E&M Documentation—Key Components
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

Heart Failure
Heart Failure Sandra Keavey, DHSc, PAC, DFAAPA Defined Heart failure (HF) is a common clinical syndrome resulting from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood. HF may be caused by disease of the myocardium, pericardium, endocardium, heart valves, vessels, or by metabolic disorders Epidemiology-Magnitude Heart failure disproportionately affects the older population. Approximately 80% of all cases of heart failure in the United States occur in persons aged 65 years and older. In the older population, heart failure accounts for more hospital admissions than any other single condition. Following hospitalization for heart failure, nearly half are readmitted within 6 months. Epidemiology-Prevalence Prevalence. About 5.1 million people in the United States have heart failure. One in 9 deaths in 2009 included heart failure as contributing cause. About half of people who develop heart failure die within 5 years of diagnosis. 25% of all heart failure patients are re-admitted to the hospital within 30 days. 50% of all heart failure patients are re-admitted to the hospital within 6 months. Systolic vs Diastolic There are two common types of heart failure Systolic HF Systolic HF is the most common type of HF Now referred to as HFrEF Heart Failure reduced Ejection Fraction The heart is weak and enlarged. The muscle of the left ventricle loses some of its ability to contract or shorten. Diastolic HF Diastolic HF is not an isolated disorder of diastole; there are widespread abnormalities of both systolic and diastolic function that become more apparent with exercise. -

Medical Terminology Abbreviations Medical Terminology Abbreviations
34 MEDICAL TERMINOLOGY ABBREVIATIONS MEDICAL TERMINOLOGY ABBREVIATIONS The following list contains some of the most common abbreviations found in medical records. Please note that in medical terminology, the capitalization of letters bears significance as to the meaning of certain terms, and is often used to distinguish terms with similar acronyms. @—at A & P—anatomy and physiology ab—abortion abd—abdominal ABG—arterial blood gas a.c.—before meals ac & cl—acetest and clinitest ACLS—advanced cardiac life support AD—right ear ADL—activities of daily living ad lib—as desired adm—admission afeb—afebrile, no fever AFB—acid-fast bacillus AKA—above the knee alb—albumin alt dieb—alternate days (every other day) am—morning AMA—against medical advice amal—amalgam amb—ambulate, walk AMI—acute myocardial infarction amt—amount ANS—automatic nervous system ant—anterior AOx3—alert and oriented to person, time, and place Ap—apical AP—apical pulse approx—approximately aq—aqueous ARDS—acute respiratory distress syndrome AS—left ear ASA—aspirin asap (ASAP)—as soon as possible as tol—as tolerated ATD—admission, transfer, discharge AU—both ears Ax—axillary BE—barium enema bid—twice a day bil, bilateral—both sides BK—below knee BKA—below the knee amputation bl—blood bl wk—blood work BLS—basic life support BM—bowel movement BOW—bag of waters B/P—blood pressure bpm—beats per minute BR—bed rest MEDICAL TERMINOLOGY ABBREVIATIONS 35 BRP—bathroom privileges BS—breath sounds BSI—body substance isolation BSO—bilateral salpingo-oophorectomy BUN—blood, urea, nitrogen -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Review of Systems – Return Visit Have You Had Any Problems Related to the Following Symptoms in the Past Month? Circle Yes Or No
REVIEW OF SYSTEMS – RETURN VISIT HAVE YOU HAD ANY PROBLEMS RELATED TO THE FOLLOWING SYMPTOMS IN THE PAST MONTH? CIRCLE YES OR NO Today’s Date: ______________ Name: _______________________________ Date of Birth: __________________ GENERAL GENITOURINARY Fatigue Y N Blood in Urine Y N Fever / Chills Y N Menstrual Irregularity Y N Night Sweats Y N Painful Menstrual Cycle Y N Weight Gain Y N Vaginal Discharge Y N Weight Loss Y N Vaginal Dryness Y N EYES Vaginal Itching Y N Vision Changes Y N Painful Sex Y N EAR, NOSE, & THROAT SKIN Hearing Loss Y N Hair Loss Y N Runny Nose Y N New Skin Lesions Y N Ringing in Ears Y N Rash Y N Sinus Problem Y N Pigmentation Change Y N Sore Throat Y N NEUROLOGIC BREAST Headache Y N Breast Lump Y N Muscular Weakness Y N Tenderness Y N Tingling or Numbness Y N Nipple Discharge Y N Memory Difficulties Y N CARDIOVASCULAR MUSCULOSKELETAL Chest Pain Y N Back Pain Y N Swelling in Legs Y N Limitation of Motion Y N Palpitations Y N Joint Pain Y N Fainting Y N Muscle Pain Y N Irregular Heart Beat Y N ENDOCRINE RESPIRATORY Cold Intolerance Y N Cough Y N Heat Intolerance Y N Shortness of Breath Y N Excessive Thirst Y N Post Nasal Drip Y N Excessive Amount of Urine Y N Wheezing Y N PSYCHOLOGY GASTROINTESTINAL Difficulty Sleeping Y N Abdominal Pain Y N Depression Y N Constipation Y N Anxiety Y N Diarrhea Y N Suicidal Thoughts Y N Hemorrhoids Y N HEMATOLOGIC / LYMPHATIC Nausea Y N Easy Bruising Y N Vomiting Y N Easy Bleeding Y N GENITOURINARY Swollen Lymph Glands Y N Burning with Urination Y N ALLERGY / IMMUNOLOGY Urinary -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Signs and Symptoms
Signs and Symptoms Some abnormal heart rhythms can happen without the person knowing it, while some may cause a feeling of the heart “racing,” lightheadedness, or dizziness. At some point in life, many adults Rapid Heartbeat – Tachycardia have had short-lived heart rhythm When the heart beats too quickly changes that are not serious. (usually above 100 beats per minute), the lower chambers, or Certain heart rhythms, especially ventricles, do not have enough time those that last long enough to af - to fill with blood, so they cannot ef - fect the heart’s function, can be fectively pump blood to the rest of serious or even deadly. the body. When this happens, some Palpitation or Skipped Beat people have symptoms such as: Although it may seem as if the Skipping a beat Slow Heartbeat – Bradycardia heart missed a beat, it has really had an early heartbeat — an extra If the heartbeat is too slow (usually Beating out of rhythm below 60 beats per minute), not beat that happens before the heart Palpitations has a chance to fill with blood. enough blood carrying oxygen Fast or racing heartbeat Therefore the squeeze is empty flows through the body. The symptoms of a slow heartbeat are: and results in a pause. Shortness of breath Fatigue (feeling tired) Fluttering Chest pain A fluttering sensation (like butter - Dizziness Dizziness flies in the chest) is usually due to Lightheadedness extra or “skipped beats” that occur Lightheadedness Fainting or near fainting one right after the other, or may be Fainting or near fainting caused by other kinds of abnormal heart rhythms. -
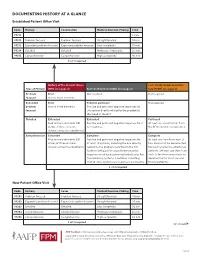
Documenting History at a Glance
DOCUMENTING HISTORY AT A GLANCE Established Patient Office Visit Code History Examination Medical Decision-Making Time 99211 — — — 5 min. 99212 Problem focused Problem focused Straightforward 10 min. 99213 Expanded problem focused Expanded problem focused Low complexity 15 min. 99214 Detailed Detailed Moderate complexity 25 min. 99215 Comprehensive Comprehensive High complexity 40 min. 2 of 3 required History of the Present Illness Past, Family and/or Social His- Type of History (HPI) (see page 2) Review of Systems (ROS) (see page 2) tory (PFSH) (see page 2) Problem Brief Not required Not required focused One to three elements Expanded Brief Problem pertinent Not required problem One to three elements Positive and pertinent negative responses for focused the system directly related to the problem(s) identified in the HPI. Detailed Extended Extended Pertinent Four or more elements (OR Positive and pertinent negative responses for 2 At least one specific item from status of three or more to 9 systems. the PFSH must be documented. chronic or inactive conditions) Comprehensive Extended Complete Complete Four or more elements (OR Positive and pertinent negative responses for At least one item from each of status of three or more at least 10 systems, including the one directly two areas must be documented chronic or inactive conditions) related to the problem identified in the HPI. for most services to established Systems with positive or pertinent negative patients. (At least one item from responses must be documented individually. For each of the three areas must be the remaining systems, a notation indicating documented for most services that all other systems are negative is permissible. -

Arrhythmia What Is It?
Arrhythmia What is it? Most of us have felt our heart race or skip a beat. It’s fairly normal every once and a while. But for some people, it’s a sign of arrhythmia – a disorder of your heart rate or rhythm – that needs to be checked out by a specialist. If you have an arrhythmia (there are multiple types), your heart either beats: • too fast • too slow or • with an irregular pattern Did You Know? This change in your heart rhythm is usually caused by a “glitch” Our heart beats an average of in your heart’s electrical activity, which tells the heart when to 70 to 80 times a minute and contract and pump blood to the body. Your heart doesn’t beat over 100,000 times a day! It’s with the regularity of a Swiss watch, and many factors can cause no wonder millions of people an irregularity. notice palpitations such as skipping a beat, fluttering or a Some of these factors include: racing heart. • having had a heart attack • having heart failure • blood chemistry imbalances • abnormal hormone levels • alcohol, caffeine and other substances or medicines • a variety of inherited abnormalities 8 Tips for Staying Heart Healthy with Arrhythmias Living with an arrhythmia varies tremendously from one person to the next. It will depend on the type of arrhythmia you have, how serious it is and the recommended treatment. Some people can take a single medication to correct their heart’s rhythm; others undergo electrophysiology studies or require a pacemaker or implantable defibrillator. No matter what kind of arrhythmia you have, there are things you can do to keep your heart healthy and ticking as it should. -

Sleep Medicine Curriculum for Neurology Residents
Sleep Medicine Curriculum for Neurology Residents This curriculum, developed in collaboration with the AAN Consortium of Neurology Program Directors and Graduate Education Subcommittee, provides a comprehensive outline of the relevant educational goals for the future generation of adult neurologists learning sleep medicine during residency. The clinical scope of this curriculum is common and uncommon sleep disorders encountered in typical neurology practices. While the all-encompassing scope of this outline covers more than is expected to be learned by neurology residents on a given subspecialty rotation, the measurable objectives are included to provide program directors and other rotation developers the means of evaluating whether a minimum competence in sleep was attained in any combination of specific areas. Finally, as sleep medicine is a cross-disciplinary neurologic subspecialty, the curriculum ends with a table highlighting overlapping conditions between major sleep disorder categories and neurologic subspecialities. Authors: Lead Author Logan Schneider, MD [email protected] Stanford/VA Alzheimer’s Center Alon Avidan, MD, MPH, FAAN David Geffen School of Medicine at UCLA Muna Irfan, MD University of Minnesota Meena Khan, MD The Ohio State University Created: January 2020 Effective: February 2020 to February 2021 Approved by the American Academy of Neurology’s Graduate Education Subcommittee Sleep Medicine Curriculum for Neurology Residents Part I. General Clinical Approach Clinical evaluation: History Efficiently obtains a complete, relevant, and organized neurologic history Performs comprehensive review of systems pertinent to ICSD-3 sleep-wake disorder categories (sleep-related disordered breathing, hypersomnias, insomnias, parasomnias, sleep-related movement disorders, circadian disorders) Performs comprehensive review of systems probing medical conditions that are known to impact sleep-wake disorders (e.g. -

Review of Systems Health History Sheet Patient: ______DOB: ______Age: ______Gender: M / F
603 28 1/4 Road Grand Junction, CO 81506 (970) 263-2600 Review of Systems Health History Sheet Patient: _________________ DOB: ____________ Age: ______ Gender: M / F Please mark any symptoms you are experiencing that are related to your complaint today: Allergic/ Immunologic Ears/Nose/Mouth/Throat Genitourinary Men Only Frequent Sneezing Bleeding Gums Pain with Urinating Pain/Lump in Testicle Hives Difficulty Hearing Blood in Urine Penile Itching, Itching Dizziness Difficulty Urinating Burning or Discharge Runny Nose Dry Mouth Incomplete Emptying Problems Stopping or Sinus Pressure Ear Pain Urinary Frequency Starting Urine Stream Cardiovascular Frequent Infections Loss of Urinary Control Waking to Urinate at Chest Pressure/Pain Frequent Nosebleeds Hematologic / Lymphatic Night Chest Pain on Exertion Hoarseness Easy Bruising / Bleeding Sexual Problems / Irregular Heart Beats Mouth Breathing Swollen Glands Concerns Lightheaded Mouth Ulcers Integumentary (Skin) History of Sexually Swelling (Edema) Nose/Sinus Problems Changes in Moles Transmitted Diseases Shortness of Breath Ringing in Ears Dry Skin Women Only When Lying Down Endocrine Eczema Bleeding Between Shortness of Breath Increased Thirst / Growth / Lesions Periods When Walking Urination Itching Heavy Periods Constitutional Heat/Cold Intolerance Jaundice (Yellow Extreme Menstrual Pain Exercise Intolerance Gastrointestinal Skin or Eyes) Vaginal Itching, Fatigue Abdominal Pain Rash Burning or Discharge Fever Black / Tarry Stool Respiratory Waking to Urinate at Weight Gain (___lbs) Blood -

Running Head: COLORECTAL CANCER SCREENING 1
Running head: COLORECTAL CANCER SCREENING 1 COLORECTAL CANCER SCREENING IN A LARGE HEALTHCARE ORGANIZATION by Torica Todai Fuller Paper submitted in partial fulfillment of the requirements for the degree of Doctor of Nursing Practice East Carolina University College of Nursing July 22, 2019 COLORECTAL CANCER SCREENING 2 Acknowledgments First, I would like to give ALL Thanks and Praises to GOD who is the head of my life. I would like to thank Him for ordering my steps and leading me back to East Carolina University. As an adult student, I have grown and matured both professionally and spiritually. This learning experience has taught me to become a better person and better provider. Even with juggling my career, being a pastor’s wife and also a student, God still showed Himself strong in my life and I am truly thankful and honored to be used by God. This was a test, but it is now my testimony. My favorite scripture is: “I can do ALL things through CHRIST who strengthens ME” (Philippians 4:13). The journey has been filled with new friendships which have also blossomed into a tight- knit cohort family. Moreover, I am grateful to all for every word of encouragement and support. I would like to thank my colleagues for their support, Dr. Lori Haigler, the Interim Medical Director, Dr. Lan Tran-Phu, Dr. Krystle Vinson, my Site Champion, and Mr. Duane Holder, the Interim Health Director. As I close and reflect back on the last twenty-four months, I would like to applaud and thank Dr. Tracey Robertson-Bell, my DNP advisor for her words of encouragement, unwavering support and professional guidance.