The Value of the Physical Examination in Clinical Practice: an International Survey
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -

A Neurological Examination
THE 3 MINUTE NEUROLOGICAL EXAMINATION DEMYSTIFIED Faculty: W.J. Oczkowski MD, FRCPC Professor and Academic Head, Division of Neurology, Department of Medicine, McMaster University Stroke Neurologist, Hamilton Health Sciences Relationships with commercial interests: ► Not Applicable Potential for conflict(s) of interest: ► Not Applicable Mitigating Potential Bias ► All the recommendations involving clinical medicine are based on evidence that is accepted within the profession. ► All scientific research referred to, reported, or used is in the support or justification of patient care. ► Recommendations conform to the generally accepted standards. ► Independent content validation. ► The presentation will mitigate potential bias by ensuring that data and recommendations are presented in a fair and balanced way. ► Potential bias will be mitigated by presenting a full range of products that can be used in this therapeutic area. ► Information of the history, development, funding, and the sponsoring organizations of the disclosure presented will be discussed. Objectives ► Overview of neurological assessment . It’s all about stroke! . It’s all about the chief complaint and history. ► Overview: . 3 types of clinical exams . Neurological signs . Neurological localization o Pathognomonic signs o Upper versus lower motor neuron signs ► Cases and practice Bill ► 72 year old male . Hypertension . Smoker ► Stroke call: dizzy, facial droop, slurred speech ► Neurological Exam: . Ptosis and miosis on left . Numb left face . Left palatal weakness . Dysarthria . Ataxic left arm and left leg . Numb right arm and leg NIH Stroke Scale Score ► LOC: a,b,c_________________ 0 ► Best gaze__________________ 0 0 ► Visual fields________________ 0 ► Facial palsy________________ 0 ► Motor arm and leg__________ -Left Ptosis 2 -Left miosis ► Limb ataxia________________ -Weakness of 1 ► Sensory_______________________ left palate ► Best Language______________ 0 1 ► Dysarthria_________________ 0 ► Extinction and inattention____ - . -

Central Venous Pressure Venous Examination but Underestimates Ultrasound Accurately Reflects the Jugular
Ultrasound Accurately Reflects the Jugular Venous Examination but Underestimates Central Venous Pressure Gur Raj Deol, Nicole Collett, Andrew Ashby and Gregory A. Schmidt Chest 2011;139;95-100; Prepublished online August 26, 2010; DOI 10.1378/chest.10-1301 The online version of this article, along with updated information and services can be found online on the World Wide Web at: http://chestjournal.chestpubs.org/content/139/1/95.full.html Chest is the official journal of the American College of Chest Physicians. It has been published monthly since 1935. Copyright2011by the American College of Chest Physicians, 3300 Dundee Road, Northbrook, IL 60062. All rights reserved. No part of this article or PDF may be reproduced or distributed without the prior written permission of the copyright holder. (http://chestjournal.chestpubs.org/site/misc/reprints.xhtml) ISSN:0012-3692 Downloaded from chestjournal.chestpubs.org at UCSF Library & CKM on January 21, 2011 © 2011 American College of Chest Physicians CHEST Original Research CRITICAL CARE Ultrasound Accurately Refl ects the Jugular Venous Examination but Underestimates Central Venous Pressure Gur Raj Deol , MD ; Nicole Collett , MD ; Andrew Ashby , MD ; and Gregory A. Schmidt , MD , FCCP Background: Bedside ultrasound examination could be used to assess jugular venous pressure (JVP), and thus central venous pressure (CVP), more reliably than clinical examination. Methods: The study was a prospective, blinded evaluation comparing physical examination of external jugular venous pressure (JVPEXT), internal jugular venous pressure (JVPINT), and ultrasound collapse pressure (UCP) with CVP measured using an indwelling catheter. We com- pared the examination of the external and internal JVP with each other and with the UCP and CVP. -
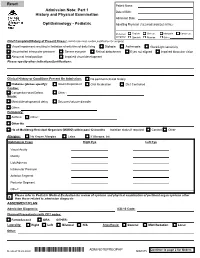
Adm Notepreophp
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

Bates' Pocket Guide to Physical Examination and History Taking
Lynn S. Bickley, MD, FACP Clinical Professor of Internal Medicine School of Medicine University of New Mexico Albuquerque, New Mexico Peter G. Szilagyi, MD, MPH Professor of Pediatrics Chief, Division of General Pediatrics University of Rochester School of Medicine and Dentistry Rochester, New York Acquisitions Editor: Elizabeth Nieginski/Susan Rhyner Product Manager: Annette Ferran Editorial Assistant: Ashley Fischer Design Coordinator: Joan Wendt Art Director, Illustration: Brett MacNaughton Manufacturing Coordinator: Karin Duffield Indexer: Angie Allen Prepress Vendor: Aptara, Inc. 7th Edition Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2009 by Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2007, 2004, 2000 by Lippincott Williams & Wilkins. Copyright © 1995, 1991 by J. B. Lippincott Company. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appear- ing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at Two Commerce Square, 2001 Market Street, Philadelphia PA 19103, via email at [email protected] or via website at lww.com (products and services). 9 8 7 6 5 4 3 2 1 Printed in China Library of Congress Cataloging-in-Publication Data Bickley, Lynn S. Bates’ pocket guide to physical examination and history taking / Lynn S. -

1- Assessing Pain
Foundations of Assessing and Treating Pain Assessing Pain Table of Contents Assessing Pain........................................................................................................................................2 Goal:..............................................................................................................................................2 After completing this module, participants will be able to:..............................................................2 Professional Practice Gaps............................................................................................................2 Introduction............................................................................................................................................. 2 Assessment and Diagnosis of Pain Case: Ms. Ward..........................................................................3 Confidentiality..........................................................................................................................................4 Pain History: A Standardized Approach..................................................................................................4 Evaluating Pain Using PQRSTU: Steps P, Q, R, S T, and U..............................................................5 Ms. Ward's Pain History (P, Q, R, S, T, U)..........................................................................................6 Video: Assessing Pain Systematically with PQRTSTU Acronym........................................................8 -

Medical Staff Medical Record Policy
Number: MS -012 Effective Date: September 26, 2016 BO Revised:11/28/2016; 11/27/2017; 1/22/2018; 8/27/2018 CaroMont Regional Medical Center Author: Approved: Patrick Russo, MD, Chief-of-Staff Authorized: Todd Davis, MD, EVP, GMO MEDICAL STAFF MEDICAL RECORD POLICY 1. REQUIRED COMPONENTS OF THE MEDICAL RECORD The medical record shall include information to support the patient's diagnosis and condition, justify the patient's care, treatment and services, and document the course and result of the patient's care, and services to promote continuity of care among providers. The components may consist of the following: identification data, history and physical examination, consultations, clinical laboratory findings, radiology reports, procedure and anesthesia consents, medical or surgical treatment, operative report, pathological findings, progress notes, final diagnoses, condition on discharge, autopsy report when performed, other pertinent information and discharge summary. 2. ADMISSION HISTORY AND PHYSICAL EXAMINATION FOR HOSPITAL CARE Please refer to CaroMont Regional Medical Center Medical Staff Bylaws, Section 12.E. A. The history and physical examination (H&P), when required, shall be performed and recorded by a physician, dentist, podiatrist, or privileged practitioner who has an active NC license and has been granted privileges by the hospital. The H&P is the responsibility of the attending physician or designee. Oral surgeons, dentists, and podiatrists are responsible for the history and physical examination pertinent to their area of specialty. B. If a physician has delegated the responsibility of completing or updating an H&P to a privileged practitioner who has been granted privileges to do H&Ps, the H&P and/or update must be countersigned by the supervisor physician within 30 days after discharge to complete the medi_cal record. -

Medical History and Physical Examination Worksheet
U.S. Department of State OMB No. 1405-0113 EXPIRATION DATE: xx/xx/20xx MEDICAL HISTORY AND ESTIMATED BURDEN: 15 minutes PHYSICAL EXAMINATION WORKSHEET (See Page 2 - Back of Form) Photo Surnames Given Names Exam Date (mm-dd-yyyy) I Birth Date (mm-dd-yyyy) Document Type Document Number Case or Alien Number I I 1. Medical History (Past or present) No Yes No Yes Obstetrics Applicant appears to be providing unreliable or false Pregnant, on day of exam □ □ information, specify in remarks □ □ Estimated delivery date (mm-dd-yyyy) General LMP □ □ Illness or injury requiring hospitalization (including psychiatric) □ □ Previous live births, number: Birth dates of live births (mm-dd-yyyy) Cardiology □ □ Hypertension □ □ Congestive heart failure or coronary artery disease Arrhythmia □ □ Sexually Transmitted Diseases □ □ Rheumatic heart disease Congenital heart disease Previous treatment for sexually transmitted diseases, □ □ specify date (mm-yyyy) and treatment: Pulmonology □ □ Syphilis □ □ Tobacco use: □ Current □ Former □ □ Gonorrhea □ □ Asthma Chronic obstructive pulmonary disease □ □ Endocrinology Tuberculosis history: Diagnosed (mm-yyyy) □ □ □ □ Diabetes Treatment Completed (mm-yyyy) Thyroid disease Diagnosed (mm-yyyy) □ □ Treatment Completed (mm-yyyy) Hematologic/Lymphatic Diagnosed (mm-yyyy) □ □ Anemia Treatment Completed (mm-yyyy) □ □ Sickle Cell Disease □ □ Fever □ □ Thalassemia □ □ Cough Other hemoglobinopathy Night sweats □ □ □ □ Other □ □ Weight loss □ □ An abnormal or reactive HIV blood test Psychiatry Diagnosed (mm-yyyy) □ □ Psychological/Psychiatric -

General Rules of the Marquette General Health System Medical Staff
General Rules of the Marquette General Health System Medical Staff I. PATIENT ADMISSION, ALTERNATE COVERAGE, TRANSFER, DISCHARGE AND DEATH 1.1 ADMISSION CRITERIA 1.1-1 Who may admit patients. Only a Member with admitting privileges may admit or co-admit a patient to the Hospital. Except as provided for Qualified Oral Surgeons, Podiatrists and Independent Allied Health Professionals in the Medical Staff Bylaws, a physician Member will be responsible for the general medical care and treatment of every patient admitted to the Hospital. Medical care may be provided by a Resident, other specified professional personnel or Allied Health Staff members provided they are working under the supervision of a Practitioner with clinical privileges. Medical care will be provided only by Members and Hospital support staff authorized to perform such services. 1.1-2 Admission Information. An admitting Practitioner will provide the following information in the patient’s medical record, if such information is available to the admitting Practitioner: (a) Provisional diagnosis. (b) A valid reason for admitting the patient, including information to support the medical necessity and the appropriateness of the admission. (c) Information needed to properly care for the patient being admitted. (d) Information needed to protect the patient from himself/herself. (e) Information needed to protect Hospital personnel and others from potential problems or dangers presented by the patient. (f) Information deemed necessary by the Hospital. 1.1-3 Admission of potentially suicidal or dangerous patients. If an admitting Practitioner reasonably believes a patient admitted for other purposes is potentially suicidal or dangerous to himself/herself or others, the admitting Practitioner will promptly obtain a consultation from a suitable mental health professional. -
Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents
U.S. DEPARTMENT OF VETERANS AFFAIRS Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents “Supervising Practitioner” (synonymous with “Attending”): Responsible for all care in which interns, residents or fellows are involved. “Resident” is used to apply to physician, dentist, optometrist, and podiatrist residents and fellows, regardless of training level. Documentation of all patient encounters must identify the supervising practitioner (attending) by name and indicate the level of involvement. Depending upon the clinical situation, Four types of documentation of resident supervision are allowed: 1. Attending’s progress note or other entry into the patient health record. 2. Attending’s addendum to the resident admission or progress note. 3. Co-signature by the attending implies that the attending has reviewed the resident note or other health record entry, and absent an addendum to the contrary, concurs with the content of the resident note or entry. Use of CPRS function "Additional Signer" is not acceptable for documenting supervision. 4. Resident documentation of attending supervision. [Includes involvement of the attending and the attending’s level of supervision or oversight responsibility (e.g., "I have seen and discussed the patient with my attending, Dr. 'X', and Dr. 'X' agrees with my assessment and plan"), at a minimum, the responsible attending should be identified (e.g., "The attending of record for this patient encounter is Dr. 'X'")] Outpatient: New Patient Visit (includes Emergency Department visits) Attending must be physically present in the clinic. Every patient who is new to the facility must be seen by or discussed with an attending. Documentation: An independent note, addendum to the resident's note, or resident note description of attending involvement. -

Teaching Bedside Physical Examination with Ultrasound
SHARE DECEMBER 2019 V42, NO.12 MEDICAL EDUCATION: PART II TEACHING BEDSIDE PHYSICAL EXAMINATION WITH ULTRASOUND: AN OPPORTUNITY TO RE-ENGAGE AND INVIGORATE LEARNERS Kang Zhang, MD, FACP; Irene Ma, MD, PhD, FRCPC, FACP, RDMS, RDCS Dr. Zhang ([email protected]) is associate program director, Internal Medicine Residency Spokane, and clinical instructor and internal medicine clerkship director, University of Washington School of Medicine-Spokane. Dr. Ma ([email protected]) is associate professor, Division of General Internal Medicine, director of ultrasonography and procedural skills, Internal Medicine Residency Program, University of Calgary. he bedside physical examination is an integral pleural effusion.3 However, accuracy of the examination component of the clinical encounter. However, is limited by patient characteristics and size of the effu- Twith decreased time spent teaching at the bedside,1 sions. POCUS offers direct visualization of the pleural there has been a notable decline in physical exam skills effusion, confirming not only of its presence, but also among medical trainees. In the past decade, there has allows for a visual estimation of its size. Bedside rounds been increasing literature supporting the use of point-of- is an excellent way to illustrate ultrasound augmented care ultrasound (POCUS) to augment the physical exam physical examination to learners. As the patient is sitting to better guide physicians with clinical decision making.2 upright, learners are asked to determine if pleural effu- In this article, we describe a strategy to teach bedside sion is present or absent by the traditional physical exam physical examination skills by incorporating POCUS, on both hemithoraces. A mark is made at the first area which provides immediate visual feedback to the learn- of dullness that either represents the diaphragm or top of ers. -

Student Clerkship Guide a Comprehensive Guide to Clerkship at the Ottawa Hospital
STUDENT CLERKSHIP GUIDE A COMPREHENSIVE GUIDE TO CLERKSHIP AT THE OTTAWA HOSPITAL Gemma Cox and Stephanie Lubchansky MD 2015 CANDIDATES SPECIAL THANKS To Dr. Krista Wooller for her guidance, support, and feedback during the writing process. The Faculty of Medicine at the University of Ottawa for supporting this endeavor. EDITORS-IN-CHIEF EDITORS Gemma Cox, MD Candidate 2015 Pierre-Olivier Auclair, Mandatory Selectives Coordinator Stephanie Lubchansky, MD Candidate 2015 Dr. Contreras-Dominguez, Internal Medicine Rotation Director FACULTY SUPERVISOR Kelly Frydrych, MD Candidate 2015 Dr. Krista Wooller Julie Ghatalia, Department of Anesthesiology CONTRIBUTORS Celine Giordano, MD Candidate 2015 Kevin Dong, MD Candidate 2015 Hilary Gore, Department of Obstetrics and Bani Falcon, MD Candidate 2015 Gynecology Kelly Frydrych, MD Candidate 2015 Dr. Laura Hopkins, Obstetrics and Habibat Garuba, PGY-2 Internal Medicine Gynecology Rotation Director Celine Giordano, MD Candidate 2015 Dr. B.K. Lam, Surgery Rotation Director Anne McHale, MD Candidate 2015 Dr. Tim Lau, Department of Psychiatry Department of Pediatrics, Children’s Dr. Safeena Kherani, Mandatory Selectives Hospital of Eastern Ontario (CHEO) Rotation Director Department of Surgery, The Ottawa Anne McHale, MD Candidate 2015 Hospital Dr. Eoghan O’Shea, Family Medicine Rotation Diector Dr. Nikhil Rastogi, Anesthesiology Rotation Director Brigitte Rutherford, Department of Psychiatry Denis Vadeboncoeur, 3rd year Liaison Officer Dr. Krista Wooller, Department of Internal Medicine Amy Whyte, Department of Surgery Donna Williams, Department of Family Medicine Dr. Stella Yiu, Emergency Medicine Rotation Director Dr. Marc Zucker, Pediatrics Rotation Director A FEW WORDS FROM THE EDITORS IN CHIEF… This guide was created to help orient you, the incoming clerkship class, to the many experiences that you will encounter over the course of this year.