing with multiple myeloma. Chronic inflammatory conditions such as rheumatoid arthritis or chronic infections such as bronchiectasis are associated with chronically elevated levels of the inflammatory protein, serum amyloid A, which may misfold and cause AA amyloidosis. The hereditary forms of amyloidosis are autosomal dominant diseases characterized by deposition of variant proteins, in dis- tinctive tissues. The most common hereditary form is transthyretin amyloidosis (ATTR) caused by the misfolding of protein monomers derived from the tetrameric protein transthyretin (TTR). Mutations in the gene for TTR frequently re- sult in instability of TTR and subsequent fibril formation. Closely related is wild-type TTR in which the native TTR protein, particu- larly in the elderly, can destabilize and re-aggregate causing non- familial cases of TTR amyloidosis. -

Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019
Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019 Centers for Medicare & Medicaid Services PRA Disclosure Statement According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is x. The time required to complete this information collection is estimated to average 0.3 minutes per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. This estimate does not include time for training. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850. *****CMS Disclaimer*****Please do not send applications, claims, payments, medical records or any documents containing sensitive information to the PRA Reports Clearance Office. Please note that any correspondence not pertaining to the information collection burden approved under the associated OMB control number listed on this form will not be reviewed, forwarded, or retained. If you have questions or concerns regarding where to submit your documents, please contact Joan Proctor National Coordinator, Home Health Quality Reporting Program Centers for Medicare & Medicaid. OASIS-D Guidance Manual Table of Contents Page -

General Rules of the Marquette General Health System Medical Staff
General Rules of the Marquette General Health System Medical Staff I. PATIENT ADMISSION, ALTERNATE COVERAGE, TRANSFER, DISCHARGE AND DEATH 1.1 ADMISSION CRITERIA 1.1-1 Who may admit patients. Only a Member with admitting privileges may admit or co-admit a patient to the Hospital. Except as provided for Qualified Oral Surgeons, Podiatrists and Independent Allied Health Professionals in the Medical Staff Bylaws, a physician Member will be responsible for the general medical care and treatment of every patient admitted to the Hospital. Medical care may be provided by a Resident, other specified professional personnel or Allied Health Staff members provided they are working under the supervision of a Practitioner with clinical privileges. Medical care will be provided only by Members and Hospital support staff authorized to perform such services. 1.1-2 Admission Information. An admitting Practitioner will provide the following information in the patient’s medical record, if such information is available to the admitting Practitioner: (a) Provisional diagnosis. (b) A valid reason for admitting the patient, including information to support the medical necessity and the appropriateness of the admission. (c) Information needed to properly care for the patient being admitted. (d) Information needed to protect the patient from himself/herself. (e) Information needed to protect Hospital personnel and others from potential problems or dangers presented by the patient. (f) Information deemed necessary by the Hospital. 1.1-3 Admission of potentially suicidal or dangerous patients. If an admitting Practitioner reasonably believes a patient admitted for other purposes is potentially suicidal or dangerous to himself/herself or others, the admitting Practitioner will promptly obtain a consultation from a suitable mental health professional. -
Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents
U.S. DEPARTMENT OF VETERANS AFFAIRS Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents “Supervising Practitioner” (synonymous with “Attending”): Responsible for all care in which interns, residents or fellows are involved. “Resident” is used to apply to physician, dentist, optometrist, and podiatrist residents and fellows, regardless of training level. Documentation of all patient encounters must identify the supervising practitioner (attending) by name and indicate the level of involvement. Depending upon the clinical situation, Four types of documentation of resident supervision are allowed: 1. Attending’s progress note or other entry into the patient health record. 2. Attending’s addendum to the resident admission or progress note. 3. Co-signature by the attending implies that the attending has reviewed the resident note or other health record entry, and absent an addendum to the contrary, concurs with the content of the resident note or entry. Use of CPRS function "Additional Signer" is not acceptable for documenting supervision. 4. Resident documentation of attending supervision. [Includes involvement of the attending and the attending’s level of supervision or oversight responsibility (e.g., "I have seen and discussed the patient with my attending, Dr. 'X', and Dr. 'X' agrees with my assessment and plan"), at a minimum, the responsible attending should be identified (e.g., "The attending of record for this patient encounter is Dr. 'X'")] Outpatient: New Patient Visit (includes Emergency Department visits) Attending must be physically present in the clinic. Every patient who is new to the facility must be seen by or discussed with an attending. Documentation: An independent note, addendum to the resident's note, or resident note description of attending involvement. -

Student Clerkship Guide a Comprehensive Guide to Clerkship at the Ottawa Hospital
STUDENT CLERKSHIP GUIDE A COMPREHENSIVE GUIDE TO CLERKSHIP AT THE OTTAWA HOSPITAL Gemma Cox and Stephanie Lubchansky MD 2015 CANDIDATES SPECIAL THANKS To Dr. Krista Wooller for her guidance, support, and feedback during the writing process. The Faculty of Medicine at the University of Ottawa for supporting this endeavor. EDITORS-IN-CHIEF EDITORS Gemma Cox, MD Candidate 2015 Pierre-Olivier Auclair, Mandatory Selectives Coordinator Stephanie Lubchansky, MD Candidate 2015 Dr. Contreras-Dominguez, Internal Medicine Rotation Director FACULTY SUPERVISOR Kelly Frydrych, MD Candidate 2015 Dr. Krista Wooller Julie Ghatalia, Department of Anesthesiology CONTRIBUTORS Celine Giordano, MD Candidate 2015 Kevin Dong, MD Candidate 2015 Hilary Gore, Department of Obstetrics and Bani Falcon, MD Candidate 2015 Gynecology Kelly Frydrych, MD Candidate 2015 Dr. Laura Hopkins, Obstetrics and Habibat Garuba, PGY-2 Internal Medicine Gynecology Rotation Director Celine Giordano, MD Candidate 2015 Dr. B.K. Lam, Surgery Rotation Director Anne McHale, MD Candidate 2015 Dr. Tim Lau, Department of Psychiatry Department of Pediatrics, Children’s Dr. Safeena Kherani, Mandatory Selectives Hospital of Eastern Ontario (CHEO) Rotation Director Department of Surgery, The Ottawa Anne McHale, MD Candidate 2015 Hospital Dr. Eoghan O’Shea, Family Medicine Rotation Diector Dr. Nikhil Rastogi, Anesthesiology Rotation Director Brigitte Rutherford, Department of Psychiatry Denis Vadeboncoeur, 3rd year Liaison Officer Dr. Krista Wooller, Department of Internal Medicine Amy Whyte, Department of Surgery Donna Williams, Department of Family Medicine Dr. Stella Yiu, Emergency Medicine Rotation Director Dr. Marc Zucker, Pediatrics Rotation Director A FEW WORDS FROM THE EDITORS IN CHIEF… This guide was created to help orient you, the incoming clerkship class, to the many experiences that you will encounter over the course of this year. -

Cardiac Amyloidosis
Cardiac Amyloidosis Ronald Witteles, MD Stanford University & Brendan M. Weiss, MD University of Pennsylvania Amyloidosis: What is it? • Amylum – Starch (Latin) • Generic term for many diseases: • Protein misfolds into β-sheets • Forms into 8-10 nm fibrils • Extracellular deposition into amyloid deposits Types of Amyloid – Incomplete List • Systemic: • Light chains (AL) – “Primary ” • Transthyretin (ATTR) – “Senile ” or “Familial ” or “FAC” or “FAP” • Serum amyloid A (AA) – “Secondary ” • Localized – Not to be memorized! • Beta-2 microglobulin (A-β2) – Dialysis (osteoarticular structures) • Apolipoprotein A-1 (AApoA-I) – Age-related (aortic intima, cardiac, neuropathic) • Apolipoprotein A-2 (AApoA-2) – Hereditary (kidney) • Calcitonin (ACal) – Complication of thyroid medullary CA • Islet amyloid polypeptide (AIAPP) – Age-related (seen in DM) • Atrial natriuretic peptide (AANF) – Age-related (atrial amyloidosis) • Prolactin (APro) – Age-related, pituitary tumors • Insulin (AIns) – Insulin-pump use (local effects) • Amyloid precursor protein (ABeta) – Age-related/hereditary (Alzheimers) • Prion protein (APrPsc) – Hereditary/sporadic (spongiform encephalopathies) • Cystatin-C (ACys) – Hereditary (cerebral hemorrhage) • Fibrinogen alpha chain (AFib) – Hereditary (kidney) • Lysozome (ALys) – Hereditary (Diffuse, especially kidney, spares heart) • Medin/Lactadherin – Age-related (medial aortic amyloidosis) • Gelsolin (AGel) – Hereditary (neuropathic, corneal) • Keratin – Cutaneous AL: A Brief Dive into Hematology… Plasma cells: Make antibodies