Overactive Bladder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urinary Incontinence Embarrassing but Treatable 2015 Rev
This information provides a general overview on this topic and may not apply to Health Notes everyone. To find out if this information applies to you and to get more information on From Your Family Doctor this subject, talk to your family doctor. Urinary incontinence Embarrassing but treatable 2015 rev. What is urinary incontinence? Are there different types Urinary incontinence means that you can’t always of incontinence? control when you urinate, or pee. The amount of leakage Yes. There are five types of urinary incontinence. can be small—when you sneeze, cough, or laugh—or large, due to very strong urges to urinate that are hard to Stress incontinence is when urine leaks because of control. This can be embarrassing, but it can be treated. sudden pressure on your lower stomach muscles, such as when you cough, sneeze, laugh, rise from a Millions of adults in North America have urinary chair, lift something, or exercise. Stress incontinence incontinence. It’s most common in women over 50 years usually occurs when the pelvic muscles are weakened, of age, but it can also affect younger people, especially sometimes by childbirth, or by prostate or other pelvic women who have just given birth. surgery. Stress incontinence is common in women. Be sure to talk to your doctor if you have this problem. Urge incontinence is when the need to urinate comes on If you hide your incontinence, you risk getting rashes, too fast—before you can get to a toilet. Your body may only sores, and skin and urinary tract (bladder) infections. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -
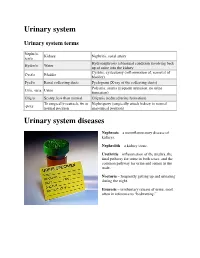
Urinary System
Urinary system Urinary system terms Nephr/o, Kidney Nephritis, renal artery ren/o Hydronephrosis (abnormal condition involving back Hydro/o Water up of urine into the kidney Cystitis, cystectomy (inflammation of, removal of Cyst/o Bladder bladder) Pyel/o Renal collecting ducts Pyelogram (X-ray of the collecting ducts) Polyuria, anuria (frequent urination, no urine Ur/o, -uria Urine formation) Olig/o Scanty, less than normal Oliguria (reduced urine formation) To surgically reattach, fix in Nephropexy (surgically attach kidney in normal -pexy normal position anatomical position) Urinary system diseases Nephrosis – a noninflammatory disease of kidneys. Nephrolith – a kidney stone. Urethritis – inflammation of the urethra, the final pathway for urine in both sexes, and the common pathway for urine and semen in the male. Nocturia – frequently getting up and urinating during the night. Enuresis – involuntary release of urine, most often in reference to “bedwetting.” Urinary system procedures Nephrologist – I am hoping by now, you would know this is a physician specializing in kidney diseases. Urologist – a physician specializing in the genitourinary tract, which includes kidneys, urinary bladder and urethra of both men and women and the prostate and testes in men. Cystoscopy – looking into the urinary bladder with a fiberoptic instrument. Intravenous pyelogram – special X-rays showing the drainage pattern of the kidneys. A dye opaque to X-rays is injected into a vein. After a waiting period for the blood and dye to pass through the kidneys, X-rays can be taken of the collecting system of the kidney, ureter and bladder. Retrograde pyelogram – personally, I prefer the former procedure! In this procedure a dye opaque to X-rays is flushed backwards up the urethra and bladder and up the ureters to the kidneys. -

Frequently Asked Questions About Overactive Bladder
ABOUT OAB Frequently Asked Questions about Overactive Bladder What is Overactive Bladder (OAB)? If you live with OAB, you may also: Overactive Bladder (OAB) isn’t a disease. It’s the u Leak urine (incontinence): Sometimes people name of a group of urinary symptoms. The most with OAB also have “urgency incontinence.” common symptom of OAB is a sudden urge to This means that urine leaks when you feel urinate that you can’t control. Some people will the sudden urge to go. This isn’t the same as leak urine when they feel this urge. Having to “stress urinary incontinence” or “SUI.” People urinate many times during the day and night is with SUI leak urine while sneezing, laughing or another symptom of OAB. doing other physical activities. (You can learn more about SUI at UrologyHealth.org/SUI.) How common is OAB? u Urinate frequently: You may also need to go OAB is common. It affects millions of Americans. to the bathroom many times during the day. As many as 30 percent of men and 40 percent The number of times someone urinates varies of women in the United States live with OAB from person to person. But many experts symptoms. agree that going to the bathroom more than eight times in 24 hours is “frequent urination.” Who is at risk for OAB? u Wake up at night to urinate: Waking from As you grow older, you’re at higher risk for sleep to go to the bathroom more than once a OAB. But no matter what your age, there are night is another symptom of OAB. -

Gotta Gotta Go Right Now: a Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis
Gotta Go Right Now: A Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis Kelly Haack, M.A., and William J. Warzak, Ph.D. Department of Psychology, Munroe-Meyer Institute at the University of Nebraska Medical Center INTRODUCTION METHOD RESULTS Participant Bartter’s Syndrome Baseline 2 Months Following BRT ¾ Bartter’s Syndrome is caused by a defect in the kidney’s ¾ The participant was a 14-year-old male with Bartter’s Syndrome. Fluid Intake and Output Fluid Intake and Output ability to reabsorb potassium. ¾ He presented with frequent daytime and nighttime voiding. 1000 1000 ¾ As a result, the kidneys remove too much potassium from ¾ Medical History: 900 900 the body. 4 years old: Renal Ultrasound showed normal kidneys and 800 800 ¾ Excessive loss of potassium leads to muscle cramping and hypokalemia (low potassium level) was ruled out. Intake weakness, constipation, increased frequency of urination, 700 700 Intake and growth failure. 11 years old: Ditropan XL 10 mg daily and Imipramine 35 mg 600 600 daily were prescribed to treat symptoms of overactive bladder, Nocturnal Enuresis 500 500 ML such as frequent urination. ML ¾ Nocturnal Enuresis is involuntary passing of urine while 12 years old: Neurological exam was normal and neurogenic 400 400 asleep. bladder was ruled out. 300 300 Output Bartter’s Syndrome Output • Continued taking Ditropan and Imipramine. 200 200 and • Prescribed DDAVP 0.6 mg each evening to increase urine 100 100 concentration and decrease urine production. Nocturnal Enuresis 0 0 ¾ Adolescents with Bartter’s Syndrome often have a problem • Started use of a urine alarm; however, it was a short trial and 3:00 6:00 7:45 9:45 1:00 2:30 4:00 5:00 6:20 8:00 9:30 1:00 2:45 5:00 7:00 9:00 2:00 4:00 5:00 7:00 9:00 1:45 4:00 7:00 4:00 7:05 9:45 2:00 4:00 5:45 7:00 9:30 2:30 5:00 7:45 2:30 4:30 7:00 9:30 1:45 5:00 12:00 11:00 11:00 10:45 12:00 10:00 12:00 concentrating urine and excrete an excessive volume of he slept through it and continued to wet 5 out of 7 nights. -
Urinary Tract Infections
Urinary Tract Infections www.kidney.org Did you know that... n Urinary tract infections (UTIs) are responsible for nearly 10 million doctor visits each year. n One in five women will have at least one UTI in her lifetime. Nearly 20 percent of women who have a UTI will have another, and 30 percent of those will have yet another. Of this last group, 80 percent will have recurrences. n About 80 to 90 percent of UTIs are caused by a single type of bacteria. 2 NATIONAL KIDNEY FOUNDATION n UTIs can be treated effectively with medications called antibiotics. n People who get repeated UTIs may need additional tests to check for other health problems. n UTIs also may be called cystitis or a bladder infection. This brochure answers the questions most often asked about UTIs. If you have more questions, speak to your doctor. What is a urinary tract infection? A urinary tract infection is what happens when bacteria (germs) get into the urinary tract (the bladder) and multiply. The result is redness, swelling and pain in the urinary tract (see diagram). WWW.KIDNEY.ORG 3 Most UTIs stay in the bladder, the pouch-shaped organ where urine is stored before it passes out of the body. If a UTI is not treated promptly, the bacteria can travel up to the kidneys and cause a more serious type of infection, called pyelonephritis (pronounced pie-low-nef-right- iss). Pyelonephritis is an actual infection of the kidney, where urine is produced. This may result in fever and back pain. What causes a UTI? About 80 to 90 percent of UTIs are caused by a type of bacteria, called E. -

FDA CVM Comprehensive ADE Report Listing for Afoxolaner
CVM ADE Comprehensive Clinical Detail Report Listing Cumulative Date Range : 04-Sep-2013 -thru- 31-Jul-2018 Included 1932a cases = : True Included Medicated Feed cases = : False DRUG: AFOXOLANER Species: Cat Route of Administration: oral Sign: VOMITING, Number of times reported: 4 Sign: HYPERACTIVITY, Number of times reported: 3 Sign: ITCHING, Number of times reported: 3 Sign: LETHARGY, Number of times reported: 3 Sign: PRURITUS, Number of times reported: 3 Sign: ACCIDENTAL EXPOSURE, Number of times reported: 2 Sign: ANOREXIA, Number of times reported: 2 Sign: LABOURED BREATHING, Number of times reported: 2 Sign: NOT EATING, Number of times reported: 2 Sign: PANTING, Number of times reported: 2 Sign: SEIZURE NOS, Number of times reported: 2 Sign: ABNORMAL TEST RESULT, Number of times reported: 1 Sign: AGITATION, Number of times reported: 1 Sign: ALOPECIA, Number of times reported: 1 Sign: ANAEMIA NOS, Number of times reported: 1 Sign: ATAXIA, Number of times reported: 1 Sign: CERVICAL VENTROFLEXION, Number of times reported: 1 Sign: CONSTIPATION, Number of times reported: 1 Sign: DECREASED CHOLESTEROL (TOTAL), Number of times reported: 1 Sign: ELEVATED ALT, Number of times reported: 1 Sign: ELEVATED AST, Number of times reported: 1 Sign: ELEVATED BUN, Number of times reported: 1 Sign: ELEVATED CREATINE-KINASE (CK), Number of times reported: 1 Sign: ELEVATED CREATININE, Number of times reported: 1 Sign: ELEVATED TOTAL BILIRUBIN, Number of times reported: 1 Sign: EXCESSIVE LICKING AND/OR GROOMING, Number of times reported: 1 Sign: FEVER, -

TYPE 1 DIABETES Symptoms
TYPE 1 DIABETES Title: Endocrinology Source: Mayo Clinic Link: http://www.mayoclinic.com/health/type-1-diabetes/DS00329 Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition in which the pancreas produces little or no insulin, a hormone needed to allow sugar (glucose) to enter cells to produce energy. Type 2 diabetes, which is far more common, occurs when the body becomes resistant to the effects of insulin or doesn't make enough insulin. Various factors may contribute to type 1 diabetes, including genetics and exposure to certain viruses. Although type 1 diabetes typically appears during adolescence, it can develop at any age. Despite active research, type 1 diabetes has no cure, although it can be managed. With proper treatment, people who have type 1 diabetes can expect to live longer, healthier lives than in the past. Symptoms By Mayo Clinic staff Type 1 diabetes signs and symptoms can come on quickly and may include: • Increased thirst and frequent urination. As excess sugar builds up in your bloodstream, fluid is pulled from your tissues. This may leave you thirsty. As a result, you may drink — and urinate — more than usual. • Extreme hunger. Without enough insulin to move sugar into your cells, your muscles and organs become depleted of energy. This triggers intense hunger that may persist even after you eat. Without insulin, the sugar in your food never reaches your energy-starved tissues. • Weight loss. Despite eating more than usual to relieve hunger, you may lose weight — sometimes rapidly. Without the energy sugar supplies, your muscle tissues and fat stores may simply shrink. -

Urinary System Diseases and Disorders
URINARY SYSTEM DISEASES AND DISORDERS BERRYHILL & CASHION HS1 2017-2018 - CYSTITIS INFLAMMATION OF THE BLADDER CAUSE=PATHOGENS ENTERING THE URINARY MEATUS CYSTITIS • MORE COMMON IN FEMALES DUE TO SHORT URETHRA • SYMPTOMS=FREQUENT URINATION, HEMATURIA, LOWER BACK PAIN, BLADDER SPASM, FEVER • TREATMENT=ANTIBIOTICS, INCREASE FLUID INTAKE GLOMERULONEPHRITIS • AKA NEPHRITIS • INFLAMMATION OF THE GLOMERULUS • CAN BE ACUTE OR CHRONIC ACUTE GLOMERULONEPHRITIS • USUALLY FOLLOWS A STREPTOCOCCAL INFECTION LIKE STREP THROAT, SCARLET FEVER, RHEUMATIC FEVER • SYMPTOMS=CHILLS, FEVER, FATIGUE, EDEMA, OLIGURIA, HEMATURIA, ALBUMINURIA ACUTE GLOMERULONEPHRITIS • TREATMENT=REST, SALT RESTRICTION, MAINTAIN FLUID & ELECTROLYTE BALANCE, ANTIPYRETICS, DIURETICS, ANTIBIOTICS • WITH TREATMENT, KIDNEY FUNCTION IS USUALLY RESTORED, & PROGNOSIS IS GOOD CHRONIC GLOMERULONEPHRITIS • REPEATED CASES OF ACUTE NEPHRITIS CAN CAUSE CHRONIC NEPHRITIS • PROGRESSIVE, CAUSES SCARRING & SCLEROSING OF GLOMERULI • EARLY SYMPTOMS=HEMATURIA, ALBUMINURIA, HTN • WITH DISEASE PROGRESSION MORE GLOMERULI ARE DESTROYED CHRONIC GLOMERULONEPHRITIS • LATER SYMPTOMS=EDEMA, FATIGUE, ANEMIA, HTN, ANOREXIA, WEIGHT LOSS, CHF, PYURIA, RENAL FAILURE, DEATH • TREATMENT=LOW NA DIET, ANTIHYPERTENSIVE MEDS, MAINTAIN FLUIDS & ELECTROLYTES, HEMODIALYSIS, KIDNEY TRANSPLANT WHEN BOTH KIDNEYS ARE SEVERELY DAMAGED PYELONEPHRITIS • INFLAMMATION OF THE KIDNEY & RENAL PELVIS • CAUSE=PYOGENIC (PUS-FORMING) BACTERIA • SYMPTOMS=CHILLS, FEVER, BACK PAIN, FATIGUE, DYSURIA, HEMATURIA, PYURIA • TREATMENT=ANTIBIOTICS, -
EMA Medical Terms Simplifier
EMA medical terms simplifier Plain-language description of medical terms related to medicines use polyuria petechiae tophi trismus idiopathic immunoglobulins acute antagonist An agency of the European Union 19 March 2021 EMA/158473/2021 EMA Medical Terms Simplifier Plain-language description of medical terms related to medicines use This compilation gives plain-language descriptions of medical terms commonly used in information about medicines. Communication specialists at EMA use these descriptions for materials prepared for the public. In our documents, we often adjust the description wordings to fit the context so that the writing flows smoothly without distorting the meaning. Since the main purpose of these descriptions is to serve our own writing needs, some also include alternative or optional wording to use as needed; we use ‘<>’ for this purpose. Our list concentrates on side effects and similar terms in summaries of product characteristics and public assessments of medicines but omits terms that are used only rarely. It does not include descriptions of most disease states or those that relate to specialties such as regulation, statistics and complementary medicine or, indeed, broader fields of medicine such as anatomy, microbiology, pathology and physiology. This resource is continually reviewed and updated internally, and we will publish updates periodically. If you have comments or suggestions, you may contact us by filling in this form. EMA Medical Terms Simplifier EMA/158473/2021 Page 1/76 A│B│C│D│E│F│G│H│I│J│K│L│M│N│O│P│Q│R│S│T│U│V│W│X│Y│Z -

Overactive Bladder During Childhood: When and How It Should Be Treated
Incont Pelvic Floor Dysfunct 2010; 4(1):13-17 Review Overactive Bladder during Childhood: When and How It Should Be Treated Yi-Sheng Chen, M.D.1, Stephen Shei-Dei Yang, M.D.2, Shang-Jen Chang, M.D.2 Department of Urology1, National Taiwan University Hospital, Yun-Lin Branch, Yunlin, Taiwan; Division of Urology2, Buddhist Tzu Chi General Hospital, Taipei Branch, Taipei, Taiwan and School of Medicine, Buddhist Tzu Chi University, Hualien, Taiwan fkqolar`qflk ê~íÉ=çÑ=ÉåìêÉëáë=ÇÉÅêÉ~ëÉÇ=ïáíÜ=~ÖÉI=áí=åÉîÉê=êÉ~ÅÜÉÇ=MBK=qÜÉ=êÉëìäíë çÑ=íÜÉ=ëíìÇó=Äó=h~êàáï~ê~=Éí=~ä=~äëç=ëÜçïÉÇ=íÜÉ=ë~ãÉ=íêÉåÇ=xVzK=få=íÜÉ m~íáÉåíë=ïáíÜ=çîÉê~ÅíáîÉ=Ää~ÇÇÉê=El^_F=ïÉêÉ=~ëëìãÉÇ=íç=Ü~îÉ é~íáÉåíë=ïáíÜ=Ç~óíáãÉ=ìêáå~êó=áåÅçåíáåÉåÅÉI=ìêÖÉåÅó=~äçåÉ=ï~ë=íÜÉ=ãçëí ÇÉíêìëçê=çîÉê~ÅíáîáíóI=ìêÖÉ=ëóåÇêçãÉI=ÜóéÉê~ÅíáîÉ=Ää~ÇÇÉêI=éÉêëáëíÉåí Åçããçå=ÅÜ~ê~ÅíÉêáëíáÅ=áå=ÄçíÜ=ëÉñÉëK áåÑ~åíáäÉ=Ää~ÇÇÉêI=~åÇ=ÇÉíêìëçê=ÜóéÉêíçåá~K=`ÜáäÇêÉå=ïáíÜ=l^_=ã~ó éêÉëÉåí=ïáíÜ=ëóãéíçãë=çÑ=Ç~óíáãÉ=ÑêÉèìÉåí=ìêáå~íáçåI=ìêÖÉåÅóI=áåÅçåJ m^qelmevpflildv íáåÉåÅÉ=~åÇ=åáÖÜííáãÉ=ÉåìêÉëáëK=qÜÉ=ÇÉÑáåáíáçå=çÑ=éÉÇá~íêáÅ=l^_=Äó=íÜÉ fåíÉêå~íáçå~ä=`ÜáäÇêÉåDë=`çåíáåÉåÅÉ=pçÅáÉíó=Ef``pF=áë=áå=~ÅÅçêÇ~åÅÉ=íç qÜÉ=é~íÜçéÜóëáçäçÖó=çÑ=l^_=áë=åçí=ïÉää=ìåÇÉêëíççÇK=qê~Çáíáçå~ääóI íÜÉ=ÅçåëÉåëìë=çÑ=íÜÉ=fåíÉêå~íáçå~ä=`çåíáåÉåÅÉ=pçÅáÉíó=Ef`pF=xNzK=qÜÉ l^_=áë=íÜçìÖÜí=íç=ÄÉ=íÜÉ=êÉëìäí=çÑ=ã~íìê~íáçå=ÇÉä~óK=oÉÅÉåíäóI=êÉëÉ~êÅÜJ ÅçêÉ=ëóãéíçã=çÑ=l^_=áå=ÅÜáäÇêÉå=áë=ìêÖÉåÅó=xNzK=fí=ã~ó=çÅÅìê=ïáíÜ Éêë=Ü~îÉ=ëÜçïå=íÜ~í=l^_=ã~ó=Ü~îÉ=~å=~ëëçÅá~íáçå=ïáíÜ=ëÉñì~ä=ÇóëJ ëóãéíçãë=çÑ=ìêÖÉ=áåÅçåíáåÉåÅÉI=ÑêÉèìÉåí=ìêáå~íáçå=~åÇ=åçÅíìêå~ä ÑìåÅíáçå=xNMJNOzK=^äëçI=íÜÉ=êÉëÉ~êÅÜÉêë=~äëç=ëìÖÖÉëíÉÇ=íÜ~í=l^_=ã~ó -
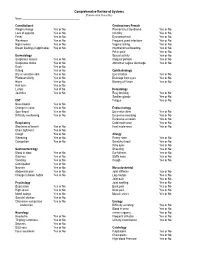
Comprehensive Review of Systems (Please Circle Yes Or No) Name: ______
Comprehensive Review of Systems (Please circle Yes or No) Name: __________________________________________ Constitutional Genitourinary Female Weight change Yes or No Premenstrual Syndrome Yes or No Loss of appetite Yes or No Infertility Yes or No Fever Yes or No Dysmenorrheal Yes or No Weakness Yes or No Frequent yeast infections Yes or No Night sweats Yes or No Vaginal itching Yes or No Breast feeding (if applicable) Yes or No Intermenstrual bleeding Yes or No Pelvic pain Yes or No Dermatology Sexual activity Yes or No Suspicious lesions Yes or No Irregular periods Yes or No Suspicious moles Yes or No Abnormal vaginal discharge Yes or No Rash Yes or No Itching Yes or No Ophthalmology Dry or sensitive skin Yes or No Eye irritation Yes or No Photosensitivity Yes or No Drainage from eyes Yes or No Hives Yes or No Blurring of Vision Yes or No Hair loss Yes or No Lumps Yes of No Hematology Jaundice Yes or No Easy bruising Yes or No Swollen glands Yes or No ENT Fatigue Yes or No Nose bleeds Yes or No Change in voice Yes or No Endocrinology Sore throat Yes or No Excessive thirst Yes or No Difficulty swallowing Yes or No Excessive sweating Yes or No Excessive urination Yes or No Respiratory Cold intolerance Yes or No Shortness of breath Yes or No Heat intolerance Yes or No Chest tightness Yes or No Cough Yes or No Allergy Wheezing Yes or No Runny nose Yes or No Congestion Yes or No Scratchy throat Yes or No Itchy eyes Yes or No Gastroenterology Sneezing Yes or No Blood in stool Yes or No Ear fullness Yes or No Diarrhea Yes or No Stuffy nose