CMS Manual System Human Services (DHHS) Pub
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urinary Incontinence: Impact on Long Term Care
Urinary Incontinence: Impact on Long Term Care Muhammad S. Choudhury, MD, FACS Professor and Chairman Department of Urology New York Medical College Director of Urology Westchester Medical Center 1 Urinary Incontinence: Overview • Definition • Scope • Anatomy and Physiology of Micturition • Types • Diagnosis • Management • Impact on Long Term Care 2 Urinary Incontinence: Definition • Involuntary leakage of urine which is personally and socially unacceptable to an individual. • It is a multifactorial syndrome caused by a combination of: • Genito urinary pathology. • Age related changes. • Comorbid conditions that impair normal micturition. • Loss of functional ability to toilet oneself. 3 Urinary Incontinence: Scope • Prevalence of Urinary incontinence increase with age. • Affects more women than men (2:1) up to age 80. • After age 80, both women and men are equally affected. • Urinary Incontinence affect 15% to 30% of the general population > 65 years. • > 50% of 1.5 million Long Term Care residents may be incontinent. • The cost to care for this group is >5 billion per year. • The total cost of care for Urinary Incontinence in the U.S. is estimated to be over $36 billion. Ehtman et al., 2012. 4 Urinary Incontinence: Impact on Quality of Life • Loss of self esteem. • Avoidance of social activity and interaction. • Decreased ability to maintain independent life style. • Increased dependence on care givers. • One of the most common reason for long term care placement. Grindley et al. Age Aging. 1998; 22: 82-89/Harris T. Aging in the eighties. NCHS # 121 1985. Noelker L. Gerontologist 1987; 27: 194-200. 5 Health related consequences of Urinary Incontinence • Increased propensity for fall/fracture. -

A Clever Technique for Placement of a Urinary Catheter Over a Wire
[Downloaded free from http://www.urologyannals.com on Monday, August 24, 2015, IP: 107.133.192.199] Original Article A clever technique for placement of a urinary catheter over a wire Joel E. Abbott, Adam Heinemann, Robert Badalament, Julio G. Davalos1 Department of Urology, St. John Providence, Michigan State University, Detroit, MI 48071, 1Chesapeake Urology Associates, University of Maryland, Baltimore, MD 21061, USA Abstract Objective: The objective was to present a straightforward, step-by-step reproducible technique for placement of a guide-wire into any type of urethral catheter, thereby offering a means of access similar to that of a council-tip in a situation that may require a different type of catheter guided over a wire. Materials and Methods: Using a shielded intravenous catheter inserted into the eyelet of a urinary catheter and through the distal tip, a “counsel-tip” can be created in any size or type of catheter. Once transurethral bladder access has been achieved with a hydrophilic guide-wire, this technique will allow unrestricted use of catheters placed over a wire facilitating guided catheterization. Results: Urethral catheters of different types and sizes are easily advanced into the bladder with wire-guidance; catheterization is improved in the setting of difficult urethral catheterization (DUC). Cost analysis demonstrates benefit overuse of traditional council-tip catheter. Conclusion: Placing urinary catheters over a wire is standard practice for urologists, however, use of this technique gives the freedom of performing wire-guided catheterization in more situations than a council-tip allows. This technique facilitates successful transurethral catheterization over wire in the setting of DUC for all catheter types and styles aiding in urologic management of patients at a cost benefit to the health care system. -

What a Difference a Delay Makes! CT Urogram: a Pictorial Essay
Abdominal Radiology (2019) 44:3919–3934 https://doi.org/10.1007/s00261-019-02086-0 SPECIAL SECTION : UROTHELIAL DISEASE What a diference a delay makes! CT urogram: a pictorial essay Abraham Noorbakhsh1 · Lejla Aganovic1,2 · Noushin Vahdat1,2 · Soudabeh Fazeli1 · Romy Chung1 · Fiona Cassidy1,2 Published online: 18 June 2019 © This is a U.S. Government work and not under copyright protection in the US; foreign copyright protection may apply 2019 Abstract Purpose The aim of this pictorial essay is to demonstrate several cases where the diagnosis would have been difcult or impossible without the excretory phase image of CT urography. Methods A brief discussion of CT urography technique and dose reduction is followed by several cases illustrating the utility of CT urography. Results CT urography has become the primary imaging modality for evaluation of hematuria, as well as in the staging and surveillance of urinary tract malignancies. CT urography includes a non-contrast phase and contrast-enhanced nephrographic and excretory (delayed) phases. While the three phases add to the diagnostic ability of CT urography, it also adds potential patient radiation dose. Several techniques including automatic exposure control, iterative reconstruction algorithms, higher noise tolerance, and split-bolus have been successfully used to mitigate dose. The excretory phase is timed such that the excreted contrast opacifes the urinary collecting system and allows for greater detection of flling defects or other abnormali- ties. Sixteen cases illustrating the utility of excretory phase imaging are reviewed. Conclusions Excretory phase imaging of CT urography can be an essential tool for detecting and appropriately characterizing urinary tract malignancies, renal papillary and medullary abnormalities, CT radiolucent stones, congenital abnormalities, certain chronic infammatory conditions, and perinephric collections. -

Mimickers of Urothelial Carcinoma and the Approach to Differential Diagnosis
Review Mimickers of Urothelial Carcinoma and the Approach to Differential Diagnosis Claudia Manini 1, Javier C. Angulo 2,3 and José I. López 4,* 1 Department of Pathology, San Giovanni Bosco Hospital, 10154 Turin, Italy; [email protected] 2 Clinical Department, Faculty of Medical Sciences, European University of Madrid, 28907 Getafe, Spain; [email protected] 3 Department of Urology, University Hospital of Getafe, 28905 Getafe, Spain 4 Department of Pathology, Cruces University Hospital, Biocruces-Bizkaia Health Research Institute, 48903 Barakaldo, Spain * Correspondence: [email protected]; Tel.: +34-94-600-6084 Received: 17 December 2020; Accepted: 18 February 2021; Published: 25 February 2021 Abstract: A broad spectrum of lesions, including hyperplastic, metaplastic, inflammatory, infectious, and reactive, may mimic cancer all along the urinary tract. This narrative collects most of them from a clinical and pathologic perspective, offering urologists and general pathologists their most salient definitory features. Together with classical, well-known, entities such as urothelial papillomas (conventional (UP) and inverted (IUP)), nephrogenic adenoma (NA), polypoid cystitis (PC), fibroepithelial polyp (FP), prostatic-type polyp (PP), verumontanum cyst (VC), xanthogranulomatous inflammation (XI), reactive changes secondary to BCG instillations (BCGitis), schistosomiasis (SC), keratinizing desquamative squamous metaplasia (KSM), post-radiation changes (PRC), vaginal-type metaplasia (VM), endocervicosis (EC)/endometriosis (EM) (müllerianosis), -

Urinary Tract Infection (UTI): Western and Ayurvedic Diagnosis and Treatment Approaches
Urinary tract infection (UTI): Western and Ayurvedic Diagnosis and Treatment Approaches. By: Mahsa Ranjbarian Urinary system Renal or Urinary system is one of the 10 body systems that we have. This system is the body drainage system. The urinary system is composed of kidneys (vrikka), ureters (mutravaha nadis), bladder(mutrashaya) and urethra(mutramarga). The kidneys are a pair of bean-shaped, fist size organs that lie in the middle of the back, just below the rib cage, one on each side of the spine. Ureters are tubes that carry the wastes or urine from the kidneys to the bladder. The urine finally exit the body from the urethra when the bladder is full.1 Urethras length is shorter in women than men due to the anatomical differences. Major function of the urinary system is to remove wastes and water from our body through urination. Other important functions of the urinary system are as follows. 1. Prevent dehydration and at the same time prevent the buildup of extra fluid in the body 2. Cleans the blood of metabolic wastes 3. Removing toxins from the body 4. Maintaining the homeostasis of many factors including blood PH and blood pressure 5. Producing erythrocytes 6. make hormones that help regulate blood pressure 7. keep bones strong 8. keep levels of electrolytes, such as potassium and phosphate, stable 2 The Urinary system like any other systems of our body is working under the forces of three doshas, subdoshas. Mutravaha srotas, Ambuvahasrota and raktavahasrota are involved in formation and elimination of the urine. Urine gets separated from the rasa by maladhara kala with the help of pachaka pitta and samana vayu and then through the mutravaha srota(channels carrying the urine) it is taken to the bladder. -

Urinary Tract Infection (Uti) Fact Sheet
URINARY TRACT INFECTION (UTI) FACT SHEET Overview A urinary tract infection (UTI) is an infection that involves any part of the urinary tract, including the kidneys, bladder and urethra. It is usually caused by exposure of the urinary tract to a fecal organism such as Escherichia coli (E. coli) but also may be caused by other organisms. An indwelling urinary catheter is a drainage tube that is inserted into the urinary bladder through the urethra, is left in place and is connected to a closed urine collection system. Urinary tract infections in patients with an indwelling urinary catheter are called catheter-associated UTIs, or CAUTIs. Signs and Symptoms Common symptoms of UTI include: • fever; • pain or burning in the lower abdomen; • burning during urination; • an increase in the frequency of urination; and • cloudy appearing urine. Causes and Transmission A UTI occurs when germs (usually bacteria) enter the urinary tract through the meatus (the opening of the urinary tract). These germs then cause infection. The urinary tract is normally sterile, meaning it contains no germs. A CAUTI occurs when germs (usually bacteria) enter the urinary tract through the urinary catheter and cause infection. This can occur when health care worker hands are not properly cleaned before the insertion of a catheter or during the process of cleaning or emptying of the urine collection system. Risk Factors Sexually active women, people with blockages in the urinary tract, such as prostate enlargement, and women using certain types of birth control, such as diaphragms, or those who are undergoing menopause are at higher risk of UTI. -
Interventional Radiology and Interventional Endoscopy Practical Applications for Veterinary Medicine
Interventional Radiology and Interventional Endoscopy Practical Applications for Veterinary Medicine Megan Morgan, VMD, DACVIM Marnin Forman, DVM, DACVIM This lecture is sponsored by… Outline – Background on Interventional Radiology (IR) and Interventional Endoscopy (IE) – IR and IE in the treatment of Urolithiasis – IR and IE in the treatment of Urinary incontinence – IR and IE in the treatment of Tracheal collapse – IR and IE in the treatment of Urinary obstructions IR and IE-Background • What is Interventional Radiology (IR)? – A specialty that utilizes image guidance to perform minimally invasive procedures to diagnose and treat disease. Thoracic radiograph of a patient with a tracheal stent 4 IR and IE-Background • What is Interventional Endoscopy (IE)? – A specialty that utilizes endoscopic guidance to perform minimally invasive procedures to diagnose and treat disease. Cystoscopic image of a patient with bilateral ectopic ureters 5 IR and IE-Background • Image guidance tools - Fluoroscopy - Ultrasound - Digital radiography - CTA - MRA Seldinger Technique • Minimally invasive access http://www.accessmedicine.ca - Natural orifice - Seldinger technique 6 IR and IE-Background • IR and IE goals – Palliation of clinical signs – Adjuvant therapy – Definitive treatment Fluoroscopic image of a retrograde contrast urethrocystogram in a patient with urethral transitional cell carcinoma 7 IR and IE-Background . IR and IE equipment – Guidewires • Most common sizes –0.035 inch--fits through an 18 gauge needle –0.018 inch--fits through a 22 gauge needle –0.025 inch--fits through a 20 gauge needle – Specialized catheters • Categorized by the type of tip Vascular access catheters IR and IE-Background . IR and IE equipment – Sheaths • Sized by the size of the catheter accepted by the sheath • The actual diameter of the sheath is larger than the listed sheath size Vascular access sheath – Stents • Multiple material types • Wire mesh vs. -

Preventing Catheter Associated Urinary Tract Infections (CAUTI): What You Need to Know About Urinary Catheterization
Preventing Catheter Associated Urinary Tract Infections (CAUTI): What You Need to Know About Urinary Catheterization Presented by Mary W. Sears, RN, BA, CWOCN with Capital Nursing Education Objectives • List two (2) advantages of intermittent catheterization over indwelling catheterization • List two (2) specific clinical conditions that are considered acceptable for the placement of an indwelling urinary catheter Capital Nursing Education ©2015. All rights reserved. WOCN Best Practices Can be ordered from WOCN Bookstore @ wocn.org Capital Nursing Education ©2015. All rights reserved. Urinary Catheterization Should only be undertaken when all other methods of urinary system management have been deemed inappropriate or have failed. Short or long-tem usage-depends on cause of urinary dysfunction (Newman-2008) • Indwelling • Intermittent – Urethral – Suprapubic Capital Nursing Education ©2015. All rights reserved. Suprapubic Catheterization • Definition: • Inserted surgically through the anterior abdominal wall 2 cm above pubic bone into the bladder • Allows for continuous drainage • Indications: – Short term use following surgery – Alternative to chronic indwelling catheter – Option for long-term catheterization – To avoid urethral damage in men Capital Nursing Education ©2015. All rights reserved. Suprapubic Catheters • Advantages: – Decreases risk of contamination from organisms from fecal material – Decreases risk of infection due to less antimicrobial content on abdomen vs perineum • Potential problems: – Urine leakage – Skin erosion – Hematoma – Catheter reinsertion difficulty Capital Nursing Education ©2015. All rights reserved. Suprapubic Catheter Insertion/Reinsertion • Initial insertion by physician or specially trained urology specialist • New suprapubic tract takes 10 days to 4 weeks to become established • Reinsertion by appropriately trained health care professional when tract is well established • Interval can range from 2 to 10 weeks WOCN Best Practice (2009) Capital Nursing Education ©2015. -

Female Urethral Catheterization
T h e new england journal o f medicine videos in clinical medicine Female Urethral Catheterization Rafael Ortega, M.D., Linda Ng, M.D., Pavan Sekhar, B.S., and Michael Song, M.A. Introduction Female urethral catheterization, the insertion of a catheter through the urethra into From the Departments of Anesthesiology the urinary bladder to permit drainage of urine, is a fundamental skill for the prac- and Urology, Boston University Medical Center, Boston. Address reprint requests ticing health care professional. to Dr. Ortega at the Department of Anes- thesiology, Boston University Medical Center, 88 E. Newton St., Boston, MA Indications 02118, or at [email protected]. Female urethral catheterization is indicated for both therapeutic and diagnostic pur- N Engl J Med 2008;358:e15. poses. It permits effective bladder drainage in patients with acute or chronic urinary Copyright © 2008 Massachusetts Medical Society. retention. A urinary catheter may be used to instill medication for local intravesical therapy or for irrigation to remove blood and clots from the urinary bladder. Urethral catheterization facilitates diagnosis in several circumstances, such as ob- taining sterile urine specimens for urinalysis, measuring residual volumes after void- ing, instilling contrast media for imaging procedures, and monitoring the urinary output of critically ill patients.1 Contraindications Urethral injury can be a contraindication to catheterization. Urethral injuries are rare and most commonly result from pelvic fractures. If blood is found at the urethral meatus, urethral or bladder neck injury should be considered. If there is any ques- tion of injury, genital and rectal exams should be performed and retrograde urethrog- raphy should be considered before catheterization is attempted; consultation with a specialist before catheterization is prudent. -

233 the Use of Absorbent Pads Increases the Risk For
233 Omli R1, Skotnes L H1, Romild U1, Kuhry E1 1. Namsos Hospital THE USE OF ABSORBENT PADS INCREASES THE RISK FOR LOWER URINARY TRACT INFECTIONS IN NURSING HOMES RESIDENTS. Hypothesis / aims of study Urinary incontinence is a common medical problem in the nursing home population. The aim of this study was to determine whether use of absorbent pads is a risk factor for the development of lower urinary tract infections in nursing home residents. Introduction Lower urinary tract infections (UTIs) are a common medical problem in the elderly. Different kinds of absorbent products, such as diapers, pad and pant combinations, are used in incontinence care. In some cases, indwelling catheters, external condom catheters or in-and-out catheterisation are options for managing bladder dysfunction. About 23% of the residents in nursing homes don’t need toilet assistance. That means that the majority of residents is dependent on help from nursing staff for toileting and help to change soiled absorbent pads. Transmission of bacteria during incontinence care is associated with UTIs in elderly. In the vulnerable nursing home population, UTIs are a frequent problem and can lead to increased morbidity and even mortality. The prevalence of UTIs in nursing home residents is approximately 30%. Improving hand hygiene among staffing in nursing homes is one of the most important and effective methods to reduce hand born transmission of pathological microbes. Studies in long-term-care facilities document a lack of hand hygiene in connection to staff-resident interactions. This study studies the association between the use of absorbent pads and symptomatic UTIs in the nursing home population. -
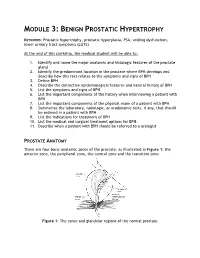
Module 3: Benign Prostatic Hypertrophy
MODULE 3: BENIGN PROSTATIC HYPERTROPHY KEYWORDS: Prostatic hypertrophy, prostatic hyperplasia, PSA, voiding dysfunction, lower urinary tract symptoms (LUTS) At the end of this clerkship, the medical student will be able to: 1. Identify and name the major anatomic and histologic features of the prostate gland 2. Identify the predominant location in the prostate where BPH develops and describe how this fact relates to the symptoms and signs of BPH 3. Define BPH 4. Describe the distinctive epidemiological features and natural history of BPH 5. List the symptoms and signs of BPH 6. List the important components of the history when interviewing a patient with BPH 7. List the important components of the physical exam of a patient with BPH 8. Summarize the laboratory, radiologic, or urodynamic tests, if any, that should be ordered in a patient with BPH 9. List the indications for treatment of BPH 10. List the medical and surgical treatment options for BPH. 11. Describe when a patient with BPH should be referred to a urologist PROSTATE ANATOMY There are four basic anatomic zones of the prostate, as illustrated in Figure 1: the anterior zone, the peripheral zone, the central zone and the transition zone. Figure 1: The zones and glandular regions of the normal prostate. The anterior zone is entirely fibromuscular and non-glandular, and it appears to have little significance in prostatic function or pathology. This area comprises approximately 20% of the bulk of prostatic tissue. The peripheral zone is composed entirely of acinar tissue. It comprises the posterior surface of the prostate, including the apical, lateral, posterolateral and anterolateral portions of the prostate. -

Guide to Treating Your Child's Daytime Or Nighttime Accidents
A GUIDE TO TREATING YOUR CHILD’S Daytime or Nighttime Accidents, Urinary Tract Infections and Constipation UCSF BENIOFF CHILDREN’S HOSPITALS UROLOGY DEPARTMENT This booklet contains information that will help you understand more about your child’s bladder problem(s) and provides tips you can use at home before your first visit to the urology clinic. www.childrenshospitaloakland.org | www.ucsfbenioffchildrens.org 2 | UCSF BENIOFF CHILDREN’S HOSPITALS UROLOGY DEPARTMENT Table of Contents Dear Parent(s), Your child has been referred to the Pediatric Urology Parent Program at UCSF Benioff Children’s Hospitals. We specialize in the treatment of children with bladder and bowel dysfunction. This booklet contains information that will help you understand more about your child’s problem(s) and tips you can use at home before your first visit to the urology clinic. Please review the sections below that match your child’s symptoms. 1. Stool Retention and Urologic Problems (p.3) (Bowel Dysfunction) 2. Bladder Dysfunction (p.7) Includes daytime incontinence (wetting), urinary frequency and infrequency, dysuria (painful urination) and overactive bladder 3. Urinary Tract Infection and Vesicoureteral Reflux (p. 10) 4. Nocturnal Enuresis (p.12) Introduction (Nighttime Bedwetting) It’s distressing to see your child continually having accidents. The good news is that the problem is very 5. Urologic Tests (p.15) common – even if it doesn’t feel that way – and that children generally outgrow it. However, the various interventions we offer can help resolve the issue sooner THIS BOOKLET ALSO CONTAINS: rather than later. » Resources for Parents (p.16) » References (p.17) Childhood bladder and bowel dysfunction takes several forms.