Foundations of Physical Examination and History Taking
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

International Journal of Medical and Health Sciences
International Journal of Medical and Health Sciences Journal Home Page: http://www.ijmhs.net ISSN:2277-4505 Review article Examining the liver – Revisiting an old friend Cyriac Abby Philips1*, Apurva Pande2 1Department of Hepatology and Transplant Medicine, PVS Institute of Digestive Diseases, PVS Memorial Hospital, Kaloor, Kochi, Kerala, India, 2Department of Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India. ABSTRACT In the current era of medical practice, super saturated with investigations of choice and development of diagnostic tools, clinical examination is a lost art. In this review we briefly discuss important aspects of examination of the liver, which is much needed in decision making on investigational approach. We urge the new medical student or the newly practicing physician to develop skills in clinical examination for resourceful management of the patient. KEYWORDS: Liver, examination, clinical skills, hepatomegaly, chronic liver disease, portal hypertension, liver span INTRODUCTION respiration, the excursion of liver movement is around 2 to 3 The liver attains its adult size by the age of 15 years. The cm. Castell and Frank has elegantly described normal liver liver weighs 1.2 to 1.4 kg in women and 1.4 to 1.5 kg in span in men and women utilizing the percussion method men. The liver seldom extends more than 5 cm beyond the (Table 1). Accordingly, the mean liver span is 10.5 cm for midline towards the left costal margin. During inspiration, men and 7 cm in women. During examination, a span 2 to 3 the diaphragmatic exertion moves the liver downward with cm larger or smaller than these values is considered anterior surface rotating to the right. -

The Stethoscope: Some Preliminary Investigations
695 ORIGINAL ARTICLE The stethoscope: some preliminary investigations P D Welsby, G Parry, D Smith Postgrad Med J: first published as on 5 January 2004. Downloaded from ............................................................................................................................... See end of article for Postgrad Med J 2003;79:695–698 authors’ affiliations ....................... Correspondence to: Dr Philip D Welsby, Western General Hospital, Edinburgh EH4 2XU, UK; [email protected] Submitted 21 April 2003 Textbooks, clinicians, and medical teachers differ as to whether the stethoscope bell or diaphragm should Accepted 30 June 2003 be used for auscultating respiratory sounds at the chest wall. Logic and our results suggest that stethoscope ....................... diaphragms are more appropriate. HISTORICAL ASPECTS note is increased as the amplitude of the sound rises, Hippocrates advised ‘‘immediate auscultation’’ (the applica- resulting in masking of higher frequency components by tion of the ear to the patient’s chest) to hear ‘‘transmitted lower frequencies—‘‘turning up the volume accentuates the sounds from within’’. However, in 1816 a French doctor, base’’ as anyone with teenage children will have noted. Rene´The´ophile Hyacinth Laennec invented the stethoscope,1 Breath sounds are generated by turbulent air flow in the which thereafter became the identity symbol of the physician. trachea and proximal bronchi. Airflow in the small airways Laennec apparently had observed two children sending and alveoli is of lower velocity and laminar in type and is 6 signals to each other by scraping one end of a long piece of therefore silent. What is heard at the chest wall depends on solid wood with a pin, and listening with an ear pressed to the conductive and filtering effect of lung tissue and the the other end.2 Later, in 1816, Laennec was called to a young characteristics of the chest wall. -
General Physical Examination Skills for Ahps
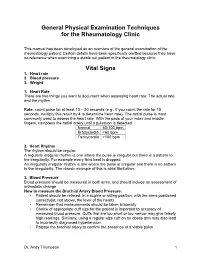
General Physical Examination Techniques for the Rheumatology Clinic This manual has been developed as an overview of the general examination of the rheumatology patient. Certain details have been specifically omitted because they have no relevance when examining a stable out patient in the rheumatology clinic. Vital Signs 1. Heart rate 2. Blood pressure 3. Weight 1. Heart Rate There are two things you want to document when assessing heart rate: The actual rate and the rhythm. Rate: count pulse for at least 15 – 30 seconds (e.g., if you count the rate for 15 seconds, multiply this result by 4 to determine heart rate). The radial pulse is most commonly used to assess the heart rate. With the pads of your index and middle fingers, compress the radial artery until a pulsation is detected. Normal 60-100 bpm Bradycardia <60 bpm Tachycardia >100 bpm 2. Heart Rhythm The rhythm should be regular. A regularly irregular rhythm is one where the pulse is irregular but there is a pattern to the irregularity. For example every third beat is dropped. An irregularly irregular rhythm is one where the pulse is irregular and there is no pattern to the irregularity. The classic example of this is atrial fibrillation. 3. Blood Pressure Blood pressure should be measured in both arms, and should include an assessment of orthostatic change How to measure the Brachial Artery Blood Pressure: • Patient should be relaxed, in a supine or sitting position, with the arms positioned correctly(at, not above, the level of the heart) • Remember that measurements should be taken bilaterally • Choice of appropriate cuff size for the patient is important to accuracy of measured blood pressure. -

HEENT EXAMINIATION ______HEENT Exam Exam Overview
HEENT EXAMINIATION ____________________________________________________________ HEENT Exam Exam Overview I. Head A. Visual inspection B. Palpation of scalp II. Eyes A. Visual Acuity B. Visual Fields C. Extraocular Movements/Near Response D. Inspection of sclera & conjunctiva E. Pupils F. Ophthalmoscopy III. Ears A. External Inspection B. Otoscopy C. Hearing Acuity D. Weber/Rinne IV. Nose A. External Inspection B. Speculum/otoscope C. Sinus areas V. Throat/Mouth A. Mouth Examination B. Pharynx Examination C. Bimanual Palpation VI. Neck A. Lymph nodes B. Thyroid gland 29 HEENT EXAMINIATION ____________________________________________________________ HEENT Terms Acuity – (ehk-yu-eh-tee) sharpness, clearness, and distinctness of perception or vision. Accommodation - adjustment, especially of the eye for seeing objects at various distances. Miosis – (mi-o-siss) constriction of the pupil of the eye, resulting from a normal response to an increase in light or caused by certain drugs or pathological conditions. Conjunctiva – (kon-junk-ti-veh) the mucous membrane lining the inner surfaces of the eyelids and anterior part of the sclera. Sclera – (sklehr-eh) the tough fibrous tunic forming the outer envelope of the eye and covering all of the eyeball except the cornea. Cornea – (kor-nee-eh) clear, bowl-shaped structure at the front of the eye. It is located in front of the colored part of the eye (iris). The cornea lets light into the eye and partially focuses it. Glaucoma – (glaw-ko-ma) any of a group of eye diseases characterized by abnormally high intraocular fluid pressure, damaged optic disk, hardening of the eyeball, and partial to complete loss of vision. Conductive hearing loss - a hearing impairment of the outer or middle ear, which is due to abnormalities or damage within the conductive pathways leading to the inner ear. -

Central Venous Pressure Venous Examination but Underestimates Ultrasound Accurately Reflects the Jugular
Ultrasound Accurately Reflects the Jugular Venous Examination but Underestimates Central Venous Pressure Gur Raj Deol, Nicole Collett, Andrew Ashby and Gregory A. Schmidt Chest 2011;139;95-100; Prepublished online August 26, 2010; DOI 10.1378/chest.10-1301 The online version of this article, along with updated information and services can be found online on the World Wide Web at: http://chestjournal.chestpubs.org/content/139/1/95.full.html Chest is the official journal of the American College of Chest Physicians. It has been published monthly since 1935. Copyright2011by the American College of Chest Physicians, 3300 Dundee Road, Northbrook, IL 60062. All rights reserved. No part of this article or PDF may be reproduced or distributed without the prior written permission of the copyright holder. (http://chestjournal.chestpubs.org/site/misc/reprints.xhtml) ISSN:0012-3692 Downloaded from chestjournal.chestpubs.org at UCSF Library & CKM on January 21, 2011 © 2011 American College of Chest Physicians CHEST Original Research CRITICAL CARE Ultrasound Accurately Refl ects the Jugular Venous Examination but Underestimates Central Venous Pressure Gur Raj Deol , MD ; Nicole Collett , MD ; Andrew Ashby , MD ; and Gregory A. Schmidt , MD , FCCP Background: Bedside ultrasound examination could be used to assess jugular venous pressure (JVP), and thus central venous pressure (CVP), more reliably than clinical examination. Methods: The study was a prospective, blinded evaluation comparing physical examination of external jugular venous pressure (JVPEXT), internal jugular venous pressure (JVPINT), and ultrasound collapse pressure (UCP) with CVP measured using an indwelling catheter. We com- pared the examination of the external and internal JVP with each other and with the UCP and CVP. -

CASE REPORT 48-Year-Old Man
THE PATIENT CASE REPORT 48-year-old man SIGNS & SYMPTOMS – Acute hearing loss, tinnitus, and fullness in the left ear Dennerd Ovando, MD; J. Walter Kutz, MD; Weber test lateralized to the – Sergio Huerta, MD right ear Department of Surgery (Drs. Ovando and Huerta) – Positive Rinne test and and Department of normal tympanometry Otolaryngology (Dr. Kutz), UT Southwestern Medical Center, Dallas; VA North Texas Health Care System, Dallas (Dr. Huerta) Sergio.Huerta@ THE CASE UTSouthwestern.edu The authors reported no A healthy 48-year-old man presented to our otolaryngology clinic with a 2-hour history of potential conflict of interest hearing loss, tinnitus, and fullness in the left ear. He denied any vertigo, nausea, vomiting, relevant to this article. otalgia, or otorrhea. He had noticed signs of a possible upper respiratory infection, including a sore throat and headache, the day before his symptoms started. His medical history was unremarkable. He denied any history of otologic surgery, trauma, or vision problems, and he was not taking any medications. The patient was afebrile on physical examination with a heart rate of 48 beats/min and blood pressure of 117/68 mm Hg. A Weber test performed using a 512-Hz tuning fork lateral- ized to the right ear. A Rinne test showed air conduction was louder than bone conduction in the affected left ear—a normal finding. Tympanometry and otoscopic examination showed the bilateral tympanic membranes were normal. THE DIAGNOSIS Pure tone audiometry showed severe sensorineural hearing loss in the left ear and a poor speech discrimination score. The Weber test confirmed the hearing loss was sensorineu- ral and not conductive, ruling out a middle ear effusion. -

The Older Adult 20
CHAPTER The Older Adult 20 Older adults now number more than 25 million people in the United States and are expected to reach 80 million by 2050.1 These seniors will live longer than previous generations: life span at birth is currently 79 years for women and 74 years for men. Those older than 85 years are projected to increase to 5% of the U.S. population within 40 years. Hence, the “demographic im- perative” is to maximize not only the life span but also the “health span” of our older population, so that seniors maintain full function for as long as possible, enjoying rich and active lives in their homes and communities. Clinicians now recognize frailty as one of society’s common myths about aging—more than 95% of Americans older than 65 years live in the commu- nity, and only 5% reside in long-term care facilities.1,2 Over the past 20 years, seniors actually have become more active and less disabled. These changes call for new goals for clinical care—“an informed activated patient inter- acting with a prepared proactive team, resulting in high quality satisfying en- counters and improved outcomes”3—and a distinct set of clinical attitudes and skills. CHAPTER 20 I THE OLDER ADULT 839 ANATOMY AND PHYSIOLOGY Assessing the older adult presents special opportunities and special challenges. Many of these are quite different from the disease-oriented approach of his- tory taking and physical examination for younger patients: the focus on healthy or “successful” aging; the need to understand and mobilize family, social, and community supports; the importance of skills directed to func- tional assessment, “the sixth vital sign”; and the opportunities for promoting the older adult’s long-term health and safety. -

Monitoring Anesthetic Depth
ANESTHETIC MONITORING Lyon Lee DVM PhD DACVA MONITORING ANESTHETIC DEPTH • The central nervous system is progressively depressed under general anesthesia. • Different stages of anesthesia will accompany different physiological reflexes and responses (see table below, Guedel’s signs and stages). Table 1. Guedel’s (1937) Signs and Stages of Anesthesia based on ‘Ether’ anesthesia in cats. Stages Description 1 Inducement, excitement, pupils constricted, voluntary struggling Obtunded reflexes, pupil diameters start to dilate, still excited, 2 involuntary struggling 3 Planes There are three planes- light, medium, and deep More decreased reflexes, pupils constricted, brisk palpebral reflex, Light corneal reflex, absence of swallowing reflex, lacrimation still present, no involuntary muscle movement. Ideal plane for most invasive procedures, pupils dilated, loss of pain, Medium loss of palpebral reflex, corneal reflexes present. Respiratory depression, severe muscle relaxation, bradycardia, no Deep (early overdose) reflexes (palpebral, corneal), pupils dilated Very deep anesthesia. Respiration ceases, cardiovascular function 4 depresses and death ensues immediately. • Due to arrival of newer inhalation anesthetics and concurrent use of injectable anesthetics and neuromuscular blockers the above classic signs do not fit well in most circumstances. • Modern concept has two stages simply dividing it into ‘awake’ and ‘unconscious’. • One should recognize and familiarize the reflexes with different physiologic signs to avoid any untoward side effects and complications • The system must be continuously monitored, and not neglected in favor of other signs of anesthesia. • Take all the information into account, not just one sign of anesthetic depth. • A major problem faced by all anesthetists is to avoid both ‘too light’ anesthesia with the risk of sudden violent movement and the dangerous ‘too deep’ anesthesia stage. -

Bates' Pocket Guide to Physical Examination and History Taking
Lynn S. Bickley, MD, FACP Clinical Professor of Internal Medicine School of Medicine University of New Mexico Albuquerque, New Mexico Peter G. Szilagyi, MD, MPH Professor of Pediatrics Chief, Division of General Pediatrics University of Rochester School of Medicine and Dentistry Rochester, New York Acquisitions Editor: Elizabeth Nieginski/Susan Rhyner Product Manager: Annette Ferran Editorial Assistant: Ashley Fischer Design Coordinator: Joan Wendt Art Director, Illustration: Brett MacNaughton Manufacturing Coordinator: Karin Duffield Indexer: Angie Allen Prepress Vendor: Aptara, Inc. 7th Edition Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2009 by Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2007, 2004, 2000 by Lippincott Williams & Wilkins. Copyright © 1995, 1991 by J. B. Lippincott Company. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appear- ing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at Two Commerce Square, 2001 Market Street, Philadelphia PA 19103, via email at [email protected] or via website at lww.com (products and services). 9 8 7 6 5 4 3 2 1 Printed in China Library of Congress Cataloging-in-Publication Data Bickley, Lynn S. Bates’ pocket guide to physical examination and history taking / Lynn S. -

1- Assessing Pain
Foundations of Assessing and Treating Pain Assessing Pain Table of Contents Assessing Pain........................................................................................................................................2 Goal:..............................................................................................................................................2 After completing this module, participants will be able to:..............................................................2 Professional Practice Gaps............................................................................................................2 Introduction............................................................................................................................................. 2 Assessment and Diagnosis of Pain Case: Ms. Ward..........................................................................3 Confidentiality..........................................................................................................................................4 Pain History: A Standardized Approach..................................................................................................4 Evaluating Pain Using PQRSTU: Steps P, Q, R, S T, and U..............................................................5 Ms. Ward's Pain History (P, Q, R, S, T, U)..........................................................................................6 Video: Assessing Pain Systematically with PQRTSTU Acronym........................................................8 -

(June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION and WHY
DRAFT EVALUATION & MANAGEMENT DOCUMENTATION GUIDELINES (June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION AND WHY IS IT IMPORTANT? Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history including past and present illnesses, examinations, tests, treatments, and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high quality care. The medical record facilitates: · the ability of the physician and other health care professionals to evaluate and plan the patient's immediate treatment, and to monitor his/her health care over time. · communication and continuity of care among physicians and other health care professionals involved in the patient's care; · accurate and timely claims review and payment; · appropriate utilization review and quality of care evaluations; and · collection of data that may be useful for research and education. An appropriately documented medical record can reduce many of the "hassles" associated with claims processing and may serve as a legal document to verify the care provided, if necessary. WHAT DO PAYERS WANT AND WHY? Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate: · the site of service; · the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or · that services provided have been accurately reported. II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION The principles of documentation listed below are applicable to all types of medical and surgical Pg. 1 services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. -

Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019
Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019 Centers for Medicare & Medicaid Services PRA Disclosure Statement According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is x. The time required to complete this information collection is estimated to average 0.3 minutes per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. This estimate does not include time for training. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850. *****CMS Disclaimer*****Please do not send applications, claims, payments, medical records or any documents containing sensitive information to the PRA Reports Clearance Office. Please note that any correspondence not pertaining to the information collection burden approved under the associated OMB control number listed on this form will not be reviewed, forwarded, or retained. If you have questions or concerns regarding where to submit your documents, please contact Joan Proctor National Coordinator, Home Health Quality Reporting Program Centers for Medicare & Medicaid. OASIS-D Guidance Manual Table of Contents Page