Acute Abdomen
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

Acute Abdomen
Acute abdomen: Shaking down the Acute abdominal pain can be difficult to diagnose, requiring astute assessment skills and knowledge of abdominal anatomy 2.3 ANCC to discover its cause. We show you how to quickly and accurately CONTACT HOURS uncover the clues so your patient can get the help he needs. By Amy Wisniewski, BSN, RN, CCM Lehigh Valley Home Care • Allentown, Pa. The author has disclosed that she has no significant relationships with or financial interest in any commercial companies that pertain to this educational activity. NIE0110_124_CEAbdomen.qxd:Deepak 26/11/09 9:38 AM Page 43 suspects Determining the cause of acute abdominal rapidly, indicating a life-threatening process, pain is often complex due to the many or- so fast and accurate assessment is essential. gans in the abdomen and the fact that pain In this article, I’ll describe how to assess a may be nonspecific. Acute abdomen is a patient with acute abdominal pain and inter- general diagnosis, typically referring to se- vene appropriately. vere abdominal pain that occurs suddenly over a short period (usually no longer than What a pain! 7 days) and often requires surgical interven- Acute abdominal pain is one of the top tion. Symptoms may be severe and progress three symptoms of patients presenting in www.NursingMadeIncrediblyEasy.com January/February 2010 Nursing made Incredibly Easy! 43 NIE0110_124_CEAbdomen.qxd:Deepak 26/11/09 9:38 AM Page 44 the ED. Reasons for acute abdominal pain Visceral pain can be divided into three Your patient’s fall into six broad categories: subtypes: age may give • inflammatory—may be a bacterial cause, • tension pain. -

Missed Appendicitis Diagnosis: a Case Report Jocelyn Cox, Bphed, DC1 Guy Sovak, Phd2
ISSN 0008-3194 (p)/ISSN 1715-6181 (e)/2015/294–299/$2.00/©JCCA 2015 Missed appendicitis diagnosis: A case report Jocelyn Cox, BPhEd, DC1 Guy Sovak, PhD2 Objective: The purpose of this case report is to highlight Objectif : Cette étude de cas vise à souligner la nécessité and emphasize the need for an appropriate and thorough d’une liste appropriée et détaillée de diagnostics list of differential diagnoses when managing patients, as différentiels lors de la gestion des patients, car il n’est it is insufficient to assume cases are mechanical, until pas suffisant de supposer que les cas sont d’ordre proven non-mechanical. There are over 250,000 cases mécanique, jusqu’à la preuve du contraire. Il y a plus de of appendicitis annually in the United States. Of these 250 000 cas d’appendicite par an aux États-Unis. Parmi cases, <50% present with classic signs and symptoms of ces cas, < 50 % présentent des signes et des symptômes pain in the right lower quadrant, mild fever and nausea. classiques de douleur dans le quadrant inférieur droit, It is standard for patients who present with appendicitis de fièvre légère et de nausées. Il est normal qu’un to be managed operatively with a laparoscopic patient qui se présente avec une appendicite soit géré appendectomy within 24 hours, otherwise the risk of par une intervention chirurgicale (appendicectomie complications such as rupture, infection, and even death par laparoscopie) dans les 24 heures, sinon le risque increases dramatically. de complications, telles que rupture, infection et décès, Clinical Features: This is a retrospective case report augmente considérablement. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Review of Systems – Return Visit Have You Had Any Problems Related to the Following Symptoms in the Past Month? Circle Yes Or No
REVIEW OF SYSTEMS – RETURN VISIT HAVE YOU HAD ANY PROBLEMS RELATED TO THE FOLLOWING SYMPTOMS IN THE PAST MONTH? CIRCLE YES OR NO Today’s Date: ______________ Name: _______________________________ Date of Birth: __________________ GENERAL GENITOURINARY Fatigue Y N Blood in Urine Y N Fever / Chills Y N Menstrual Irregularity Y N Night Sweats Y N Painful Menstrual Cycle Y N Weight Gain Y N Vaginal Discharge Y N Weight Loss Y N Vaginal Dryness Y N EYES Vaginal Itching Y N Vision Changes Y N Painful Sex Y N EAR, NOSE, & THROAT SKIN Hearing Loss Y N Hair Loss Y N Runny Nose Y N New Skin Lesions Y N Ringing in Ears Y N Rash Y N Sinus Problem Y N Pigmentation Change Y N Sore Throat Y N NEUROLOGIC BREAST Headache Y N Breast Lump Y N Muscular Weakness Y N Tenderness Y N Tingling or Numbness Y N Nipple Discharge Y N Memory Difficulties Y N CARDIOVASCULAR MUSCULOSKELETAL Chest Pain Y N Back Pain Y N Swelling in Legs Y N Limitation of Motion Y N Palpitations Y N Joint Pain Y N Fainting Y N Muscle Pain Y N Irregular Heart Beat Y N ENDOCRINE RESPIRATORY Cold Intolerance Y N Cough Y N Heat Intolerance Y N Shortness of Breath Y N Excessive Thirst Y N Post Nasal Drip Y N Excessive Amount of Urine Y N Wheezing Y N PSYCHOLOGY GASTROINTESTINAL Difficulty Sleeping Y N Abdominal Pain Y N Depression Y N Constipation Y N Anxiety Y N Diarrhea Y N Suicidal Thoughts Y N Hemorrhoids Y N HEMATOLOGIC / LYMPHATIC Nausea Y N Easy Bruising Y N Vomiting Y N Easy Bleeding Y N GENITOURINARY Swollen Lymph Glands Y N Burning with Urination Y N ALLERGY / IMMUNOLOGY Urinary -

A RISK MANAGEMENT APPROACH to ABDOMINAL PAIN in PRIMARY CARE Symptoms Most Predictive of Appendicitis Are Right Lower Torsion
EMERGENCY MEDICINE – WHAT THE FAMILY PHYSICIAN CAN TREAT UNIT NO. 6 A RISK MANAGEMENT APPROACH TO ABDOMINAL PAIN IN PRIMARY CARE Symptoms most predictive of appendicitis are right lower torsion. inammatory disease (PID) and appendicitis can be virtually for a patient with abdominal pain yields little information, aneurysm or a dissection in elderly patients presenting with quadrant pain (RLQ), and migration of pain from the indistinguishable via the anterior abdominal examination, and unless one is specically looking for air-uid levels indicative of ank pain. Up to one-third of patients with abdominal aortic SUMMARY Dr Lim Jia Hao periumbilical region to RLQ. Anorexia, which has been Palpation should begin with light palpation to localise the it will be the pelvic examination that can reveal the true intestinal obstruction in a patient exhibiting obstructive aneurysms may have haematuria, which can further confound classically taught to be useful in diagnosing appendicitis has region of tenderness and to elicit guarding. Deep palpation aetiology. While both conditions can result in painful cervical symptoms. Abnormal calcications associated with gallstone the physician. Detection of vascular emergencies can be dicult e assessment of abdominal pain in the primary healthcare been found to have little predictive value.6, 7 A gynaecological follows for the detection of organomegaly and masses. However, motion and adnexal tenderness, it is the presence of disease, kidney stones, appendicoliths, as well as aortic if the diagnosis is not entertained from the outset. setting will require the family physician to employ the ABSTRACT just as important to recognise the patients that require a referral and sexual history should be obtained when evaluating women, this can be deeply distressing to the patient with severe mucopurulent discharge from the cervix that will allow the calcications can sometimes be seen on the plain lm as well. -
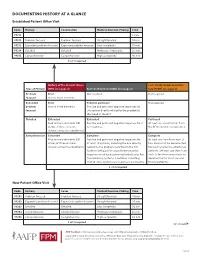
Documenting History at a Glance
DOCUMENTING HISTORY AT A GLANCE Established Patient Office Visit Code History Examination Medical Decision-Making Time 99211 — — — 5 min. 99212 Problem focused Problem focused Straightforward 10 min. 99213 Expanded problem focused Expanded problem focused Low complexity 15 min. 99214 Detailed Detailed Moderate complexity 25 min. 99215 Comprehensive Comprehensive High complexity 40 min. 2 of 3 required History of the Present Illness Past, Family and/or Social His- Type of History (HPI) (see page 2) Review of Systems (ROS) (see page 2) tory (PFSH) (see page 2) Problem Brief Not required Not required focused One to three elements Expanded Brief Problem pertinent Not required problem One to three elements Positive and pertinent negative responses for focused the system directly related to the problem(s) identified in the HPI. Detailed Extended Extended Pertinent Four or more elements (OR Positive and pertinent negative responses for 2 At least one specific item from status of three or more to 9 systems. the PFSH must be documented. chronic or inactive conditions) Comprehensive Extended Complete Complete Four or more elements (OR Positive and pertinent negative responses for At least one item from each of status of three or more at least 10 systems, including the one directly two areas must be documented chronic or inactive conditions) related to the problem identified in the HPI. for most services to established Systems with positive or pertinent negative patients. (At least one item from responses must be documented individually. For each of the three areas must be the remaining systems, a notation indicating documented for most services that all other systems are negative is permissible. -

Acute Abdomen in the Emergency Department
IAJPS 2018, 05 (11), 11847-11852 Muhanad Khalid Kondarji et al ISSN 2349-7750 CODEN [USA]: IAJPBB ISSN: 2349-7750 INDO AMERICAN JOURNAL OF PHARMACEUTICAL SCIENCES Available online at: http://www.iajps.com Review Article ACUTE ABDOMEN IN THE EMERGENCY DEPARTMENT Muhanad Khalid Kondarji1, Mohammed Khalid Kondarji2, Abdullah Mohammed Alzahrani1, Hussa Ali Alrashid2, Turki Ghaleb Al Ahmadi1, Faisal Mohammed Hinkish3, Fisal Amjed Abdulaziz4, Hamoud Marzuq Alrougi1, Rayan Tareq Alrefai1, Hassan Ibrahim Alasmari1 1 King Fahd Hospital, Jeddah 2 King Abdulaziz University 3 Althaghr Hospital 4 Taibah University Abstract: Introduction: 7% of the patients come to the emergency department with the chief complain of acute abdominal pain. They can have minor causes, but also be due to very serious causes, which requires urgency in care and serious diagnosis and management. Acute abdominal emergencies are a big contributor to morbidity and mortality. Aim of the work: In this study, we aim to understand the standard way to approach a case of acute abdominal pain in the emergency department. Methodology: we conducted this review using a comprehensive search of MEDLINE, PubMed and EMBASE from January 1970 to March 2017. The following search terms were used: acute abdomen, abdominal pain management, clinical evaluation of abdominal pain, management acute abdomen Conclusion: Acute abdomen is an extremely common presentation in the emergency department. However, it is not easy to assess, diagnose, and manage. Rate of misdiagnoses and fatalities are high; therefore, physicians should always consider all possible and start with more serious etiologies. Proper assessment and management of acute abdomen can lead to significant improvement of morbidity and mortality. -

Sleep Medicine Curriculum for Neurology Residents
Sleep Medicine Curriculum for Neurology Residents This curriculum, developed in collaboration with the AAN Consortium of Neurology Program Directors and Graduate Education Subcommittee, provides a comprehensive outline of the relevant educational goals for the future generation of adult neurologists learning sleep medicine during residency. The clinical scope of this curriculum is common and uncommon sleep disorders encountered in typical neurology practices. While the all-encompassing scope of this outline covers more than is expected to be learned by neurology residents on a given subspecialty rotation, the measurable objectives are included to provide program directors and other rotation developers the means of evaluating whether a minimum competence in sleep was attained in any combination of specific areas. Finally, as sleep medicine is a cross-disciplinary neurologic subspecialty, the curriculum ends with a table highlighting overlapping conditions between major sleep disorder categories and neurologic subspecialities. Authors: Lead Author Logan Schneider, MD [email protected] Stanford/VA Alzheimer’s Center Alon Avidan, MD, MPH, FAAN David Geffen School of Medicine at UCLA Muna Irfan, MD University of Minnesota Meena Khan, MD The Ohio State University Created: January 2020 Effective: February 2020 to February 2021 Approved by the American Academy of Neurology’s Graduate Education Subcommittee Sleep Medicine Curriculum for Neurology Residents Part I. General Clinical Approach Clinical evaluation: History Efficiently obtains a complete, relevant, and organized neurologic history Performs comprehensive review of systems pertinent to ICSD-3 sleep-wake disorder categories (sleep-related disordered breathing, hypersomnias, insomnias, parasomnias, sleep-related movement disorders, circadian disorders) Performs comprehensive review of systems probing medical conditions that are known to impact sleep-wake disorders (e.g. -

Review of Systems Health History Sheet Patient: ______DOB: ______Age: ______Gender: M / F
603 28 1/4 Road Grand Junction, CO 81506 (970) 263-2600 Review of Systems Health History Sheet Patient: _________________ DOB: ____________ Age: ______ Gender: M / F Please mark any symptoms you are experiencing that are related to your complaint today: Allergic/ Immunologic Ears/Nose/Mouth/Throat Genitourinary Men Only Frequent Sneezing Bleeding Gums Pain with Urinating Pain/Lump in Testicle Hives Difficulty Hearing Blood in Urine Penile Itching, Itching Dizziness Difficulty Urinating Burning or Discharge Runny Nose Dry Mouth Incomplete Emptying Problems Stopping or Sinus Pressure Ear Pain Urinary Frequency Starting Urine Stream Cardiovascular Frequent Infections Loss of Urinary Control Waking to Urinate at Chest Pressure/Pain Frequent Nosebleeds Hematologic / Lymphatic Night Chest Pain on Exertion Hoarseness Easy Bruising / Bleeding Sexual Problems / Irregular Heart Beats Mouth Breathing Swollen Glands Concerns Lightheaded Mouth Ulcers Integumentary (Skin) History of Sexually Swelling (Edema) Nose/Sinus Problems Changes in Moles Transmitted Diseases Shortness of Breath Ringing in Ears Dry Skin Women Only When Lying Down Endocrine Eczema Bleeding Between Shortness of Breath Increased Thirst / Growth / Lesions Periods When Walking Urination Itching Heavy Periods Constitutional Heat/Cold Intolerance Jaundice (Yellow Extreme Menstrual Pain Exercise Intolerance Gastrointestinal Skin or Eyes) Vaginal Itching, Fatigue Abdominal Pain Rash Burning or Discharge Fever Black / Tarry Stool Respiratory Waking to Urinate at Weight Gain (___lbs) Blood -

Running Head: COLORECTAL CANCER SCREENING 1
Running head: COLORECTAL CANCER SCREENING 1 COLORECTAL CANCER SCREENING IN A LARGE HEALTHCARE ORGANIZATION by Torica Todai Fuller Paper submitted in partial fulfillment of the requirements for the degree of Doctor of Nursing Practice East Carolina University College of Nursing July 22, 2019 COLORECTAL CANCER SCREENING 2 Acknowledgments First, I would like to give ALL Thanks and Praises to GOD who is the head of my life. I would like to thank Him for ordering my steps and leading me back to East Carolina University. As an adult student, I have grown and matured both professionally and spiritually. This learning experience has taught me to become a better person and better provider. Even with juggling my career, being a pastor’s wife and also a student, God still showed Himself strong in my life and I am truly thankful and honored to be used by God. This was a test, but it is now my testimony. My favorite scripture is: “I can do ALL things through CHRIST who strengthens ME” (Philippians 4:13). The journey has been filled with new friendships which have also blossomed into a tight- knit cohort family. Moreover, I am grateful to all for every word of encouragement and support. I would like to thank my colleagues for their support, Dr. Lori Haigler, the Interim Medical Director, Dr. Lan Tran-Phu, Dr. Krystle Vinson, my Site Champion, and Mr. Duane Holder, the Interim Health Director. As I close and reflect back on the last twenty-four months, I would like to applaud and thank Dr. Tracey Robertson-Bell, my DNP advisor for her words of encouragement, unwavering support and professional guidance. -

Abdominal Pain
10 Abdominal Pain Adrian Miranda Acute abdominal pain is usually a self-limiting, benign condition that irritation, and lateralizes to one of four quadrants. Because of the is commonly caused by gastroenteritis, constipation, or a viral illness. relative localization of the noxious stimulation to the underlying The challenge is to identify children who require immediate evaluation peritoneum and the more anatomically specific and unilateral inner- for potentially life-threatening conditions. Chronic abdominal pain is vation (peripheral-nonautonomic nerves) of the peritoneum, it is also a common complaint in pediatric practices, as it comprises 2-4% usually easier to identify the precise anatomic location that is produc- of pediatric visits. At least 20% of children seek attention for chronic ing parietal pain (Fig. 10.2). abdominal pain by the age of 15 years. Up to 28% of children complain of abdominal pain at least once per week and only 2% seek medical ACUTE ABDOMINAL PAIN attention. The primary care physician, pediatrician, emergency physi- cian, and surgeon must be able to distinguish serious and potentially The clinician evaluating the child with abdominal pain of acute onset life-threatening diseases from more benign problems (Table 10.1). must decide quickly whether the child has a “surgical abdomen” (a Abdominal pain may be a single acute event (Tables 10.2 and 10.3), a serious medical problem necessitating treatment and admission to the recurring acute problem (as in abdominal migraine), or a chronic hospital) or a process that can be managed on an outpatient basis. problem (Table 10.4). The differential diagnosis is lengthy, differs from Even though surgical diagnoses are fewer than 10% of all causes of that in adults, and varies by age group.