Sleep Medicine Curriculum for Neurology Residents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Am I Still Tired?
ZZZ Why Am I Still Tired? Excessive daytime sleepiness (EDS) is defined as inability to maintain wakefulness or alertness during the major planned awake time of the day, or difficulty waking up after adequate or prolonged nighttime sleep. EDS is a broad condition that includes several sleep disorders like hypo-arousal disorders (involving wake-promoting regions of the brain), narcolepsy, idiopathic hypersomnia. It may be caused by disorders which affect quality of sleep, such as sleep apnea, or a circadian rhythm sleep disorder. Other potential causes of excessive daytime sleepiness include certain medical and psychiatric conditions or vitamin deficiencies, including the use of alcohol or a head injury. This is why it’s important to make sure you have an updated health and wellness physical including lab work with your primary care provider. EDS and Fatigue are different. With EDS (including those with hypersomnias like narcolepsy and idiopathic hypersomnia), you can have the overwhelming urge to nap repeatedly during the day or simply not feel like staying awake. Some may report fighting off increasingly strong urges to sleep during inappropriate times, such as while driving, at work, during a meal or in conversations. Fatigue is a lack of overall energy level. However, EDS and fatigue can often be present together. Do you feel like you are getting the most out of your day? Does daytime sleepiness keep you from activities that you want or need to do in your social or professional life? If the answer is yes, then EDS is negatively impacting your quality of life! EDS can directly impact • Mood swings your overall health in • Poor work or school performance many negative ways: • Weight gain (Decreased activity level and increased food cravings) • Motor vehicle accidents What can be done to fix this? Quick TIPS to get started now • Sleep testing, such as an overnight • Keep a regular sleep/wake sleep study, can help rule out schedule. -

NREM Parasomnias: an Important Comorbidity in Epilepsy Patients of Pediatric Age Pediyatrik Yaş Grubu Epilepsi Hastalarında Önemli Bir Komorbidite: NREM Parasomnileri
Epilepsi 2013;19(3):109-113 DOI: 10.5505/epilepsi.2013.68442 ORIGINAL ARTICLE / KLİNİK ÇALIŞMA NREM Parasomnias: An Important Comorbidity in Epilepsy Patients of Pediatric Age Pediyatrik Yaş Grubu Epilepsi Hastalarında Önemli Bir Komorbidite: NREM Parasomnileri Mecbure NALBANTOĞLU, Gülçin BENBİR, Derya KARADENİZ, Cengiz YALÇINKAYA Department of Neurology, Istanbul University Cerrahpasa Faculty of Medicine, Istanbul Summary Objectives: We here aimed to investigate our pediatric group of patients to reveal the comorbidity of epilepsy and non-rapid eye movement (NREM) parasomnias and their clinical and polysomnographic characteristics. Methods: We retrospectively investigated all patients at the age of 18 or younger internalized within the last two years patients for a full night polysomnographic evaluation in our Sleep and Wake Disorders Unit. The diagnosis of epilepsy was made on the basis of clinical find- ings and electroencephalography findings; and the diagnosis of NREM parasomnia was made according to the International Classification of Sleep Disorders. Results: A total of 29 male (67.4%) and 14 female (32.6%) patients were investigated. Nineteen (44.2%) out of 43 patients were diagnosed as epilepsy. Nine (47.4%) of the patients with epilepsy also had delta-alpha paroxysms (DAP) and partial wakefulness during sleep – which are the characteristics polysomnographic features of NREM parasomnias. Conclusion: We observed a high comorbidity of epilepsy and NREM parasomnia in pediatric group of patients investigated in our sleep center. The arousal parasomnias are increasingly being reported to be more common in patients with epilepsy, probably due to shared com- mon physiopathological mechanism characterized by pathological arousals originating in abnormal thalamo-cortical circuits produced by the central pattern generators. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Society of Anesthesia and Sleep Medicine Guideline On
E SPECIAL ARTICLE Society of Anesthesia and Sleep Medicine Guideline on Intraoperative Management of Adult Patients With Obstructive Sleep Apnea Stavros G. Memtsoudis, MD, PhD, Crispiana Cozowicz, MD, Mahesh Nagappa, MD, Jean Wong, MD, FRCPC, Girish P. Joshi, MBBS, MD, FFARCSI,║ David T. Wong, MD, FRCPC, Anthony G. Doufas, MD, PhD, Meltem*† Yilmaz, MD, Mark H. *Stein,† MD, ‡ Megan L. Krajewski, MD,§ Mandeep Singh, MBBS, MD, MSc, FRCPC, Lukas Pichler,§ MD, Satya Krishna Ramachandran,¶ MD, and Frances #Chung, MBBS, FRCPC** †† ‡‡§§¶¶## *† The purpose of the Society*** of Anesthesia and Sleep Medicine Guideline§ on Intraoperative 07/07/2018 on BhDMf5ePHKbH4TTImqenVLeEdd5NVDXpsv/wMCbE4bP6HQREYnIxByUL3Ye/wWTshIKnEwtQwdU= by http://journals.lww.com/anesthesia-analgesia from Downloaded Management of Adult Patients With Obstructive Sleep Apnea (OSA) is to present recommenda- tions based on current scientific evidence. This guideline seeks to address questions regarding Downloaded the intraoperative care of patients with OSA, including airway management, anesthetic drug and agent effects, and choice of anesthesia type. Given the paucity of high-quality studies from with regard to study design and execution in this perioperative field, recommendations were http://journals.lww.com/anesthesia-analgesia to a large part developed by subject-matter experts through consensus processes, taking into account the current scientific knowledge base and quality of evidence. This guideline may not be suitable for all clinical settings and patients and is not intended to define standards of care or absolute requirements for patient care; thus, assessment of appropriateness should be made on an individualized basis. Adherence to this guideline cannot guarantee successful outcomes, but recommendations should rather aid health care professionals and institutions to formulate plans and develop protocols for the improvement of the perioperative care of patients with OSA, considering patient-related factors, interventions, and resource availability. -

Review of Systems – Return Visit Have You Had Any Problems Related to the Following Symptoms in the Past Month? Circle Yes Or No
REVIEW OF SYSTEMS – RETURN VISIT HAVE YOU HAD ANY PROBLEMS RELATED TO THE FOLLOWING SYMPTOMS IN THE PAST MONTH? CIRCLE YES OR NO Today’s Date: ______________ Name: _______________________________ Date of Birth: __________________ GENERAL GENITOURINARY Fatigue Y N Blood in Urine Y N Fever / Chills Y N Menstrual Irregularity Y N Night Sweats Y N Painful Menstrual Cycle Y N Weight Gain Y N Vaginal Discharge Y N Weight Loss Y N Vaginal Dryness Y N EYES Vaginal Itching Y N Vision Changes Y N Painful Sex Y N EAR, NOSE, & THROAT SKIN Hearing Loss Y N Hair Loss Y N Runny Nose Y N New Skin Lesions Y N Ringing in Ears Y N Rash Y N Sinus Problem Y N Pigmentation Change Y N Sore Throat Y N NEUROLOGIC BREAST Headache Y N Breast Lump Y N Muscular Weakness Y N Tenderness Y N Tingling or Numbness Y N Nipple Discharge Y N Memory Difficulties Y N CARDIOVASCULAR MUSCULOSKELETAL Chest Pain Y N Back Pain Y N Swelling in Legs Y N Limitation of Motion Y N Palpitations Y N Joint Pain Y N Fainting Y N Muscle Pain Y N Irregular Heart Beat Y N ENDOCRINE RESPIRATORY Cold Intolerance Y N Cough Y N Heat Intolerance Y N Shortness of Breath Y N Excessive Thirst Y N Post Nasal Drip Y N Excessive Amount of Urine Y N Wheezing Y N PSYCHOLOGY GASTROINTESTINAL Difficulty Sleeping Y N Abdominal Pain Y N Depression Y N Constipation Y N Anxiety Y N Diarrhea Y N Suicidal Thoughts Y N Hemorrhoids Y N HEMATOLOGIC / LYMPHATIC Nausea Y N Easy Bruising Y N Vomiting Y N Easy Bleeding Y N GENITOURINARY Swollen Lymph Glands Y N Burning with Urination Y N ALLERGY / IMMUNOLOGY Urinary -
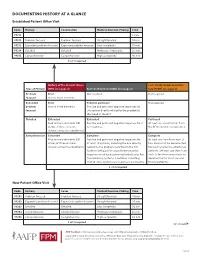
Documenting History at a Glance
DOCUMENTING HISTORY AT A GLANCE Established Patient Office Visit Code History Examination Medical Decision-Making Time 99211 — — — 5 min. 99212 Problem focused Problem focused Straightforward 10 min. 99213 Expanded problem focused Expanded problem focused Low complexity 15 min. 99214 Detailed Detailed Moderate complexity 25 min. 99215 Comprehensive Comprehensive High complexity 40 min. 2 of 3 required History of the Present Illness Past, Family and/or Social His- Type of History (HPI) (see page 2) Review of Systems (ROS) (see page 2) tory (PFSH) (see page 2) Problem Brief Not required Not required focused One to three elements Expanded Brief Problem pertinent Not required problem One to three elements Positive and pertinent negative responses for focused the system directly related to the problem(s) identified in the HPI. Detailed Extended Extended Pertinent Four or more elements (OR Positive and pertinent negative responses for 2 At least one specific item from status of three or more to 9 systems. the PFSH must be documented. chronic or inactive conditions) Comprehensive Extended Complete Complete Four or more elements (OR Positive and pertinent negative responses for At least one item from each of status of three or more at least 10 systems, including the one directly two areas must be documented chronic or inactive conditions) related to the problem identified in the HPI. for most services to established Systems with positive or pertinent negative patients. (At least one item from responses must be documented individually. For each of the three areas must be the remaining systems, a notation indicating documented for most services that all other systems are negative is permissible. -

UNIVERSITY of MISSOURI HEALTH CARE Neurosciences Hello and Welcome to Neurosciences at University of Missouri Health Care
UNIVERSITY OF MISSOURI HEALTH CARE Neurosciences Hello and welcome to Neurosciences at University of Missouri Health Care. We would like to take this opportunity to introduce you to our different programs and professionals, as well as highlight some of our team’s capabilities and accomplishments. Over the last several years, we have seen an increase in demand for care of patients with neurological disease — whether it be stroke, brain tumors, sleep, epilepsy, Parkinson’s Disease or another condition. As a result of these increases, our neurology and neurosurgery teams have worked together to build up existing programs; recruit new faculty, nurses and other staff; acquire new equipment and look for new approaches to improve patient access to care. Recently, our epilepsy program has been recertified as a Level IV Center – the highest rating available. Our stroke center has also been recertified as a Comprehensive Stroke Center. We now have three stroke neurologists and three endovascular providers to care for strokes, aneurysms and other vascular diseases of the brain, and new endovascular techniques are being incorporated into our armamentarium. For our patients with brain tumors, we’ve added a medical neuro-oncologist and intra-operative CT scanner, and we offer a number of clinical trials in addition to our advanced surgical procedures. Our neuroscience intensive care unit has also been expanded to 14 beds. As a part of an academic health system, we are committed to training the next generation of doctors. We offer residency programs in neurology and neurosurgery with medical students regularly rotating in on both services. We offer fellowship programs in neurocritical care, sleep medicine, clinical neurophysiology, stroke and neuroendovascular procedures. -

Specialty: Medicine – Sleep Medicine Delineation of Privileges
Final – Approved by Board of Trustees 2/14/12 NAME _____________________________________ Fort Hamilton Hospital Specialty: Medicine – Sleep Medicine Delineation of Privileges Instructions: 1. Check the Request checkbox to request all privileges in the Core group. 2. Uncheck any privileges you do not want to request in that group. 3. Check off any special privileges you want to request. 4. Sign/Date form and Submit with required documentation. Required Qualifications Education/Training/Experience To be eligible to apply for core privileges in sleep medicine, the initial applicant must meet the following criteria: Minimum formal training: Applicants must demonstrate successful completion of an ACGMS/AOA accredited postgraduate training program in a primary medical specialty such as pulmonology, psychiatry, pediatrics, otolaryngology, neurology or internal medicine. 2. Successful completion of a postgraduate sleep medicine training accredited by the AASM or ACGME, or Board Certification in Sleep Medicine. Otherwise, applicants must be able to demonstrate that they have successfully evaluated at least 400 sleep medicine patients, including 200 new patients and 200 follow-up patients, in addition to the successful interpretation/review of raw data for 200 PSGs and 25 MSLTs. 3. For new applicants to medical staff, not yet Board Certified, a letter of reference must come from the director of the applicant’s sleep medicine training program. Alternatively, a letter of reference regarding competence should come from the chief of sleep medicine at the institution where the applicant most recently practiced. Certification The applicant physician must possess current board certification by the specialty board most commonly applicable to his or her specialty, or become board certified as such within six years of completing his or her residency program or receiving medical staff membership or clinical privileges. -

Sleep Medicine Fellowship Programs
Frequently Asked Questions: Sleep Medicine Review Committee for Internal Medicine, Neurology, Pediatrics, or Psychiatry ACGME Question Answer Sponsoring Institution Is the sponsoring institution for a sleep No. Although a sponsoring institution is not required to have key faculty members and medicine fellowship required to have residencies in each of these disciplines, the program must demonstrate that fellows are residencies in family medicine, internal able to acquire the experience and knowledge from each of these disciplines as they medicine, neurology, pediatrics, and relate to the practice of sleep medicine. The Review Committee will closely examine psychiatry. whether fellows receive adequate education in all of the aforementioned disciplines. (Program Requirement: I.A.1] Can more than one sleep medicine With the exception of pediatric facilities (i.e., sleep laboratory, clinic, or hospital), program, even if from a different sponsoring facilities used by one sleep medicine program cannot be used as an essential institution, utilize the same facilities for component of another sleep medicine program. The Review Committee believes that program education? sharing of facilities will lead to dilution of the clinical experience by the host program. [Program Requirement I.A.2] In the case of pediatric facilities, the Committee recognizes that there may be a shortage of pediatric resources in certain geographical areas. Therefore, more than one sleep medicine program can utilize the same pediatric facility provided the pediatric facility can demonstrate that there is a sufficient volume of patients and/or polysomnograms to support the number of fellows utilizing the facility, and that there are adequate numbers of supervising faculty members. -

SLEEP MEDICINE? Consultations with the Center’S Medical Staff Can Be Arranged by Calling Us Directly Or Through a Referral from Your Primary Care Physician
WHAT IS A SLEEP STUDY? TESTING HOURS A sleep study is part of a comprehensive Monday through Friday: 8 a.m. – 4 p.m. evaluation of sleep problems. During a Monday through Friday: 7:30 p.m. – 8 a.m. sleep study, a patient will spend the night in a private “bedroom” at the sleep center. CONSULTATION HOURS The patient will have brain wave activity Monday, Thursday & Friday: 8:30 a.m. – 5 p.m. and body systems monitored throughout Tuesday & Wednesday: 11 a.m. – 7 p.m. the night by a technologist who remains outside the room at a control center. Most patients find it similar to sleeping in a hotel and are able to fall asleep quite easily. After a sleep study is completed, our physicians will interpret the results and prepare an individualized treatment plan. HOW DO I GET REFERRED TO THE CENTER FOR SLEEP MEDICINE? Consultations with the center’s medical staff can be arranged by calling us directly or through a referral from your primary care physician. DO CHILDREN HAVE SLEEPING DISORDERS? Sleep disorders are common among Capital Health – Hamilton children as well as adults. In children, sleep 1401 Whitehorse-Mercerville Road CENTER FOR disorder symptoms differ from adults and Suite 219 SLEEP MEDICINE are often linked to hyperactivity, poor school Hamilton, NJ 08619 performance, and ADHD. Our medical 609.584.5150 experts treat children as well as adults and Fax 609.584.5144 can evaluate and treat anyone one year of age or older. sleepatcapitalhealth.com DOES MY INSURANCE COVER A SLEEP STUDY? Sleep testing is covered by most insurances including Medicare, but you should always verify coverage with your provider ahead of time. -

Role of the Allergist-Immunologist and Upper Airway Allergy in Sleep-Disordered Breathing
AAAAI Work Group Report Role of the Allergist-Immunologist and Upper Airway Allergy in Sleep-Disordered Breathing Dennis Shusterman, MD, MPHa, Fuad M. Baroody, MDb, Timothy Craig, DOc, Samuel Friedlander, MDd, Talal Nsouli, MDe, and Bernard Silverman, MD, MPHf; on behalf of the American Academy of Allergy, Asthma & Immunology’s Rhinitis, Rhinosinusitis and Ocular Allergy Committee Work Group on Rhinitis and Sleep-disordered Breathing San Francisco, Calif; Chicago, Ill; Hershey, Pa; Solon, Ohio; Washington, DC; and Brooklyn, NY BACKGROUND: Sleep-disordered breathing in general and RESULTS: Survey results were returned by 339 of 4881 active obstructive sleep apnea in particular are commonly encountered members (7%). More than two-third of respondents routinely conditions in allergy practice. Physiologically, nasal (or asked about sleep problems, believed that sleep-disordered nasopharyngeal) obstruction from rhinitis, nasal polyposis, or breathing was a problem for at least a “substantial minority” adenotonsillar hypertrophy are credible contributors to snoring (10%-30%) of their adult patients, and believed that medical and nocturnal respiratory obstructive events. Nevertheless, therapy for upper airway inflammatory conditions could existing practice parameters largely relegate the role of the potentially help ameliorate sleep-related complaints. Literature allergist to adjunctive treatment in cases of continuous positive review supported the connection between high-grade nasal airway pressure intolerance. congestion/adenotonsillar hypertrophy and obstructive sleep OBJECTIVES: To survey active American Academy of Allergy, apnea, and at least in the case of pediatric patients, supported the Asthma & Immunology members regarding their perceptions use of anti-inflammatory medication in the initial management and practices concerning sleep-disordered breathing in adult and of obstructive sleep apnea of mild-to-moderate severity. -

SLEEP MEDICINE Official Journal of the World Sleep Society and International Pediatric Sleep Association
SLEEP MEDICINE Official Journal of the World Sleep Society and International Pediatric Sleep Association AUTHOR INFORMATION PACK TABLE OF CONTENTS XXX . • Description p.1 • Audience p.1 • Impact Factor p.1 • Abstracting and Indexing p.2 • Editorial Board p.2 • Guide for Authors p.4 ISSN: 1389-9457 DESCRIPTION . Sleep Medicine has an open access mirror journal Sleep Medicine: X which has the same aims and scope, editorial board and peer-review process. To submit to Sleep Medicine: X visit https://www.editorialmanager.com/SLEEPX/default.aspx. Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without. A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry. The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites. Benefits to authors We also provide many author benefits, such as free PDFs, a liberal copyright policy, special discounts on Elsevier publications and much more. Please click here for more information on our author services. Please see our Guide for Authors for information on article submission. If you require any further information or help, please visit our Support Center AUDIENCE . Neurologists, clinical neurophysiologists, psychologists, psychiatrists, internists, particularly pulmonologists, cardiologists, gastroenterologists, nephrologists; sleep technologists, pediatricians, family physicians, otolaryngologists.