Urinary Incontinence Embarrassing but Treatable 2015 Rev
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urinary Incontinence
GLICKMAN UROLOGICAL & KIDNEY INSTITUTE Urinary Incontinence What is it? can lead to incontinence, as can prostate cancer surgery or Urinary incontinence is the inability to control when you radiation treatments. Sometimes the cause of incontinence pass urine. It’s a common medical problem. As many as isn’t clear. 20 million Americans suffer from loss of bladder control. The condition is more common as men get older, but it’s Where can I get help? not an inevitable part of aging. Often, embarrassment stops Talking to your doctor is the first step. You shouldn’t feel men from seeking help, even when the problem is severe ashamed; physicians regularly help patients with this prob- and affects their ability to leave the house, spend time with lem and are comfortable talking about it. Many patients family and friends or take part in everyday activities. It’s can be evaluated and treated after a simple office visit. possible to cure or significantly improve urinary inconti- Some patients may require additional diagnostic tests, nence, once its underlying cause has been identified. But which can be done in an outpatient setting and aren’t pain- it’s important to remember that incontinence is a symp- ful. Once these tests have determined the cause of your tom, not a disease. Its cause can be complex and involve incontinence, your doctor can recommend specific treat- many factors. Your doctor should do an in-depth evaluation ments, many of which do not require surgery. No matter before starting treatment. how serious the problem seems, urinary incontinence is a condition that can be significantly relieved and, in many What might be causing my incontinence? cases, cured. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Overactive Bladder
Overactive Bladder Introduction Symptoms You Might Notice “Overactive bladder” (OAB) or “unstable bladder” • A strong urge to urinate with little warning. refers to the feeling of needing to urinate much more • More frequent urination. often than is average. Since a medical name for the • Possible dribbling or loss of a large amount of urine. bladder muscle is the “detrusor,” you may also hear this • Difficulty postponing urination. This becomes a major condition called names like “detrusor overactivity” or issue for people with OAB, and can limit activities and “detrusor instability.” travel. OAB is a complex problem, but generally, the • Usually, no physical pain is associated with this bladder may contract/squeeze prematurely and hard problem, but it can be very emotionally and socially enough to make urine leak out before you can make it to disturbing. the bathroom. This type of urine loss is called “urge • Need to get up more than once at night to urinate. incontinence.” • Some people may experience an uncomfortable OAB can occur at any age. Some people are born sensation of urgency. with conditions that affect nerve and muscle signals, resulting in frequent urination, accidents, and bed Possible Causes Your Health Care Provider wetting in children. Other people may not develop OAB May Look For until they are older. The body and its muscles change • Usually no outward physical signs of OAB. with aging, making OAB quite common in older adults. • In older men, this type of bladder problem may be Additionally, certain disease processes or treatments associated with prostate enlargement. may change the bladder to be more sensitive, leading to • In older women, OAB may be related to skin, blood OAB symptoms. -
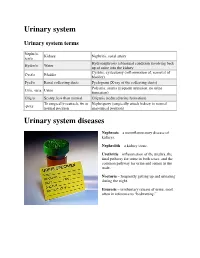
Urinary System
Urinary system Urinary system terms Nephr/o, Kidney Nephritis, renal artery ren/o Hydronephrosis (abnormal condition involving back Hydro/o Water up of urine into the kidney Cystitis, cystectomy (inflammation of, removal of Cyst/o Bladder bladder) Pyel/o Renal collecting ducts Pyelogram (X-ray of the collecting ducts) Polyuria, anuria (frequent urination, no urine Ur/o, -uria Urine formation) Olig/o Scanty, less than normal Oliguria (reduced urine formation) To surgically reattach, fix in Nephropexy (surgically attach kidney in normal -pexy normal position anatomical position) Urinary system diseases Nephrosis – a noninflammatory disease of kidneys. Nephrolith – a kidney stone. Urethritis – inflammation of the urethra, the final pathway for urine in both sexes, and the common pathway for urine and semen in the male. Nocturia – frequently getting up and urinating during the night. Enuresis – involuntary release of urine, most often in reference to “bedwetting.” Urinary system procedures Nephrologist – I am hoping by now, you would know this is a physician specializing in kidney diseases. Urologist – a physician specializing in the genitourinary tract, which includes kidneys, urinary bladder and urethra of both men and women and the prostate and testes in men. Cystoscopy – looking into the urinary bladder with a fiberoptic instrument. Intravenous pyelogram – special X-rays showing the drainage pattern of the kidneys. A dye opaque to X-rays is injected into a vein. After a waiting period for the blood and dye to pass through the kidneys, X-rays can be taken of the collecting system of the kidney, ureter and bladder. Retrograde pyelogram – personally, I prefer the former procedure! In this procedure a dye opaque to X-rays is flushed backwards up the urethra and bladder and up the ureters to the kidneys. -

Frequently Asked Questions About Overactive Bladder
ABOUT OAB Frequently Asked Questions about Overactive Bladder What is Overactive Bladder (OAB)? If you live with OAB, you may also: Overactive Bladder (OAB) isn’t a disease. It’s the u Leak urine (incontinence): Sometimes people name of a group of urinary symptoms. The most with OAB also have “urgency incontinence.” common symptom of OAB is a sudden urge to This means that urine leaks when you feel urinate that you can’t control. Some people will the sudden urge to go. This isn’t the same as leak urine when they feel this urge. Having to “stress urinary incontinence” or “SUI.” People urinate many times during the day and night is with SUI leak urine while sneezing, laughing or another symptom of OAB. doing other physical activities. (You can learn more about SUI at UrologyHealth.org/SUI.) How common is OAB? u Urinate frequently: You may also need to go OAB is common. It affects millions of Americans. to the bathroom many times during the day. As many as 30 percent of men and 40 percent The number of times someone urinates varies of women in the United States live with OAB from person to person. But many experts symptoms. agree that going to the bathroom more than eight times in 24 hours is “frequent urination.” Who is at risk for OAB? u Wake up at night to urinate: Waking from As you grow older, you’re at higher risk for sleep to go to the bathroom more than once a OAB. But no matter what your age, there are night is another symptom of OAB. -

Diagnosis and Management of Urinary Incontinence in Childhood
Committee 9 Diagnosis and Management of Urinary Incontinence in Childhood Chairman S. TEKGUL (Turkey) Members R. JM NIJMAN (The Netherlands), P. H OEBEKE (Belgium), D. CANNING (USA), W.BOWER (Hong-Kong), A. VON GONTARD (Germany) 701 CONTENTS E. NEUROGENIC DETRUSOR A. INTRODUCTION SPHINCTER DYSFUNCTION B. EVALUATION IN CHILDREN F. SURGICAL MANAGEMENT WHO WET C. NOCTURNAL ENURESIS G. PSYCHOLOGICAL ASPECTS OF URINARY INCONTINENCE AND ENURESIS IN CHILDREN D. DAY AND NIGHTTIME INCONTINENCE 702 Diagnosis and Management of Urinary Incontinence in Childhood S. TEKGUL, R. JM NIJMAN, P. HOEBEKE, D. CANNING, W.BOWER, A. VON GONTARD In newborns the bladder has been traditionally described as “uninhibited”, and it has been assumed A. INTRODUCTION that micturition occurs automatically by a simple spinal cord reflex, with little or no mediation by the higher neural centres. However, studies have indicated that In this chapter the diagnostic and treatment modalities even in full-term foetuses and newborns, micturition of urinary incontinence in childhood will be discussed. is modulated by higher centres and the previous notion In order to understand the pathophysiology of the that voiding is spontaneous and mediated by a simple most frequently encountered problems in children the spinal reflex is an oversimplification [3]. Foetal normal development of bladder and sphincter control micturition seems to be a behavioural state-dependent will be discussed. event: intrauterine micturition is not randomly distributed between sleep and arousal, but occurs The underlying pathophysiology will be outlined and almost exclusively while the foetus is awake [3]. the specific investigations for children will be discussed. For general information on epidemiology and During the last trimester the intra-uterine urine urodynamic investigations the respective chapters production is much higher than in the postnatal period are to be consulted. -

Gotta Gotta Go Right Now: a Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis
Gotta Go Right Now: A Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis Kelly Haack, M.A., and William J. Warzak, Ph.D. Department of Psychology, Munroe-Meyer Institute at the University of Nebraska Medical Center INTRODUCTION METHOD RESULTS Participant Bartter’s Syndrome Baseline 2 Months Following BRT ¾ Bartter’s Syndrome is caused by a defect in the kidney’s ¾ The participant was a 14-year-old male with Bartter’s Syndrome. Fluid Intake and Output Fluid Intake and Output ability to reabsorb potassium. ¾ He presented with frequent daytime and nighttime voiding. 1000 1000 ¾ As a result, the kidneys remove too much potassium from ¾ Medical History: 900 900 the body. 4 years old: Renal Ultrasound showed normal kidneys and 800 800 ¾ Excessive loss of potassium leads to muscle cramping and hypokalemia (low potassium level) was ruled out. Intake weakness, constipation, increased frequency of urination, 700 700 Intake and growth failure. 11 years old: Ditropan XL 10 mg daily and Imipramine 35 mg 600 600 daily were prescribed to treat symptoms of overactive bladder, Nocturnal Enuresis 500 500 ML such as frequent urination. ML ¾ Nocturnal Enuresis is involuntary passing of urine while 12 years old: Neurological exam was normal and neurogenic 400 400 asleep. bladder was ruled out. 300 300 Output Bartter’s Syndrome Output • Continued taking Ditropan and Imipramine. 200 200 and • Prescribed DDAVP 0.6 mg each evening to increase urine 100 100 concentration and decrease urine production. Nocturnal Enuresis 0 0 ¾ Adolescents with Bartter’s Syndrome often have a problem • Started use of a urine alarm; however, it was a short trial and 3:00 6:00 7:45 9:45 1:00 2:30 4:00 5:00 6:20 8:00 9:30 1:00 2:45 5:00 7:00 9:00 2:00 4:00 5:00 7:00 9:00 1:45 4:00 7:00 4:00 7:05 9:45 2:00 4:00 5:45 7:00 9:30 2:30 5:00 7:45 2:30 4:30 7:00 9:30 1:45 5:00 12:00 11:00 11:00 10:45 12:00 10:00 12:00 concentrating urine and excrete an excessive volume of he slept through it and continued to wet 5 out of 7 nights. -
Urinary Tract Infections
Urinary Tract Infections www.kidney.org Did you know that... n Urinary tract infections (UTIs) are responsible for nearly 10 million doctor visits each year. n One in five women will have at least one UTI in her lifetime. Nearly 20 percent of women who have a UTI will have another, and 30 percent of those will have yet another. Of this last group, 80 percent will have recurrences. n About 80 to 90 percent of UTIs are caused by a single type of bacteria. 2 NATIONAL KIDNEY FOUNDATION n UTIs can be treated effectively with medications called antibiotics. n People who get repeated UTIs may need additional tests to check for other health problems. n UTIs also may be called cystitis or a bladder infection. This brochure answers the questions most often asked about UTIs. If you have more questions, speak to your doctor. What is a urinary tract infection? A urinary tract infection is what happens when bacteria (germs) get into the urinary tract (the bladder) and multiply. The result is redness, swelling and pain in the urinary tract (see diagram). WWW.KIDNEY.ORG 3 Most UTIs stay in the bladder, the pouch-shaped organ where urine is stored before it passes out of the body. If a UTI is not treated promptly, the bacteria can travel up to the kidneys and cause a more serious type of infection, called pyelonephritis (pronounced pie-low-nef-right- iss). Pyelonephritis is an actual infection of the kidney, where urine is produced. This may result in fever and back pain. What causes a UTI? About 80 to 90 percent of UTIs are caused by a type of bacteria, called E. -

FDA CVM Comprehensive ADE Report Listing for Afoxolaner
CVM ADE Comprehensive Clinical Detail Report Listing Cumulative Date Range : 04-Sep-2013 -thru- 31-Jul-2018 Included 1932a cases = : True Included Medicated Feed cases = : False DRUG: AFOXOLANER Species: Cat Route of Administration: oral Sign: VOMITING, Number of times reported: 4 Sign: HYPERACTIVITY, Number of times reported: 3 Sign: ITCHING, Number of times reported: 3 Sign: LETHARGY, Number of times reported: 3 Sign: PRURITUS, Number of times reported: 3 Sign: ACCIDENTAL EXPOSURE, Number of times reported: 2 Sign: ANOREXIA, Number of times reported: 2 Sign: LABOURED BREATHING, Number of times reported: 2 Sign: NOT EATING, Number of times reported: 2 Sign: PANTING, Number of times reported: 2 Sign: SEIZURE NOS, Number of times reported: 2 Sign: ABNORMAL TEST RESULT, Number of times reported: 1 Sign: AGITATION, Number of times reported: 1 Sign: ALOPECIA, Number of times reported: 1 Sign: ANAEMIA NOS, Number of times reported: 1 Sign: ATAXIA, Number of times reported: 1 Sign: CERVICAL VENTROFLEXION, Number of times reported: 1 Sign: CONSTIPATION, Number of times reported: 1 Sign: DECREASED CHOLESTEROL (TOTAL), Number of times reported: 1 Sign: ELEVATED ALT, Number of times reported: 1 Sign: ELEVATED AST, Number of times reported: 1 Sign: ELEVATED BUN, Number of times reported: 1 Sign: ELEVATED CREATINE-KINASE (CK), Number of times reported: 1 Sign: ELEVATED CREATININE, Number of times reported: 1 Sign: ELEVATED TOTAL BILIRUBIN, Number of times reported: 1 Sign: EXCESSIVE LICKING AND/OR GROOMING, Number of times reported: 1 Sign: FEVER, -

TYPE 1 DIABETES Symptoms
TYPE 1 DIABETES Title: Endocrinology Source: Mayo Clinic Link: http://www.mayoclinic.com/health/type-1-diabetes/DS00329 Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition in which the pancreas produces little or no insulin, a hormone needed to allow sugar (glucose) to enter cells to produce energy. Type 2 diabetes, which is far more common, occurs when the body becomes resistant to the effects of insulin or doesn't make enough insulin. Various factors may contribute to type 1 diabetes, including genetics and exposure to certain viruses. Although type 1 diabetes typically appears during adolescence, it can develop at any age. Despite active research, type 1 diabetes has no cure, although it can be managed. With proper treatment, people who have type 1 diabetes can expect to live longer, healthier lives than in the past. Symptoms By Mayo Clinic staff Type 1 diabetes signs and symptoms can come on quickly and may include: • Increased thirst and frequent urination. As excess sugar builds up in your bloodstream, fluid is pulled from your tissues. This may leave you thirsty. As a result, you may drink — and urinate — more than usual. • Extreme hunger. Without enough insulin to move sugar into your cells, your muscles and organs become depleted of energy. This triggers intense hunger that may persist even after you eat. Without insulin, the sugar in your food never reaches your energy-starved tissues. • Weight loss. Despite eating more than usual to relieve hunger, you may lose weight — sometimes rapidly. Without the energy sugar supplies, your muscle tissues and fat stores may simply shrink. -

Urinary System Diseases and Disorders
URINARY SYSTEM DISEASES AND DISORDERS BERRYHILL & CASHION HS1 2017-2018 - CYSTITIS INFLAMMATION OF THE BLADDER CAUSE=PATHOGENS ENTERING THE URINARY MEATUS CYSTITIS • MORE COMMON IN FEMALES DUE TO SHORT URETHRA • SYMPTOMS=FREQUENT URINATION, HEMATURIA, LOWER BACK PAIN, BLADDER SPASM, FEVER • TREATMENT=ANTIBIOTICS, INCREASE FLUID INTAKE GLOMERULONEPHRITIS • AKA NEPHRITIS • INFLAMMATION OF THE GLOMERULUS • CAN BE ACUTE OR CHRONIC ACUTE GLOMERULONEPHRITIS • USUALLY FOLLOWS A STREPTOCOCCAL INFECTION LIKE STREP THROAT, SCARLET FEVER, RHEUMATIC FEVER • SYMPTOMS=CHILLS, FEVER, FATIGUE, EDEMA, OLIGURIA, HEMATURIA, ALBUMINURIA ACUTE GLOMERULONEPHRITIS • TREATMENT=REST, SALT RESTRICTION, MAINTAIN FLUID & ELECTROLYTE BALANCE, ANTIPYRETICS, DIURETICS, ANTIBIOTICS • WITH TREATMENT, KIDNEY FUNCTION IS USUALLY RESTORED, & PROGNOSIS IS GOOD CHRONIC GLOMERULONEPHRITIS • REPEATED CASES OF ACUTE NEPHRITIS CAN CAUSE CHRONIC NEPHRITIS • PROGRESSIVE, CAUSES SCARRING & SCLEROSING OF GLOMERULI • EARLY SYMPTOMS=HEMATURIA, ALBUMINURIA, HTN • WITH DISEASE PROGRESSION MORE GLOMERULI ARE DESTROYED CHRONIC GLOMERULONEPHRITIS • LATER SYMPTOMS=EDEMA, FATIGUE, ANEMIA, HTN, ANOREXIA, WEIGHT LOSS, CHF, PYURIA, RENAL FAILURE, DEATH • TREATMENT=LOW NA DIET, ANTIHYPERTENSIVE MEDS, MAINTAIN FLUIDS & ELECTROLYTES, HEMODIALYSIS, KIDNEY TRANSPLANT WHEN BOTH KIDNEYS ARE SEVERELY DAMAGED PYELONEPHRITIS • INFLAMMATION OF THE KIDNEY & RENAL PELVIS • CAUSE=PYOGENIC (PUS-FORMING) BACTERIA • SYMPTOMS=CHILLS, FEVER, BACK PAIN, FATIGUE, DYSURIA, HEMATURIA, PYURIA • TREATMENT=ANTIBIOTICS, -

Chapter 31: Lower Urinary Tract Conditions in Elderly Patients
Chapter 31: Lower Urinary Tract Conditions in Elderly Patients Damon Dyche and Jay Hollander William Beaumont Hospital, Royal Oak, Michigan As our population ages, the number of patients pre- uroflow/urodynamic studies, and cystoscopy. Com- senting to their primary care physicians with uro- mon transurethral treatment modalities include re- logic problems is significantly increasing. Urologic section, laser ablation, and microwave or radiofre- issues are the third most common type of complaint quency therapy. in patients 65 yr of age or older and account for at There are two major approaches of medical ther- least a part of 47% of office visits.1 One of the most apy for prostatic outflow obstruction: relaxing the predominant urologic problems in elderly persons, prostate smooth muscle tissue or decreasing glan- ␣ and the focus of this chapter, is lower urinary tract dular volume. 1-adrenergic blockade relaxes the symptoms (LUTS). There are several disease pro- smooth muscle fibers of the prostatic stroma and cesses that can lead to LUTS, as well as a number of can significantly improve urine flow. Because ␣ consequences. In this chapter, we will give a brief blockade can also have significant cardiovascular ␣ overview of the major issues as they relate to elderly side effects, 1 selective medications were devel- persons. oped to specifically target the urinary system. Com- mon nonselective agents include terazosin and dox- azosin; selective medications are tamsulosin and BENIGN PROSTATIC HYPERPLASIA AND alfuzosin. 5-␣ reductase inhibitors block the con- LUTS version of testosterone 3 DHT, which is a potent stimulator of prostatic glandular tissue. This reduc- The prostate surrounds the male urethra between tion in local androgen stimulation results in a pro- the bladder neck and urinary sphincter like a gressive decrease in prostatic volume over a period doughnut.