Review of Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

Approach to Cyanosis in a Neonate.Pdf
PedsCases Podcast Scripts This podcast can be accessed at www.pedscases.com, Apple Podcasting, Spotify, or your favourite podcasting app. Approach to Cyanosis in a Neonate Developed by Michelle Fric and Dr. Georgeta Apostol for PedsCases.com. June 29, 2020 Introduction Hello, and welcome to this pedscases podcast on an approach to cyanosis in a neonate. My name is Michelle Fric and I am a fourth-year medical student at the University of Alberta. This podcast was made in collaboration with Dr. Georgeta Apostol, a general pediatrician at the Royal Alexandra Hospital Pediatrics Clinic in Edmonton, Alberta. Cyanosis refers to a bluish discoloration of the skin or mucous membranes and is a common finding in newborns. It is a clinical manifestation of the desaturation of arterial or capillary blood and may indicate serious hemodynamic instability. It is important to have an approach to cyanosis, as it can be your only sign of a life-threatening illness. The goal of this podcast is to develop this approach to a cyanotic newborn with a focus on these can’t miss diagnoses. After listening to this podcast, the learner should be able to: 1. Define cyanosis 2. Assess and recognize a cyanotic infant 3. Develop a differential diagnosis 4. Identify immediate investigations and management for a cyanotic infant Background Cyanosis can be further broken down into peripheral and central cyanosis. It is important to distinguish these as it can help you to formulate a differential diagnosis and identify cases that are life-threatening. Peripheral cyanosis affects the distal extremities resulting in blue color of the hands and feet, while the rest of the body remains pinkish and well perfused. -

Urinary Incontinence Embarrassing but Treatable 2015 Rev
This information provides a general overview on this topic and may not apply to Health Notes everyone. To find out if this information applies to you and to get more information on From Your Family Doctor this subject, talk to your family doctor. Urinary incontinence Embarrassing but treatable 2015 rev. What is urinary incontinence? Are there different types Urinary incontinence means that you can’t always of incontinence? control when you urinate, or pee. The amount of leakage Yes. There are five types of urinary incontinence. can be small—when you sneeze, cough, or laugh—or large, due to very strong urges to urinate that are hard to Stress incontinence is when urine leaks because of control. This can be embarrassing, but it can be treated. sudden pressure on your lower stomach muscles, such as when you cough, sneeze, laugh, rise from a Millions of adults in North America have urinary chair, lift something, or exercise. Stress incontinence incontinence. It’s most common in women over 50 years usually occurs when the pelvic muscles are weakened, of age, but it can also affect younger people, especially sometimes by childbirth, or by prostate or other pelvic women who have just given birth. surgery. Stress incontinence is common in women. Be sure to talk to your doctor if you have this problem. Urge incontinence is when the need to urinate comes on If you hide your incontinence, you risk getting rashes, too fast—before you can get to a toilet. Your body may only sores, and skin and urinary tract (bladder) infections. -

Abdominal Pain - Gastroesophageal Reflux Disease
ACS/ASE Medical Student Core Curriculum Abdominal Pain - Gastroesophageal Reflux Disease ABDOMINAL PAIN - GASTROESOPHAGEAL REFLUX DISEASE Epidemiology and Pathophysiology Gastroesophageal reflux disease (GERD) is one of the most commonly encountered benign foregut disorders. Approximately 20-40% of adults in the United States experience chronic GERD symptoms, and these rates are rising rapidly. GERD is the most common gastrointestinal-related disorder that is managed in outpatient primary care clinics. GERD is defined as a condition which develops when stomach contents reflux into the esophagus causing bothersome symptoms and/or complications. Mechanical failure of the antireflux mechanism is considered the cause of GERD. Mechanical failure can be secondary to functional defects of the lower esophageal sphincter or anatomic defects that result from a hiatal or paraesophageal hernia. These defects can include widening of the diaphragmatic hiatus, disturbance of the angle of His, loss of the gastroesophageal flap valve, displacement of lower esophageal sphincter into the chest, and/or failure of the phrenoesophageal membrane. Symptoms, however, can be accentuated by a variety of factors including dietary habits, eating behaviors, obesity, pregnancy, medications, delayed gastric emptying, altered esophageal mucosal resistance, and/or impaired esophageal clearance. Signs and Symptoms Typical GERD symptoms include heartburn, regurgitation, dysphagia, excessive eructation, and epigastric pain. Patients can also present with extra-esophageal symptoms including cough, hoarse voice, sore throat, and/or globus. GERD can present with a wide spectrum of disease severity ranging from mild, intermittent symptoms to severe, daily symptoms with associated esophageal and/or airway damage. For example, severe GERD can contribute to shortness of breath, worsening asthma, and/or recurrent aspiration pneumonia. -

Acute Abdomen
Acute abdomen: Shaking down the Acute abdominal pain can be difficult to diagnose, requiring astute assessment skills and knowledge of abdominal anatomy 2.3 ANCC to discover its cause. We show you how to quickly and accurately CONTACT HOURS uncover the clues so your patient can get the help he needs. By Amy Wisniewski, BSN, RN, CCM Lehigh Valley Home Care • Allentown, Pa. The author has disclosed that she has no significant relationships with or financial interest in any commercial companies that pertain to this educational activity. NIE0110_124_CEAbdomen.qxd:Deepak 26/11/09 9:38 AM Page 43 suspects Determining the cause of acute abdominal rapidly, indicating a life-threatening process, pain is often complex due to the many or- so fast and accurate assessment is essential. gans in the abdomen and the fact that pain In this article, I’ll describe how to assess a may be nonspecific. Acute abdomen is a patient with acute abdominal pain and inter- general diagnosis, typically referring to se- vene appropriately. vere abdominal pain that occurs suddenly over a short period (usually no longer than What a pain! 7 days) and often requires surgical interven- Acute abdominal pain is one of the top tion. Symptoms may be severe and progress three symptoms of patients presenting in www.NursingMadeIncrediblyEasy.com January/February 2010 Nursing made Incredibly Easy! 43 NIE0110_124_CEAbdomen.qxd:Deepak 26/11/09 9:38 AM Page 44 the ED. Reasons for acute abdominal pain Visceral pain can be divided into three Your patient’s fall into six broad categories: subtypes: age may give • inflammatory—may be a bacterial cause, • tension pain. -

Overactive Bladder
Overactive Bladder Introduction Symptoms You Might Notice “Overactive bladder” (OAB) or “unstable bladder” • A strong urge to urinate with little warning. refers to the feeling of needing to urinate much more • More frequent urination. often than is average. Since a medical name for the • Possible dribbling or loss of a large amount of urine. bladder muscle is the “detrusor,” you may also hear this • Difficulty postponing urination. This becomes a major condition called names like “detrusor overactivity” or issue for people with OAB, and can limit activities and “detrusor instability.” travel. OAB is a complex problem, but generally, the • Usually, no physical pain is associated with this bladder may contract/squeeze prematurely and hard problem, but it can be very emotionally and socially enough to make urine leak out before you can make it to disturbing. the bathroom. This type of urine loss is called “urge • Need to get up more than once at night to urinate. incontinence.” • Some people may experience an uncomfortable OAB can occur at any age. Some people are born sensation of urgency. with conditions that affect nerve and muscle signals, resulting in frequent urination, accidents, and bed Possible Causes Your Health Care Provider wetting in children. Other people may not develop OAB May Look For until they are older. The body and its muscles change • Usually no outward physical signs of OAB. with aging, making OAB quite common in older adults. • In older men, this type of bladder problem may be Additionally, certain disease processes or treatments associated with prostate enlargement. may change the bladder to be more sensitive, leading to • In older women, OAB may be related to skin, blood OAB symptoms. -

Review of Systems – Return Visit Have You Had Any Problems Related to the Following Symptoms in the Past Month? Circle Yes Or No
REVIEW OF SYSTEMS – RETURN VISIT HAVE YOU HAD ANY PROBLEMS RELATED TO THE FOLLOWING SYMPTOMS IN THE PAST MONTH? CIRCLE YES OR NO Today’s Date: ______________ Name: _______________________________ Date of Birth: __________________ GENERAL GENITOURINARY Fatigue Y N Blood in Urine Y N Fever / Chills Y N Menstrual Irregularity Y N Night Sweats Y N Painful Menstrual Cycle Y N Weight Gain Y N Vaginal Discharge Y N Weight Loss Y N Vaginal Dryness Y N EYES Vaginal Itching Y N Vision Changes Y N Painful Sex Y N EAR, NOSE, & THROAT SKIN Hearing Loss Y N Hair Loss Y N Runny Nose Y N New Skin Lesions Y N Ringing in Ears Y N Rash Y N Sinus Problem Y N Pigmentation Change Y N Sore Throat Y N NEUROLOGIC BREAST Headache Y N Breast Lump Y N Muscular Weakness Y N Tenderness Y N Tingling or Numbness Y N Nipple Discharge Y N Memory Difficulties Y N CARDIOVASCULAR MUSCULOSKELETAL Chest Pain Y N Back Pain Y N Swelling in Legs Y N Limitation of Motion Y N Palpitations Y N Joint Pain Y N Fainting Y N Muscle Pain Y N Irregular Heart Beat Y N ENDOCRINE RESPIRATORY Cold Intolerance Y N Cough Y N Heat Intolerance Y N Shortness of Breath Y N Excessive Thirst Y N Post Nasal Drip Y N Excessive Amount of Urine Y N Wheezing Y N PSYCHOLOGY GASTROINTESTINAL Difficulty Sleeping Y N Abdominal Pain Y N Depression Y N Constipation Y N Anxiety Y N Diarrhea Y N Suicidal Thoughts Y N Hemorrhoids Y N HEMATOLOGIC / LYMPHATIC Nausea Y N Easy Bruising Y N Vomiting Y N Easy Bleeding Y N GENITOURINARY Swollen Lymph Glands Y N Burning with Urination Y N ALLERGY / IMMUNOLOGY Urinary -
Urinary System
Urinary system Urinary system terms Nephr/o, Kidney Nephritis, renal artery ren/o Hydronephrosis (abnormal condition involving back Hydro/o Water up of urine into the kidney Cystitis, cystectomy (inflammation of, removal of Cyst/o Bladder bladder) Pyel/o Renal collecting ducts Pyelogram (X-ray of the collecting ducts) Polyuria, anuria (frequent urination, no urine Ur/o, -uria Urine formation) Olig/o Scanty, less than normal Oliguria (reduced urine formation) To surgically reattach, fix in Nephropexy (surgically attach kidney in normal -pexy normal position anatomical position) Urinary system diseases Nephrosis – a noninflammatory disease of kidneys. Nephrolith – a kidney stone. Urethritis – inflammation of the urethra, the final pathway for urine in both sexes, and the common pathway for urine and semen in the male. Nocturia – frequently getting up and urinating during the night. Enuresis – involuntary release of urine, most often in reference to “bedwetting.” Urinary system procedures Nephrologist – I am hoping by now, you would know this is a physician specializing in kidney diseases. Urologist – a physician specializing in the genitourinary tract, which includes kidneys, urinary bladder and urethra of both men and women and the prostate and testes in men. Cystoscopy – looking into the urinary bladder with a fiberoptic instrument. Intravenous pyelogram – special X-rays showing the drainage pattern of the kidneys. A dye opaque to X-rays is injected into a vein. After a waiting period for the blood and dye to pass through the kidneys, X-rays can be taken of the collecting system of the kidney, ureter and bladder. Retrograde pyelogram – personally, I prefer the former procedure! In this procedure a dye opaque to X-rays is flushed backwards up the urethra and bladder and up the ureters to the kidneys. -

Frequently Asked Questions About Overactive Bladder
ABOUT OAB Frequently Asked Questions about Overactive Bladder What is Overactive Bladder (OAB)? If you live with OAB, you may also: Overactive Bladder (OAB) isn’t a disease. It’s the u Leak urine (incontinence): Sometimes people name of a group of urinary symptoms. The most with OAB also have “urgency incontinence.” common symptom of OAB is a sudden urge to This means that urine leaks when you feel urinate that you can’t control. Some people will the sudden urge to go. This isn’t the same as leak urine when they feel this urge. Having to “stress urinary incontinence” or “SUI.” People urinate many times during the day and night is with SUI leak urine while sneezing, laughing or another symptom of OAB. doing other physical activities. (You can learn more about SUI at UrologyHealth.org/SUI.) How common is OAB? u Urinate frequently: You may also need to go OAB is common. It affects millions of Americans. to the bathroom many times during the day. As many as 30 percent of men and 40 percent The number of times someone urinates varies of women in the United States live with OAB from person to person. But many experts symptoms. agree that going to the bathroom more than eight times in 24 hours is “frequent urination.” Who is at risk for OAB? u Wake up at night to urinate: Waking from As you grow older, you’re at higher risk for sleep to go to the bathroom more than once a OAB. But no matter what your age, there are night is another symptom of OAB. -

Chilaiditi's Syndrome Complicated by Colon Perforation
CASE REPORT Chilaiditi’s syndrome complicated by colon perforation: a case report Turan Acar, M.D., Erdinç Kamer, M.D., Nihan Acar, M.D., Ahmet Er, M.D., Mustafa Peşkersoy, M.D. Department of Surgery, Izmir Katip Celebi University Ataturk Training and Research Hospital, Izmir ABSTRACT Hepatodiaphragmatic interposition of the small or large intestine is known as Chilaiditi syndrome, whichis a rare disease diagnosed incidentally. Chilaiditi syndrome is typically asymptomatic, but it can be associated with symptoms ranging from intermittent, mild ab- dominal pain to acute intestinal obstruction, constipation, chest pain and breathlessness. A 54-year-old male patient was admitted to the hospital with a history of abdominal pain, nausea and vomiting. Chest X-ray revealed an elevation of the right hemidiaphragma caused by the presence of a dilated colonic loop below. The patient underwent urgent surgery with perforation as preliminary diagnosis. The pa- tient underwent right hemicolectomy and ileocolic anastomosis because of the intestinal obstruction related to Chilaiditi’s Syndrome. Due to the rarity of this syndrome and typical radiological findings, this case was aimed to be presented. Key words: Abdominal pain; Chilaiditi’s syndrome; surgery. INTRODUCTION CASE REPORT Interposition of the bowel (usually transverse colon or he- A 54-year-oldmale patient was admitted to the Emergency patic flexura) or the small intestine between the liver and Department of Surgery, Izmir Katip Celebi University Ataturk diaphragm, which is a rare anomaly, was first defined by the Training and Research Hospital with a 24-hour history of right Greek radiologist Demetrius Chilaiditi in 1910.[1,2] It is inci- upper abdominal pain, nausea and vomiting. -
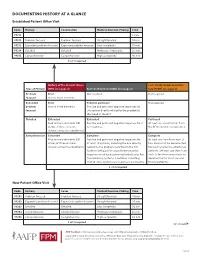
Documenting History at a Glance
DOCUMENTING HISTORY AT A GLANCE Established Patient Office Visit Code History Examination Medical Decision-Making Time 99211 — — — 5 min. 99212 Problem focused Problem focused Straightforward 10 min. 99213 Expanded problem focused Expanded problem focused Low complexity 15 min. 99214 Detailed Detailed Moderate complexity 25 min. 99215 Comprehensive Comprehensive High complexity 40 min. 2 of 3 required History of the Present Illness Past, Family and/or Social His- Type of History (HPI) (see page 2) Review of Systems (ROS) (see page 2) tory (PFSH) (see page 2) Problem Brief Not required Not required focused One to three elements Expanded Brief Problem pertinent Not required problem One to three elements Positive and pertinent negative responses for focused the system directly related to the problem(s) identified in the HPI. Detailed Extended Extended Pertinent Four or more elements (OR Positive and pertinent negative responses for 2 At least one specific item from status of three or more to 9 systems. the PFSH must be documented. chronic or inactive conditions) Comprehensive Extended Complete Complete Four or more elements (OR Positive and pertinent negative responses for At least one item from each of status of three or more at least 10 systems, including the one directly two areas must be documented chronic or inactive conditions) related to the problem identified in the HPI. for most services to established Systems with positive or pertinent negative patients. (At least one item from responses must be documented individually. For each of the three areas must be the remaining systems, a notation indicating documented for most services that all other systems are negative is permissible.