Gotta Gotta Go Right Now: a Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Healthy Toileting Practices
Healthy Toileting Practices Bowel movements: Start a toilet time routine. Choose a specific time during the day when your child will sit on the toilet to pass a bowel movement (make a poop) and have them use the toilet at the same time every day. The body is usually ready for a bowel movement 20-30 minutes after eating, so a good time to try would be after breakfast, lunch, or dinner. Your child’s stool (poop) should be soft and easy to pass, and look like a snake or sausage. To help your child have regular bowel movements, they should eat fruits and vegetables, and drink plenty of water. If your child is constipated they will be unable to have a bowel movement or have painful and difficult bowel movements. Please call us with any questions or concerns about constipation. Hygiene and proper cleaning are important. Please remember to wipe from “front to back”. Urination: Remind your child to sit on the toilet AT LEAST every 3 hours, or more often if they need to. Give your child enough time to sit on the toilet and try to urinate (pee). Remind your child not to rush while they urinate. Ask your child to breathe deeply and take their time when trying to urinate to relax the pelvic floor (no squeezing or pushing with the tummy). Ask them to take deep breaths and blow out the air slowly to help them relax. Double voiding: Try to have your child urinate. After your child urinates and says they are “finished”, wipe them from front to back and ask them to stand up and move around and then sit back down on the toilet and try again. -

Leave No Trace Outdoor Skills & Ethics
ISLE ROYALE NATIONAL PARK Leave No Trace Outdoor Skills & Ethics Leave No Trace Outdoor Skills and Ethics ISLE ROYALE NATIONAL PARK Leave No Trace Center for Outdoor Ethics November, 2004 Leave No Trace — Isle Royale National Park Skills & Ethics 1 Wildland Ethics "Ethical and moral questions and how we answer them may determine whether primal scenes will continue to be a source of joy and comfort to future generations. The decisions are ours and we have to search our minds and souls for the right answers..." "The real significance of wilderness is a cultural matter. It is far more than hunting, fishing, hiking, camping or canoeing; it has to do with the human spirit." —Sigurd F. Olson ...and so we visit wild places to discover ourselves, to let our spirits run with the graceful canoe and journey through the beckoning forests. The wilderness is good for us. It enables us to discover who we really are, and to explore who we are really meant to be. It is the nature of wild places that gives us the space to slow the pace of our lives, to becalm the storms of everyday life, to gain perspective on the things we truly value. Sigurd Olson needed wild places...they gave much to him, as they do to us—and, so, we should be eager to give back. Our favorite places— those whose forests have welcomed us, whose lakes have refreshed us, whose sunsets have inspired awe—are not ours alone. They are a treasured resource, there for the good of all who seek their own true spirit through solitude and adventure. -

Urinary Incontinence Embarrassing but Treatable 2015 Rev
This information provides a general overview on this topic and may not apply to Health Notes everyone. To find out if this information applies to you and to get more information on From Your Family Doctor this subject, talk to your family doctor. Urinary incontinence Embarrassing but treatable 2015 rev. What is urinary incontinence? Are there different types Urinary incontinence means that you can’t always of incontinence? control when you urinate, or pee. The amount of leakage Yes. There are five types of urinary incontinence. can be small—when you sneeze, cough, or laugh—or large, due to very strong urges to urinate that are hard to Stress incontinence is when urine leaks because of control. This can be embarrassing, but it can be treated. sudden pressure on your lower stomach muscles, such as when you cough, sneeze, laugh, rise from a Millions of adults in North America have urinary chair, lift something, or exercise. Stress incontinence incontinence. It’s most common in women over 50 years usually occurs when the pelvic muscles are weakened, of age, but it can also affect younger people, especially sometimes by childbirth, or by prostate or other pelvic women who have just given birth. surgery. Stress incontinence is common in women. Be sure to talk to your doctor if you have this problem. Urge incontinence is when the need to urinate comes on If you hide your incontinence, you risk getting rashes, too fast—before you can get to a toilet. Your body may only sores, and skin and urinary tract (bladder) infections. -

A Concept of Clean Toilet from the Islamic Perspective
A CONCEPT OF CLEAN TOILET FROM THE ISLAMIC PERSPECTIVE Asiah Abdul Rahim Department ofArchitecture Kulliyyah afArchitecture and Environmental Design INTERNATIONAL ISLAMIC UNIVERSITY MALAYSIA Abstract Islam is the official religion of Malaysia and more than half of the population is Muslim. As Muslims, the aspect of cleanliness is one of the most important and basic things that should be followed and practised in everyday life. Allah loves those cleanse themselves as quoted in the holy Qur'an. .. God loves those who turn to Him, and He loves those who cleanse themselves ". (Surah Al-Baqarah: 222) There is a growing awareness of public toilets among the public and authorities which can be seen in the events such as the "A Clean Toilet Campaign Seminar" held at national level end of July 2003 in lohor Bahru, Johor. Criticisms by visitors and locals stirred the level of consciousness among those responsible directly or indirectly for clean and effective public facilities.Nowadays, toilet is no longer perceived as merely a small and insignificant part of a building. It contributes and serves more than the initial purposes intended. Due to socio-economic changes, a toilet has been diversified and become multi-functions. It has surpassed its traditional role as a place to empty bowels or urinates to serve as comfortable vicinity with conveniences. In developed countries such as Japan and Korea, a public toilet has become a communal area where people could do face washing, showering, freshen up or taking care of their kids and so on. In designing a public toilet, some elements should be highlighted particularly on the understanding of users needs. -

Caring for Your Bladder After Out-Patient Surgery at Von Voigtlander Women’S Hospital
Caring for Your Bladder after Out-Patient Surgery at Von Voigtlander Women’s Hospital Sometimes, surgery and pain medicine (anesthetics) can affect your bladder for several hours. This information will help you care for your bladder after surgery. How does surgery affect my bladder? If you were pregnant, your bladder may have already lost some of its tone. There can be some temporary nerve issues after surgery, which decrease your sensation (the feeling that you need to urinate). Temporary swelling after surgery can also affect your urination. If urine remains in the bladder after urinating, it can cause stretching of the bladder. It can also cause damage to the muscles of the bladder. This can lead to permanent bladder injury. What do I need to watch for? The following signs and symptoms may indicate a bladder problem. Trouble starting to void, or urinate, especially after surgery. Feeling like you bladder is not empty after urinating. Dribbling, or leaking urine after urination. Needing to urinate often, but only urinating small amounts. Needing to strain to start a stream of urine. Needing to go often through the night. Feeling of fullness in your lower abdomen. You may not have any symptoms at all. If you feel any of the above symptoms, or if you suspect that you might have a problem with your bladder before you are discharged, call the nurse. Department of Obstetrics and Gynecology - 1 - What can I do to avoid problems? Try to urinate at least every 2 to 3 hours If you cannot urinate immediately after surgery, tell your nurse. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Urinary Tract Infections What Is a UTI?
Urinary Tract Infections What is a UTI? Bacteria that cause urinary tract infections are often spread from the rectal/anal area to the urethra and then into the bladder or kidneys. These bacteria can cause: Cystitis (bladder infection) Pyelonephritis (kidney infection) Urethritis (inflammation of the urethra, the tube that drains urine from the bladder) Urethral syndrome (painful urination without evidence of bacterial infection in the urine) Who are at risk for UTIs? Women are more likely to develop UTIs because their urethras are short, making it easy for bacteria to spread to the bladder. UTIs are more likely to occur in women who: Are newly sexually active or have a new sexual partner Are past menopause Are pregnant Have a history of diabetes, sickle-cell anemia, stroke, kidney stones, or any illness that causes the bladder to be paralyzed or to fail to empty completely Signs and symptoms of UTIs Pain and/or burning with urination Urgency or frequency of urination Blood or pus in urine Strong smelling urine Pain in lower pelvis, stomach, lower back, or on sides just above waist level Pain during sexual intercourse Chills, fever, fatigue, nausea or vomiting Urinating frequently during the night Diagnosing UTIs Laboratory analysis of urine (called a UA or Urine Analysis) Personal history of signs and symptoms Physical exam including a pelvic exam, if necessary For person who suffers from frequent UTIs, further testing is usually ordered Treatment Antibiotics for 3-10 days depending on severity of infection Increasing water and juice intake to more than 8 eight oz. glasses per day Tylenol or aspirin for fever and backache o See a doctor if fever is over 100 degrees Heating pad or hot water bottle applied to lower abdomen or back How can I help prevent a UTI? After a bowel movement (BM), wipe yourself from front to back to prevent germs in the stool from getting near your urethra. -

Overactive Bladder
Overactive Bladder Introduction Symptoms You Might Notice “Overactive bladder” (OAB) or “unstable bladder” • A strong urge to urinate with little warning. refers to the feeling of needing to urinate much more • More frequent urination. often than is average. Since a medical name for the • Possible dribbling or loss of a large amount of urine. bladder muscle is the “detrusor,” you may also hear this • Difficulty postponing urination. This becomes a major condition called names like “detrusor overactivity” or issue for people with OAB, and can limit activities and “detrusor instability.” travel. OAB is a complex problem, but generally, the • Usually, no physical pain is associated with this bladder may contract/squeeze prematurely and hard problem, but it can be very emotionally and socially enough to make urine leak out before you can make it to disturbing. the bathroom. This type of urine loss is called “urge • Need to get up more than once at night to urinate. incontinence.” • Some people may experience an uncomfortable OAB can occur at any age. Some people are born sensation of urgency. with conditions that affect nerve and muscle signals, resulting in frequent urination, accidents, and bed Possible Causes Your Health Care Provider wetting in children. Other people may not develop OAB May Look For until they are older. The body and its muscles change • Usually no outward physical signs of OAB. with aging, making OAB quite common in older adults. • In older men, this type of bladder problem may be Additionally, certain disease processes or treatments associated with prostate enlargement. may change the bladder to be more sensitive, leading to • In older women, OAB may be related to skin, blood OAB symptoms. -
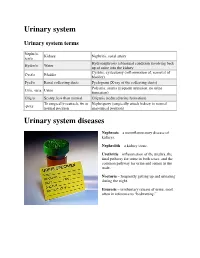
Urinary System
Urinary system Urinary system terms Nephr/o, Kidney Nephritis, renal artery ren/o Hydronephrosis (abnormal condition involving back Hydro/o Water up of urine into the kidney Cystitis, cystectomy (inflammation of, removal of Cyst/o Bladder bladder) Pyel/o Renal collecting ducts Pyelogram (X-ray of the collecting ducts) Polyuria, anuria (frequent urination, no urine Ur/o, -uria Urine formation) Olig/o Scanty, less than normal Oliguria (reduced urine formation) To surgically reattach, fix in Nephropexy (surgically attach kidney in normal -pexy normal position anatomical position) Urinary system diseases Nephrosis – a noninflammatory disease of kidneys. Nephrolith – a kidney stone. Urethritis – inflammation of the urethra, the final pathway for urine in both sexes, and the common pathway for urine and semen in the male. Nocturia – frequently getting up and urinating during the night. Enuresis – involuntary release of urine, most often in reference to “bedwetting.” Urinary system procedures Nephrologist – I am hoping by now, you would know this is a physician specializing in kidney diseases. Urologist – a physician specializing in the genitourinary tract, which includes kidneys, urinary bladder and urethra of both men and women and the prostate and testes in men. Cystoscopy – looking into the urinary bladder with a fiberoptic instrument. Intravenous pyelogram – special X-rays showing the drainage pattern of the kidneys. A dye opaque to X-rays is injected into a vein. After a waiting period for the blood and dye to pass through the kidneys, X-rays can be taken of the collecting system of the kidney, ureter and bladder. Retrograde pyelogram – personally, I prefer the former procedure! In this procedure a dye opaque to X-rays is flushed backwards up the urethra and bladder and up the ureters to the kidneys. -

Toileting Behaviors Related to Urination in Women: a Scoping Review
International Journal of Environmental Research and Public Health Review Toileting Behaviors Related to Urination in Women: A Scoping Review Chen Wu 1 , Kaikai Xue 2 and Mary H. Palmer 1,* 1 School of Nursing, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 2 School of Nursing, Xuzhou Medical University, Xuzhou 221000, China; [email protected] * Correspondence: [email protected] Received: 17 September 2019; Accepted: 17 October 2019; Published: 19 October 2019 Abstract: This scoping review explores the state of science regarding women’s toileting behaviors, gaps in knowledge, and areas for future research. Online databases were searched to identify papers published in English between January 2010 through July 2019; the search identified 25 articles. The Toileting Behaviors–Women’s Elimination Behaviors scale has been published in four validated language versions and used in 17 of the 25 studies. The most frequent behaviors include concern about public toilet cleanliness, delaying urination when busy or away from home, and using different toileting postures at and away from home. Determinants of toileting behaviors include environmental factors, chronic health conditions, and cognitive/psychological factors. Associations were found between toileting behaviors and lower urinary tract symptoms and between toileting postures and uroflowmetric parameters and post-void residual volume. Strategies that address modifiable determinants of toileting behaviors should be developed and tested in future research. Furthermore, little is known about the toileting behaviors and bladder health in older women and women from developing countries. Rigorous studies are needed to better understand the underlying mechanisms of toileting behaviors, the nature of associations between toileting behaviors and lower urinary tract symptoms, and effects of the environment on women’s toileting behaviors. -

Frequently Asked Questions About Overactive Bladder
ABOUT OAB Frequently Asked Questions about Overactive Bladder What is Overactive Bladder (OAB)? If you live with OAB, you may also: Overactive Bladder (OAB) isn’t a disease. It’s the u Leak urine (incontinence): Sometimes people name of a group of urinary symptoms. The most with OAB also have “urgency incontinence.” common symptom of OAB is a sudden urge to This means that urine leaks when you feel urinate that you can’t control. Some people will the sudden urge to go. This isn’t the same as leak urine when they feel this urge. Having to “stress urinary incontinence” or “SUI.” People urinate many times during the day and night is with SUI leak urine while sneezing, laughing or another symptom of OAB. doing other physical activities. (You can learn more about SUI at UrologyHealth.org/SUI.) How common is OAB? u Urinate frequently: You may also need to go OAB is common. It affects millions of Americans. to the bathroom many times during the day. As many as 30 percent of men and 40 percent The number of times someone urinates varies of women in the United States live with OAB from person to person. But many experts symptoms. agree that going to the bathroom more than eight times in 24 hours is “frequent urination.” Who is at risk for OAB? u Wake up at night to urinate: Waking from As you grow older, you’re at higher risk for sleep to go to the bathroom more than once a OAB. But no matter what your age, there are night is another symptom of OAB. -

Technology Review of Urine-Diverting Dry Toilets (Uddts) Overview of Design, Operation, Management and Costs
Technology Review of Urine-diverting dry toilets (UDDTs) Overview of design, operation, management and costs As a federally owned enterprise, we support the German Government in achieving its objectives in the field of international cooperation for sustainable development. Published by: Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ) GmbH Registered offices Bonn and Eschborn, Germany T +49 228 44 60-0 (Bonn) T +49 61 96 79-0 (Eschborn) Friedrich-Ebert-Allee 40 53113 Bonn, Germany T +49 228 44 60-0 F +49 228 44 60-17 66 Dag-Hammarskjöld-Weg 1-5 65760 Eschborn, Germany T +49 61 96 79-0 F +49 61 96 79-11 15 E [email protected] I www.giz.de Name of sector project: SV Nachhaltige Sanitärversorgung / Sustainable Sanitation Program Authors: Christian Rieck (GIZ), Dr. Elisabeth von Münch (Ostella), Dr. Heike Hoffmann (AKUT Peru) Editor: Christian Rieck (GIZ) Acknowledgements: We thank all reviewers who have provided substantial inputs namely Chris Buckley, Paul Calvert, Chris Canaday, Linus Dagerskog, Madeleine Fogde, Robert Gensch, Florian Klingel, Elke Müllegger, Charles Niwagaba, Lukas Ulrich, Claudia Wendland and Martina Winker, Trevor Surridge and Anthony Guadagni. We also received useful feedback from David Crosweller, Antoine Delepière, Abdoulaye Fall, Teddy Gounden, Richard Holden, Kamara Innocent, Peter Morgan, Andrea Pain, James Raude, Elmer Sayre, Dorothee Spuhler, Kim Andersson and Moses Wakala. The SuSanA discussion forum was also a source of inspiration: http://forum.susana.org/forum/categories/34-urine-diversion-systems-