Urinary Tract Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CMS Manual System Human Services (DHHS) Pub
Department of Health & CMS Manual System Human Services (DHHS) Pub. 100-07 State Operations Centers for Medicare & Provider Certification Medicaid Services (CMS) Transmittal 8 Date: JUNE 28, 2005 NOTE: Transmittal 7, of the State Operations Manual, Pub. 100-07 dated June 27, 2005, has been rescinded and replaced with Transmittal 8, dated June 28, 2005. The word “wound” was misspelled in the Interpretive Guidance section. All other material in this instruction remains the same. SUBJECT: Revision of Appendix PP – Section 483.25(d) – Urinary Incontinence, Tags F315 and F316 I. SUMMARY OF CHANGES: Current Guidance to Surveyors is entirely replaced by the attached revision. The two tags are being combined as one, which will become F315. Tag F316 will be deleted. The regulatory text for both tags will be combined, followed by this revised guidance. NEW/REVISED MATERIAL - EFFECTIVE DATE*: June 28, 2005 IMPLEMENTATION DATE: June 28, 2005 Disclaimer for manual changes only: The revision date and transmittal number apply to the red italicized material only. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual not updated.) (R = REVISED, N = NEW, D = DELETED) – (Only One Per Row.) R/N/D CHAPTER/SECTION/SUBSECTION/TITLE R Appendix PP/Tag F315/Guidance to Surveyors – Urinary Incontinence D Appendix PP/Tag F316/Urinary Incontinence III. FUNDING: Medicare contractors shall implement these instructions within their current operating budgets. IV. ATTACHMENTS: Business Requirements x Manual Instruction Confidential Requirements One-Time Notification Recurring Update Notification *Unless otherwise specified, the effective date is the date of service. -

Urinary Tract Infection (Uti) Fact Sheet
URINARY TRACT INFECTION (UTI) FACT SHEET Overview A urinary tract infection (UTI) is an infection that involves any part of the urinary tract, including the kidneys, bladder and urethra. It is usually caused by exposure of the urinary tract to a fecal organism such as Escherichia coli (E. coli) but also may be caused by other organisms. An indwelling urinary catheter is a drainage tube that is inserted into the urinary bladder through the urethra, is left in place and is connected to a closed urine collection system. Urinary tract infections in patients with an indwelling urinary catheter are called catheter-associated UTIs, or CAUTIs. Signs and Symptoms Common symptoms of UTI include: • fever; • pain or burning in the lower abdomen; • burning during urination; • an increase in the frequency of urination; and • cloudy appearing urine. Causes and Transmission A UTI occurs when germs (usually bacteria) enter the urinary tract through the meatus (the opening of the urinary tract). These germs then cause infection. The urinary tract is normally sterile, meaning it contains no germs. A CAUTI occurs when germs (usually bacteria) enter the urinary tract through the urinary catheter and cause infection. This can occur when health care worker hands are not properly cleaned before the insertion of a catheter or during the process of cleaning or emptying of the urine collection system. Risk Factors Sexually active women, people with blockages in the urinary tract, such as prostate enlargement, and women using certain types of birth control, such as diaphragms, or those who are undergoing menopause are at higher risk of UTI. -

Urinary Incontinence Embarrassing but Treatable 2015 Rev
This information provides a general overview on this topic and may not apply to Health Notes everyone. To find out if this information applies to you and to get more information on From Your Family Doctor this subject, talk to your family doctor. Urinary incontinence Embarrassing but treatable 2015 rev. What is urinary incontinence? Are there different types Urinary incontinence means that you can’t always of incontinence? control when you urinate, or pee. The amount of leakage Yes. There are five types of urinary incontinence. can be small—when you sneeze, cough, or laugh—or large, due to very strong urges to urinate that are hard to Stress incontinence is when urine leaks because of control. This can be embarrassing, but it can be treated. sudden pressure on your lower stomach muscles, such as when you cough, sneeze, laugh, rise from a Millions of adults in North America have urinary chair, lift something, or exercise. Stress incontinence incontinence. It’s most common in women over 50 years usually occurs when the pelvic muscles are weakened, of age, but it can also affect younger people, especially sometimes by childbirth, or by prostate or other pelvic women who have just given birth. surgery. Stress incontinence is common in women. Be sure to talk to your doctor if you have this problem. Urge incontinence is when the need to urinate comes on If you hide your incontinence, you risk getting rashes, too fast—before you can get to a toilet. Your body may only sores, and skin and urinary tract (bladder) infections. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Overactive Bladder
Overactive Bladder Introduction Symptoms You Might Notice “Overactive bladder” (OAB) or “unstable bladder” • A strong urge to urinate with little warning. refers to the feeling of needing to urinate much more • More frequent urination. often than is average. Since a medical name for the • Possible dribbling or loss of a large amount of urine. bladder muscle is the “detrusor,” you may also hear this • Difficulty postponing urination. This becomes a major condition called names like “detrusor overactivity” or issue for people with OAB, and can limit activities and “detrusor instability.” travel. OAB is a complex problem, but generally, the • Usually, no physical pain is associated with this bladder may contract/squeeze prematurely and hard problem, but it can be very emotionally and socially enough to make urine leak out before you can make it to disturbing. the bathroom. This type of urine loss is called “urge • Need to get up more than once at night to urinate. incontinence.” • Some people may experience an uncomfortable OAB can occur at any age. Some people are born sensation of urgency. with conditions that affect nerve and muscle signals, resulting in frequent urination, accidents, and bed Possible Causes Your Health Care Provider wetting in children. Other people may not develop OAB May Look For until they are older. The body and its muscles change • Usually no outward physical signs of OAB. with aging, making OAB quite common in older adults. • In older men, this type of bladder problem may be Additionally, certain disease processes or treatments associated with prostate enlargement. may change the bladder to be more sensitive, leading to • In older women, OAB may be related to skin, blood OAB symptoms. -
Urinary System
Urinary system Urinary system terms Nephr/o, Kidney Nephritis, renal artery ren/o Hydronephrosis (abnormal condition involving back Hydro/o Water up of urine into the kidney Cystitis, cystectomy (inflammation of, removal of Cyst/o Bladder bladder) Pyel/o Renal collecting ducts Pyelogram (X-ray of the collecting ducts) Polyuria, anuria (frequent urination, no urine Ur/o, -uria Urine formation) Olig/o Scanty, less than normal Oliguria (reduced urine formation) To surgically reattach, fix in Nephropexy (surgically attach kidney in normal -pexy normal position anatomical position) Urinary system diseases Nephrosis – a noninflammatory disease of kidneys. Nephrolith – a kidney stone. Urethritis – inflammation of the urethra, the final pathway for urine in both sexes, and the common pathway for urine and semen in the male. Nocturia – frequently getting up and urinating during the night. Enuresis – involuntary release of urine, most often in reference to “bedwetting.” Urinary system procedures Nephrologist – I am hoping by now, you would know this is a physician specializing in kidney diseases. Urologist – a physician specializing in the genitourinary tract, which includes kidneys, urinary bladder and urethra of both men and women and the prostate and testes in men. Cystoscopy – looking into the urinary bladder with a fiberoptic instrument. Intravenous pyelogram – special X-rays showing the drainage pattern of the kidneys. A dye opaque to X-rays is injected into a vein. After a waiting period for the blood and dye to pass through the kidneys, X-rays can be taken of the collecting system of the kidney, ureter and bladder. Retrograde pyelogram – personally, I prefer the former procedure! In this procedure a dye opaque to X-rays is flushed backwards up the urethra and bladder and up the ureters to the kidneys. -

Impact of Urolithiasis and Hydronephrosis on Acute Kidney Injury in Patients with Urinary Tract Infection
bioRxiv preprint doi: https://doi.org/10.1101/2020.07.13.200337; this version posted July 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Impact of urolithiasis and hydronephrosis on acute kidney injury in patients with urinary tract infection Short title: Impact of urolithiasis and hydronephrosis on AKI in UTI Chih-Yen Hsiao1,2, Tsung-Hsien Chen1, Yi-Chien Lee3,4, Ming-Cheng Wang5,* 1Division of Nephrology, Department of Internal Medicine, Ditmanson Medical Foundation Chia-Yi Christian Hospital, Chia-Yi, Taiwan 2Department of Hospital and Health Care Administration, Chia Nan University of Pharmacy and Science, Tainan, Taiwan 3Department of Internal Medicine, Fu Jen Catholic University Hospital, Fu Jen Catholic University, New Taipei, Taiwan 4School of Medicine, College of Medicine, Fu Jen Catholic University, New Taipei, Taiwan 5Division of Nephrology, Department of Internal Medicine, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan *[email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.07.13.200337; this version posted July 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Abstract Background: Urolithiasis is a common cause of urinary tract obstruction and urinary tract infection (UTI). This study aimed to identify whether urolithiasis with or without hydronephrosis has an impact on acute kidney injury (AKI) in patients with UTI. -

233 the Use of Absorbent Pads Increases the Risk For
233 Omli R1, Skotnes L H1, Romild U1, Kuhry E1 1. Namsos Hospital THE USE OF ABSORBENT PADS INCREASES THE RISK FOR LOWER URINARY TRACT INFECTIONS IN NURSING HOMES RESIDENTS. Hypothesis / aims of study Urinary incontinence is a common medical problem in the nursing home population. The aim of this study was to determine whether use of absorbent pads is a risk factor for the development of lower urinary tract infections in nursing home residents. Introduction Lower urinary tract infections (UTIs) are a common medical problem in the elderly. Different kinds of absorbent products, such as diapers, pad and pant combinations, are used in incontinence care. In some cases, indwelling catheters, external condom catheters or in-and-out catheterisation are options for managing bladder dysfunction. About 23% of the residents in nursing homes don’t need toilet assistance. That means that the majority of residents is dependent on help from nursing staff for toileting and help to change soiled absorbent pads. Transmission of bacteria during incontinence care is associated with UTIs in elderly. In the vulnerable nursing home population, UTIs are a frequent problem and can lead to increased morbidity and even mortality. The prevalence of UTIs in nursing home residents is approximately 30%. Improving hand hygiene among staffing in nursing homes is one of the most important and effective methods to reduce hand born transmission of pathological microbes. Studies in long-term-care facilities document a lack of hand hygiene in connection to staff-resident interactions. This study studies the association between the use of absorbent pads and symptomatic UTIs in the nursing home population. -
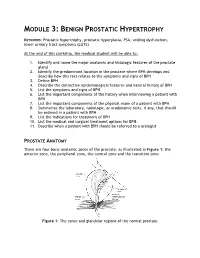
Module 3: Benign Prostatic Hypertrophy
MODULE 3: BENIGN PROSTATIC HYPERTROPHY KEYWORDS: Prostatic hypertrophy, prostatic hyperplasia, PSA, voiding dysfunction, lower urinary tract symptoms (LUTS) At the end of this clerkship, the medical student will be able to: 1. Identify and name the major anatomic and histologic features of the prostate gland 2. Identify the predominant location in the prostate where BPH develops and describe how this fact relates to the symptoms and signs of BPH 3. Define BPH 4. Describe the distinctive epidemiological features and natural history of BPH 5. List the symptoms and signs of BPH 6. List the important components of the history when interviewing a patient with BPH 7. List the important components of the physical exam of a patient with BPH 8. Summarize the laboratory, radiologic, or urodynamic tests, if any, that should be ordered in a patient with BPH 9. List the indications for treatment of BPH 10. List the medical and surgical treatment options for BPH. 11. Describe when a patient with BPH should be referred to a urologist PROSTATE ANATOMY There are four basic anatomic zones of the prostate, as illustrated in Figure 1: the anterior zone, the peripheral zone, the central zone and the transition zone. Figure 1: The zones and glandular regions of the normal prostate. The anterior zone is entirely fibromuscular and non-glandular, and it appears to have little significance in prostatic function or pathology. This area comprises approximately 20% of the bulk of prostatic tissue. The peripheral zone is composed entirely of acinar tissue. It comprises the posterior surface of the prostate, including the apical, lateral, posterolateral and anterolateral portions of the prostate. -

Urinary Incontinence ! ! !What Is Urinary Incontinence? Leakage of Urine Is Called Urinary Incontinence
! ! ! Urinary Incontinence ! ! !What is urinary incontinence? Leakage of urine is called urinary incontinence. Some women leak small amounts of !urine. At other times, leakage of urine is frequent or severe. !Are there different types of urinary incontinence? !There are several types of urinary incontinence: • Stress urinary incontinence is loss of urine when a woman coughs, laughs, or sneezes. Leaks also can happen when a woman walks, runs, or exercises. It is caused by a weakening of the tissues that support the bladder or the muscles of the ! urethra. • Urge incontinence is leakage of urine caused by overactive bladder muscles that ! contract too often or problems with the nerves that send signals to the bladder !• Mixed incontinence is a combination of both stress and urge incontinence symptoms • Overflow incontinence is a steady loss of small amounts of urine when the bladder does not empty all the way during voiding. It can be caused by an underactive bladder ! muscle or blockage of the urethra. !What are the symptoms of urinary incontinence? !In addition to leaking urine, a woman with incontinence also may have other symptoms: • Urgency— A strong urge to urinate whether or not the bladder is full, often with pelvic ! pressure !• Frequency— Voiding more often than she considers usual !• Nocturia — The need to void during hours of sleep !• Dysuria — Painful voiding !• Enuresis— Bed-wetting or leaking while sleeping ! What causes urinary incontinence? ! Urinary incontience can have short-term causes and long-term causes. Short-term !causes are easier to treat and include the following: • Urinary tract infection— Loss of bladder control may be caused by an infection of the urinary tract. -

Frequently Asked Questions About Overactive Bladder
ABOUT OAB Frequently Asked Questions about Overactive Bladder What is Overactive Bladder (OAB)? If you live with OAB, you may also: Overactive Bladder (OAB) isn’t a disease. It’s the u Leak urine (incontinence): Sometimes people name of a group of urinary symptoms. The most with OAB also have “urgency incontinence.” common symptom of OAB is a sudden urge to This means that urine leaks when you feel urinate that you can’t control. Some people will the sudden urge to go. This isn’t the same as leak urine when they feel this urge. Having to “stress urinary incontinence” or “SUI.” People urinate many times during the day and night is with SUI leak urine while sneezing, laughing or another symptom of OAB. doing other physical activities. (You can learn more about SUI at UrologyHealth.org/SUI.) How common is OAB? u Urinate frequently: You may also need to go OAB is common. It affects millions of Americans. to the bathroom many times during the day. As many as 30 percent of men and 40 percent The number of times someone urinates varies of women in the United States live with OAB from person to person. But many experts symptoms. agree that going to the bathroom more than eight times in 24 hours is “frequent urination.” Who is at risk for OAB? u Wake up at night to urinate: Waking from As you grow older, you’re at higher risk for sleep to go to the bathroom more than once a OAB. But no matter what your age, there are night is another symptom of OAB. -

UTI and Pyelonephritis Summary
CHI Franciscan Health UTI & Pyelonephritis Summary UTI/pyelonephritis is one of the most common infectious processes but is also often over-treated. Inappropriate treatment rates vary between 17-26%1,2 and up to 52% in patients with indwelling urinary catheters3. Overtreatment can result in unnecessary medication side effects, the development of Clostridium difficile resistance4, colonization with drug-resistant organisms, and undue costs to the health system. Pharmacists can play and important role in optimizing drug therapy to include the recommendation to stop inappropriate antibiotics when their use is not indicated. Asymptomatic bacteriuria (ASB): the presence of bacteria in the urine without signs/symptoms of infection5 o McGeer Criteria often used to define infection, particularly in the long-term care setting6 Clinical (at least one of the following) Lab (at least one of the following) □ Acute dysuria □ Voided specimen: positive urine culture □ Acute pain, swelling, or tenderness of testes, (> 105 CFU/mL), no more than 2 epididymis, or prostate organisms □ Fever or leukocytosis with one of the following: □ Straight cath specimen: positive urine ○ Acute CVA pain or tenderness culture (> 105 CFU/mL), any number of ○ Suprapubic pain organisms ○ Gross hematuria ○ New or marked increase in incontinence ○ New or marked increase in urgency ○ New or marked increase in frequency □ Two of the preceding symptoms in the absence of fever or leukocytosis o ASB should only be treated in pregnant women and patients undergoing invasive urologic procedures5 o People with ASB also often have WBC in the urine (pyuria) but, in the absence of symptoms, this is not indicative of infection o Caused by: colonization of the bladder or contamination of the sample .