Berkshire Adult Palliative Care Guidelines Best Practice Document
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BERKSHIRE PROSPECTUS AMBITION, COLLABORATION and GROWTH Thames Valley Berkshire LEP Berkshire Prospectus Local Authorities As Well As Other Key Stakeholders
BERKSHIRE PROSPECTUS AMBITION, COLLABORATION AND GROWTH 02 THE BERKSHIRE Berkshire Prospectus Berkshire PROSPECTUS THE OPPORTUNITIES IN THIS PROSPECTUS It is no coincidence that this prospectus for Berkshire has been released in tandem with the Thames Valley Berkshire Local Enterprise Partnership (LEP) Recovery and REPRESENT A CHANCE Renewal Plan. The two documents sit alongside each other, evidencing the formidable collaborative nature of how TO RESET POST COVID the LEP is working in partnership with the six Berkshire Local Authorities as well as other key stakeholders. AND MAKE BERKSHIRE This prospectus clearly identifies several key schemes and projects which, when delivered, will greatly enhance Berkshire’s appeal as a place to live and EVEN BETTER work in the years ahead. The projects highlighted in this prospectus represent unique opportunities for new investment that will appeal to a wide range of partners, locally, regionally and nationally. The LEP and Local Authorities will work alongside private and public sector colleagues to facilitate the development and successful delivery of these great opportunities. COLLABORATIVE WORKING We should highlight the constructive partnership between the Local Authorities and the LEP, who together have forged a great working relationship with One Public Estate (OPE). Established in 2013, OPE now works nationally with more than 300 councils.These projects are transforming local communities and public services right across the country. They provide technical support and funding to councils to deliver ambitious property and place-focused programmes in collaboration with central government and other public sector partners. Thames Valley Berkshire LEP Berkshire Thames Valley 03 As highlighted in the Recovery and Renewal Plan, Thames Valley Berkshire is more than the sum of its parts. -

Berkshire Local Aggregate Assessment 2014 and 2015
Berkshire Unitary Authorities Local Aggregate Assessments 2014 and 2015 (2005-2014 & 2006-2015) Draft Report August 2016 5125072\Berkshire Local Aggregate Assessment 2014 & 2015 FINAL REPORT rev.2R2 Berkshire Unitary Authorities Local Aggregate Assessments 2014 and 2015 (2005-2014 & 2006-2015) Final Report August 2016 Notice This report was produced by Atkins Ltd. for the Berkshire Unitary Authorities for the specific purpose of undertaking a Local Aggregate Assessment. This report may not be used by any person other than the Berkshire Unitary Authorities without its express permission. In any event, Atkins Ltd accepts no liability for any costs, liabilities or losses arising as a result of the use of or reliance upon the contents of this report by any person other than its Client. Document History JOB NUMBER: 5125072 DOCUMENT REF: Berkshire Local Aggregate Assessments 2014 and 2015 R2 Revision Purpose Description Originated Checked Reviewed Authorised Date 0 Draft Report KR CM AH AH 11.05.16 1 Final Report KR MM AH AH 6.07.16 2 Updated Final Report KR MM AH AH 3.08.16 5125072\Berkshire Local Aggregate Assessment 2014 & 2015 FINAL REPORT rev.2R2 Berkshire Unitary Authorities Local Aggregate Assessments 2014 and 2015 Contents Section Page 1. Introduction 1 Project Brief 1 Purpose of the Assessment 1 Background to the Managed Aggregate Supply System 1 Methodology 2 2. Aggregates in Berkshire 4 Geology of Berkshire and Current Mineral Working 4 Assessment of Berkshire’s Available Mineral Resources 8 Assessment of Available Mineral Resources in Berkshire’s Neighbouring Areas 9 Key Points 10 3. Past and Current Supply of Aggregates in Berkshire 12 Sand and Gravel 12 Exports, Imports and Consumption of Primary Aggregates 17 Recycled and Secondary Aggregates 20 Key Points 23 4. -

Relocate to West Berkshire
Kennet School Excellence through Endeavour Relocate to West Berkshire Thatcham is the oldest continuously inhabited settlement in Britain. It is situated on the River Kennet and the Kennet and Avon Canal. A historic market town in origin, the centre of Thatcham is made up of a small high street including supermarkets, pubs, restaurants and other local amenities. Situated 3 miles from Newbury, 14 miles West of Reading and 54 miles West of London, Thatcham proves an ideal place of residence for those who have an interest in City visits/places of leisure. Thatcham train station is on the Paddington line and, with a direct service to London, you can reach the capital in under an hour! We also benefit from excellent road links (near to M4 and other major roads) as well as proximity to major international airports. All this comes without the cost of London property. ABOUT THATCHAM Where is Kennet School? Kennet School is situated in the small market town of Thatcham in West Berkshire. Near to Newbury (3 miles), Reading (14.5 miles), and Oxford (29 miles), Thatcham is an ideal base to explore everything the South East of England has to offer. Reading (14 miles) LondonAPPLICANT (55.5 miles) OxfordLETTER (29.4 miles) Windsor Castle (35.7 miles) Highclere Castle (8.3 miles) Newbury Racecourse (2.5 miles) SURROUNDING AREAS The Woodspeen Stonehenge (44.9 miles) Thorpe Park (46.9 miles) (Michelin Star Restaurant) (5.8 miles) So much to do, so much to see… Take the family! Take a stroll along the Kennet and Avon Feed the animals at Bucklebury Farm -

22 Medway Close Thatcham West Berkshire RG18 3AU 22 Medway Close Thatcham West Berkshire RG18 3AU Price Guide: £187,500 Freehold
22 Medway Close Thatcham West Berkshire RG18 3AU 22 Medway Close Thatcham West Berkshire RG18 3AU Price Guide: £187,500 Freehold A modern starter home with garage and garden in a popular cul de sac just north of Thatcham town centre • Living room with spiral staircase • Fitted kitchen • Large double bedroom • Bathroom • Gas central heating • Double glazing • Garage and parking • Enclosed garden • No onward chain • Perfect rental, downsizer or first time buy Location Medway Close is situated on the northern edge of Thatcham close to the Regency Hotel and approximately 1 mile from Thatcham's shopping precinct. Thatcham offers an excellent range of shopping, leisure and educational facilities and has a station on the direct line to London Paddington. Road links are very good with the A4 giving access to the M4 motorway at junction 13 at Chieveley and junction 12 at Theale and Thatcham is surrounded by open countryside. The station is on the direct line to London Paddington. It is highly unusual to find such a property with a garage and a generous garden! Paul Hodgson Description This modern property forms part of a cluster and offers a double aspect living room with a spiral staircase and a fitted kitchen on the ground floor with a generous master bedroom and bathroom on the first floor. The property also offers double glazing and gas central heating and is available with no onward chain. Outside This versatile property comes with its own garage and parking space and also has its own secret garden, hidden away behind the garage and slightly separate to the house. -

West Berkshire Council Adoption Service Inspection Report for LA Adoption Agency
West Berkshire Council Adoption Service Inspection report for LA Adoption Agency Unique reference number SC057256 Inspection date 01/02/2008 Inspector Rosemary Chapman / Margaret Lynes Type of inspection Key Setting address West Berkshire District Council, Social Services, Avonbank House, West Street, NEWBURY, Berkshire, RG14 1BZ Telephone number 01635 519051 Email Registered person West Berkshire Council Registered manager Diane Grist Responsible individual Karen Reeve Date of last inspection 13/12/2004 Inspection Report: West Berkshire Council Adoption Service, 01/02/2008 2 of 10 © Crown copyright 2008 Website: www.ofsted.gov.uk This document may be reproduced in whole or in part for non-commercial educational purposes, provided that the information quoted is reproduced without adaptation and the source and date of publication are stated. You can obtain copies of The Children Act 2004, Every Child Matters and The National Minimum Standards for Children’s Services from: The Stationery Office (TSO) PO Box 29, St Crispins, Duke Street, Norwich, NR3 1GN. Tel: 0870 600 5522. Online ordering: www.tso.co.uk/bookshop Inspection Report: West Berkshire Council Adoption Service, 01/02/2008 3 of 10 About this inspection The purpose of this inspection is to assure children and young people, parents, the public, local authorities and government of the quality and standard of the service provided. The inspection was carried out under the Care Standards Act 2000. This report details the main strengths and any areas for improvement identified during the inspection. The judgements included in the report are made in relation to the outcomes for children set out in the Children Act 2004 and the relevant National Minimum Standards for the service. -

Choosing a Nursery/ School/College
SENDIASS Training for Parents & Carers of children with Special Educational Needs (0-25) Welcome Choosing a nursery/ school/ college for your child with SEN ( Special Educational Needs) Your Trainers: Hannah Pinchin and Hayley Legg HOUSE KEEPING • Microphones on mute please • Feel free to add comments and questions to the chat box and we will email you a summary sheet with the answers on after the talk • PowerPoint will be shared after the training – sit back and relax! SENDIASS (Special Educational Needs and Disability Information Advice and Support Service) Who are we? SEND Information Advice Support A service for those Providing factual Providing impartial Providing living or working information found in advice on what confidential with ages 0-25yrs SEND Law and steps to take in the individualised with Special practices as well as areas of Education, support to empower Educational Needs local knowledge and Health and Social those who seek our and Disabilities signposting Care assistance TYPES OF EDUCATION MAINTAINED INDEPENDENT Educational institutions Educational institutions controlled and funded independent of local (maintained) by local authorities / secretary of authorities state MAINSTREAM SPECIALIST RESOURCE BASE A mainstream school is a A special school is a school Resource bases provide school which is not a which is “specially targeted specialist support special school and is either organised to make special but are not separate a maintained school or an educational provision for schools or institutions. Academy (section 83 CAFA pupils with SEN” (section They are units within a 2014). 337 of the Education Act mainstream school. 1996). How to make a short list List your ideal school (involve the child/YP if possible) 1. -
Style Guide Ensuring a Strong, Recognisable Brand and Identity
Style Guide Ensuring a strong, recognisable brand and identity A shared service provided by Bracknell Forest Council, West Berkshire Council and Wokingham Borough Council Contents Introduction 3 The logo 4 The Partner footer 5 Fonts 6 Colour palette 7 Using our branding 8 How not to use our branding 8 Print design elements 9 Digital design elements 10 Stationery 11 Templates, forms and PPP PowerPoint template 12 Public Protection Partnership - Style Guide 2 Introduction The principal elements of the corporate identity are the: • Logos • Partner footer • Corporate colours and • Corporate fonts This Style Guide details the corporate identity of the PPP and how it should be applied across the service and its associated projects, either in print or digitally. There are no exceptions. This guide is aimed all PPP officers and explains what is allowed and what is not. The Style Guide racnell orest is also for all outside organisations who have been Public Protection authorised to produce information or publicity West ershire material on behalf of the PPP. Partnership Woinha In applying these brand rules, designers, as well as officers and members of the PPP, will be playing a vital role in upholding the consistent, corporate image presented by the PPP, contributing to it being a strong and recognisable brand. When creating stationery, printed or digital materials in the first instance please contact: Lead Officer – Community Engagement Claire Lockwood e-mail: [email protected] Tel: 01635 519507 Public Protection Partnership - Style Guide 3 The logo racnell orest This logo is at the heart of the PPP’s corporate Public Protection West ershire identity and it is the primary PPP logo. -

What Scope for Boosting Bus Use? an Analysis of the Intrinsic Bus Potential of Local Authority Areas in England
What scope for boosting bus use? An analysis of the Intrinsic Bus Potential of local authority areas in England October 2019 Urban Transport Group Wellington House 40-50 Wellington Street Leeds – LS1 2DE 0113 251 7445 [email protected] What scope for boosting bus use? Contents Foreword ...................................................................................................................... 3 Executive Summary ..................................................................................................... 4 1. Introduction ........................................................................................................... 6 2. Bus use data .......................................................................................................... 7 3. Explanatory factors for “good bus territory” ...................................................... 8 4. Defining Intrinsic Bus Potential ......................................................................... 15 5. Understanding the significance of public transport provision ........................ 18 6. Local authorities with higher than expected bus use ....................................... 22 7. Change in bus use over time .............................................................................. 29 8. Case studies ........................................................................................................ 34 9. Discussion and conclusions .............................................................................. 47 October 2019 -
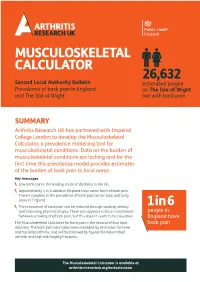
Prevalence of Back Pain in England and Local Authorities
MUSCULOSKELETAL CALCULATOR 26,632 Second Local Authority Bulletin estimated people Prevalence of back pain in England on The Isle of Wight and The Isle of Wight live with back pain SUMMARY Arthritis Research UK has partnered with Imperial College London to develop the Musculoskeletal Calculator, a prevalence modelling tool for musculoskeletal conditions. Data on the burden of musculoskeletal conditions are lacking and for the first time this prevalence model provides estimates of the burden of back pain to local areas. Key messages Low back pain is the leading cause of disability in the UK. Approximately 1 in 6 adults in England have some form of back pain. There’s variation in the prevalence of back pain across local authority areas in England. The prevalence of back pain can be reduced through tackling obesity 1in6 and improving physical activity. There also appears to be an association people in between smoking and back pain, but this doesn’t seem to be causative. England have The Musculoskeletal Calculator for back pain is the second of four local back pain datasets. The back pain estimates were preceded by estimates for knee and hip osteoarthritis, and will be followed by figures for rheumatoid arthritis and high risk fragility fractures. The Musculoskeletal Calculator is available at arthritisresearchuk.org/mskcalculator BACK PAIN IN ENGLAND Prevalence There’s variation in the prevalence of back pain at local authority level in England as estimated by the MSK Calculator. Approximately 1 in 6 people (16.9%) in England have back pain. This includes people of all ages and 9m all causes of back pain.* The prevalence varies across local authorities in estimated people England, ranging from 11.8% to 21.4%. -

Audited Accounts
Charity Registration No. 1096327 Company Registration No. 4530443 (England and Wales) PORTSMOUTH DISABILITY FORUM (PDF) (LIMITED BY GUARANTEE) TRUSTEES' REPORT AND ACCOUNTS FOR THE YEAR ENDED 31 MARCH 2015 PORTSMOUTH DISABILITY FORUM (PDF) (LIMITED BY GUARANTEE) LEGAL AND ADMINISTRATIVE INFORMATION Trustees Sharon Smithson - Chair Alasdair Carnegie - Vice Chair Renata Evans Wendy Roberts Paul Taylor - Honorary Treasurer Christine Rains Stuart Elsom Peter Cairns George Semmens Ivor Grayson Smith Secretary Lynne Rigby Charity number 1096327 Company number 4530443 Principal address Frank Sorrell Centre Prince Albert Road Eastney Portsmouth Hampshire P049HR Registered office Frank Sorrell Centre Prince Albert Road Eastney Portsmouth Hampshire P049HR Auditors Jones Avens Limited Piper House 4 Dukes Court Bognor Road Chichester West Sussex PQ19 8FX Bankers Co-operative Bank pic PO Box 250 Delf House Southway Skelmersdale WN8 6WT PORTSMOUTH DISABILITY FORUM (PDF) (LIMITED BY GUARANTEE) CONTENTS Page Trustees' report 1-6 Statement of trustees' responsibilities 7 Independent auditors' report 8-9 Statement of financial activities 10-11 Balance sheet 12 Notes to the accounts 13-25 PORTSMOUTH DISABILITY FORUM (PDF) (LIMITED BY GUARANTEE) TRUSTEES' REPORT FOR THE YEAR ENDED 31 MARCH 2015 The trustees present their report and accounts for the year ended 31 March 2015. The accounts have been prepared in accordance with the accounting policies set out in note 1 to the accounts and comply with the charity's governing document, the Companies Act 2006 and the Statement of Recommended Practice, "Accounting and Reporting by Charities", issued in March 2005. Structure, governance and management The charity is a company limited by guarantee. The charity's objects are to promote the care, welfare, interest, education and advancement of disabled people their families and personal assistants and their independence and inclusion within the community of Portsmouth and the surrounding areas. -
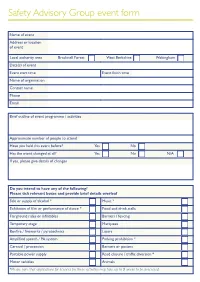
Safety Advisory Group Event Form
Safety Advisory Group event form Name of event Address or location of event Local authority area Bracknell Forest West Berkshire Wokingham Date(s) of event Event start time Event finish time Name of organisation Contact name Phone Email Brief outline of event programme / activities Approximate number of people to attend Have you held this event before? Yes No Has the event changed at all? Yes No N/A If yes, please give details of changes Do you intend to have any of the following? Please tick relevant boxes and provide brief details overleaf Sale or supply of alcohol * Music * Exhibition of film or performance of dance * Food and drink stalls Fairground rides or inflatables Barriers / fencing Temporary stage Marquees Bonfire / fireworks / pyrotechnics Lasers Amplified speech / PA system Parking prohibition * Carnival / procession Banners or posters Portable power supply Road closure / traffic diversion * Motor vehicles Animals *Please note that applications for licences for these activities may take up to 8 weeks to be processed Please provide details reference any activities ticked on page 1: Please provide details of any toilet and sanitary facilities: Please provide details of method to be used to dispose of waste from the event: Please provide details of any car parking provision and how this will be managed: Please give details of any first aid provision: Please give details of any fire safety provision: Please give details of any noise control measures: Please give details of any temporary drinking water supplies to be provided: Please give details of any external contractors and/or concessions: Are you submitting a site/route plan? Site plans should be to scale and show the position of any stalls, stages or structures, toilets, first aid points, access/egress routes for emergency vehicles, car parking etc. -

Useful Contacts
Useful websites West Berkshire Council westberks.gov.uk Citizen’s Advice Bureau West Berkshire cab.org.uk Macmillan Caring, supporting... macmillan.org.uk Sue Ryder sueryder.org Welfare Benefits Out of Hours Doctors direct.gov.uk/benefits Westcall 111 Newbury Breast Care Support Group Useful Contacts nbcsg.net Mobility Aids Marie Curie mariecurie.org.uk ShopMobility 01635 523854 Crossroads Care oxfordshirecrossroads.org.uk Stair Lifts (purchase or hire) 14-21 Time To Talk Acorn Stairlift 0800 326 5199 t2twb.org AST Services Ltd 01753 654879 / 07973 669115 This leaflet is intended as a guide and not as a recommendation. Details are accurate at the time of going to print. July 2018 Stannah Stairlift 0800 715 455 Day Therapy Sue Ryder Day Hospice 01635 273725 (Information & Day Therapy Centre for people with For further information cancer & other life threatening conditions). Director of Operations Newbury Cancer Care We’re here to The Rosemary Centre Transport West Berkshire Community Hospital help you Cabco 01635 333333 Benham Hill (Taxi – also takes wheelchairs) RG18 3AS Newbury Cancer Care 07717 783811 t. 01635 31542 Volunteer Centre West Berks 01635 49004 e. [email protected] newburycancercare.org.uk Blue Badge Parking 01635 42400 Your local cancer charity providing support and Here to help you... information in newburycancercare.org.uk West Berkshire Patron: The Countess of Carnarvon | Charity Registration No. 1157796 x Helping you with the day to day... Advice and Support Home Meal Delivery Patient Information AGE UK