Criminal Behaviour Associated with a Novel Mutation in the VPS13A-Gene Causing Chorea-Acanthocytosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kaplan & Sadock's Study Guide and Self Examination Review In
Kaplan & Sadock’s Study Guide and Self Examination Review in Psychiatry 8th Edition ← ↑ → © 2007 Lippincott Williams & Wilkins Philadelphia 530 Walnut Street, Philadelphia, PA 19106 USA, LWW.com 978-0-7817-8043-8 © 2007 by LIPPINCOTT WILLIAMS & WILKINS, a WOLTERS KLUWER BUSINESS 530 Walnut Street, Philadelphia, PA 19106 USA, LWW.com “Kaplan Sadock Psychiatry” with the pyramid logo is a trademark of Lippincott Williams & Wilkins. All rights reserved. This book is protected by copyright. No part of this book may be reproduced in any form or by any means, including photocopying, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. Printed in the USA Library of Congress Cataloging-in-Publication Data Sadock, Benjamin J., 1933– Kaplan & Sadock’s study guide and self-examination review in psychiatry / Benjamin James Sadock, Virginia Alcott Sadock. —8th ed. p. cm. Includes bibliographical references and index. ISBN 978-0-7817-8043-8 (alk. paper) 1. Psychiatry—Examinations—Study guides. 2. Psychiatry—Examinations, questions, etc. I. Sadock, Virginia A. II. Title. III. Title: Kaplan and Sadock’s study guide and self-examination review in psychiatry. IV. Title: Study guide and self-examination review in psychiatry. RC454.K36 2007 616.890076—dc22 2007010764 Care has been taken to confirm the accuracy of the information presented and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. -
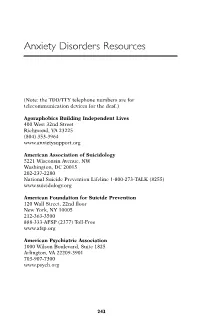
Anxiety Disorders Resources
Anxiety Disorders Resources (Note: the TDD/TTY telephone numbers are for telecommunication devices for the deaf.) Agoraphobics Building Independent Lives 400 West 32nd Street Richmond, VA 23225 (804) 353-3964 www.anxietysupport.org American Association of Suicidology 5221 Wisconsin Avenue, NW Washington, DC 20015 202-237-2280 National Suicide Prevention Lifeline 1-800-273-TALK (8255) www.suicidology.org American Foundation for Suicide Prevention 120 Wall Street, 22nd floor New York, NY 10005 212-363-3500 888-333-AFSP (2377) Toll-Free www.afsp.org American Psychiatric Association 1000 Wilson Boulevard, Suite 1825 Arlington, VA 22209-3901 703-907-7300 www.psych.org 243 244 ANXIETY DISORDERS RESOURCES American Psychological Association 750 First Street, N.E. Washington, DC 20002-4242 800-374-2721 202-336-5500 TDD/TTY: 202-336-6213 www.apa.org Anxiety Disorders Association of America 8730 Georgia Avenue, Suite 600 Silver Spring, MD 20910 240-485-1001 www.adaa.org Association for Behavioral and Cognitive Therapies 305 Seventh Avenue, 16th floor New York, NY 10001 (212) 647-1890 www.aabt.org Doctors Guide www.docguide.com Freedom from Fear 308 Seaview Avenue Staten Island, NY 10305 718-351-1717 www.freedomfromfear.org International Society for Traumatic Stress Studies 60 Revere Drive, Suite 500 Northbrook IL 60062 847-480-9028 www.istss.org MedlinePlus: Health Information www.medlineplus.gov Mental Health America (formerly National Mental Health Association) 2000 N. Beauregard St., 6t floor Alexandria, VA 22311 800-969-6MHA (6642) 703-684-7722 TTY: 800-433-5959 www.mentalhealthamerica.net ANXIETY DISORDERS RESOURCES 245 National Alliance for the Mentally Ill Colonial Place Three 2107 Wilson Boulevard, Suite 300 Arlington, VA 22201-3042 800-950-NAMI (6264) 703-524-7600 TDD: 703-516-7227 www.nami.org National Anxiety Foundation 3135 Custer Drive Lexington, KY 40517-4001 606-272-7166 National Center for Posttraumatic Stress Disorder U.S. -

Psychopathology & Abnormal Psychology
PsychopathologyPsychopathology && AbnormalAbnormal PsychologyPsychology WeWe havehave talkedtalked aboutabout individualindividual differencesdifferences inin personality,personality, abilities,abilities, etc.,etc., butbut somesome individualindividual differencesdifferences gogo beyondbeyond thethe rangerange ofof normalnormal functioningfunctioning andand areare usuallyusually calledcalled psychologicalpsychological disordersdisorders JustJust howhow toto definedefine psychopathologypsychopathology isis thethe subjectsubject ofof somesome disagreementdisagreement Is it simply statistically infrequent behavior? Violation of social norms? Behavior that produces personal distress? Maladaptive or dysfunctional behavior? PsychologicalPsychological disordersdisorders generallygenerally fitfit severalseveral ofof thesethese criteriacriteria ClassificationClassification schemesschemes ThreeThree categoriescategories (up(up untiluntil aboutabout 2525 yrsyrs ago)ago) Organic brain syndromes Neurosis : any disorder characterized by conflict and anxiety that cause distress and impair a person ’s functioning but don ’t render him/her incapable of coping with external reality (e.g., phobias, panic disorder, obsessive -compulsive disorder, etc.) Psychosis : any disorder characterized by severely disordered thought or perception to the point of a break with reality (e.g., schizophrenia, bipolar disorder) Examples ClassificationClassification schemesschemes TheThe currentcurrent emphasisemphasis isis onon clear,clear, observableobservable -
An Access-Dictionary of Internationalist High Tech Latinate English
An Access-Dictionary of Internationalist High Tech Latinate English Excerpted from Word Power, Public Speaking Confidence, and Dictionary-Based Learning, Copyright © 2007 by Robert Oliphant, columnist, Education News Author of The Latin-Old English Glossary in British Museum MS 3376 (Mouton, 1966) and A Piano for Mrs. Cimino (Prentice Hall, 1980) INTRODUCTION Strictly speaking, this is simply a list of technical terms: 30,680 of them presented in an alphabetical sequence of 52 professional subject fields ranging from Aeronautics to Zoology. Practically considered, though, every item on the list can be quickly accessed in the Random House Webster’s Unabridged Dictionary (RHU), updated second edition of 2007, or in its CD – ROM WordGenius® version. So what’s here is actually an in-depth learning tool for mastering the basic vocabularies of what today can fairly be called American-Pronunciation Internationalist High Tech Latinate English. Dictionary authority. This list, by virtue of its dictionary link, has far more authority than a conventional professional-subject glossary, even the one offered online by the University of Maryland Medical Center. American dictionaries, after all, have always assigned their technical terms to professional experts in specific fields, identified those experts in print, and in effect held them responsible for the accuracy and comprehensiveness of each entry. Even more important, the entries themselves offer learners a complete sketch of each target word (headword). Memorization. For professionals, memorization is a basic career requirement. Any physician will tell you how much of it is called for in medical school and how hard it is, thanks to thousands of strange, exotic shapes like <myocardium> that have to be taken apart in the mind and reassembled like pieces of an unpronounceable jigsaw puzzle. -
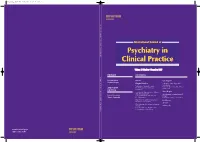
Volume 11 Number 4 December 2007 EDITORS ASSOCIATE EDITORS
Mpcp_11_4_Cover.qxp 11/13/07 12:37 PM Page 1 International Journal of Psychiatry in Clinical Practice 261–344 11 Number 4 December 2007 Pages Volume Volume 11 Number 4 December 2007 EDITORS CONTENTS David Baldwin Editorial Case Report Siegfried Kasper Original Articles Topiramate-induced psychotic exacerbation Evaluation of traumatic events EH Karsliogˇlu, H Karakiliç, E Taner BN Axelrod, J Grabowski and ASSOCIATE and B Cos¸ar EDITORS L Trewhella Screening for depression in a diabetic Short Report outpatient population Questionnaire on animal-assisted Robert Hirschfeld EJ Daly, MH Trivedi, P Raskin and therapy Shigeto Yamawaki BD Grannemann K Iwahashi, C Waga and M Ohta Risperidone in adolescent psychoses Book Review M Hrdlicka and I Dudova Abstracts Pilot of group intervention for bipolar disorder Volume Index D Castle, M Berk, L Berk, S Lauder, J Chamberlain and M Gilbert www.tandf.no/ijpcp ISSN 1365-1501 Mpcp_11_4_Cover.qxp 11/12/07 9:13 PM Page 2 INSTRUCTIONS FOR AUTHORS (www.tandf.no/ijpcp) SCOPE AND POLICY ILLUSTRATIONS International Journal of Psychiatry in Clinical Practice (IJPCP) is a high All illustrations should be uploaded as TIFF or high resolution quality quarterly journal targeted primarily at clinical psychiatrists (min.300 dpi) JPEG format. All illustrations (including line drawings working in hospital environments as well as in private practice. and photographs) should be referred to in the text as ‘Figure 1’, Particular emphasis is placed on the interface between important new ‘Figures 1–4’, using Arabic numbers. Each figure must be cited in the treatments stemming from advanced scientific research and their clinical text. -

Development of a Holistic Wellness Model for Managers in Tertiary Institutions
DEVELOPMENT OF A HOLISTIC WELLNESS MODEL FOR MANAGERS IN TERTIARY INSTITUTIONS By PETRUS ALBERTUS BOTHA Submitted in partial fulfilment of the requirements for the degree PHILOSOPHIAE DOCTOR With specialisation in Organisational Behaviour in the THE FACULTY OF ECONOMIC AND MANAGEMENT SCIENCES At the UNIVERSITY OF PRETORIA PRETORIA SEPTEMBER 2007 ii DECLARATION I hereby declare that the “DEVELOPMENT OF A HOLISTIC WELLNESS MODEL FOR MANAGERS IN TERTIARY INSTITUTIONS” is my own work and that all the sources that I used or quoted were indicated with complete references and acknowledgements. ________________ SIGNATURE PETRUS ALBERTUS BOTHA iii SUMMARY DEVELOPMENT OF A HOLISTIC WELLNESS MODEL FOR MANAGERS IN TERTIARY INSTITUTIONS By PETRUS ALBERTUS BOTHA PROMOTER: PROF HEIN BRAND DEGREE: PHILOSOPHIAE DOCTOR (Organisational Behaviour) Research into wellness literature identified the existence of various wellness models consisting of multiple dimensions, and found different relationships between these dimensions. In an attempt to expand on the theory of wellness, this study determined the wellness behaviour and health risk profile of managers at two South African higher education institutions. A sample of 89 managers from two South African universities, a traditional academic university and a technology university, was used in the study. The sample comprised 40.45% respondents from the academic university and 59.55% from the technology university. Females accounted for 31.5% of the sample, while males accounted for 68.5%. The Pearson product moment correlation coefficient was used to determine the relationship between the wellness behaviour levels and the health risk scores of managers. The results suggested that there were no significant correlations between the mean physical fitness and nutrition, medical self-care, safety, environmental wellness, social awareness, intellectual wellness, spirituality and values sub- dimensions and the health risk scores of managers. -
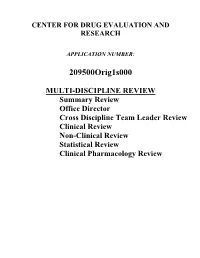
Multi-Discipline Review
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209500Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA 209500 Multi-disciplinary Review and Evaluation Caplyta (lumateperone) NDA/BLA Multi-Disciplinary Review and Evaluation Application Type NDA Application Number(s) 209500 Priority or Standard Standard Submit Date(s) September 27, 2018 Received Date(s) September 27, 2018 PDUFA Goal Date December 27, 2019 Division/Office Division of Psychiatry / Office of Drug Evaluation-I Review Completion Date December 20, 2019 Established/Proper Name Lumateperone (Proposed) Trade Name Caplyta Pharmacologic Class Atypical Antipsychotic Code name ITI-007 Applicant Intra-Cellular Therapies, Inc. Dosage form 42 mg Capsules Applicant proposed Dosing 42 mg by mouth once daily Regimen Applicant Proposed Schizophrenia/Adults Indication(s)/Population(s) Applicant Proposed 58214004 | Schizophrenia (disorder) SNOMED CT Indication Disease Term for each Proposed Indication Recommendation on Approval Regulatory Action Recommended Schizophrenia/Adults Indication(s)/Population(s) (if applicable) Recommended SNOMED 58214004 | Schizophrenia (disorder) CT Indication Disease Term for each Indication (if applicable) Recommended Dosing 42 mg by mouth once daily Regimen 1 Version date: October 12, 2018 Reference ID: 4537404 NDA 209500 Multi-disciplinary Review and Evaluation Caplyta (lumateperone) Table of Contents Table of -

Chapter8 Anxiety Disorders
Abnormal and Clinical Psychology THIRD EDITION University of Dundee 97800335237463_A01.indd i 2/9/11 3:05:53 PM University of Dundee 97800335237463_A01.indd ii 2/9/11 3:05:54 PM Abnormal and Clinical Psychology AN INTRODUCTORY TEXTBOOK THIRD EDITION University of Dundee Paul Bennett Open University Press Open University Press 97800335237463_A01.indd iii 2/9/11 3:05:54 PM Open University Press McGraw-Hill Education McGraw-Hill House Shoppenhangers Road Maidenhead Berkshire England SL6 2QL email: [email protected] world wide web: www.openup.co.uk and Two Penn Plaza, New York, NY 10121-2289, USA First published 2011 Copyright © Bennett 2011 All rights reserved. Except for the quotation of short passages for the purposes of criticism and review, no part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permission of the publisher or a licence from the Copyright Licensing Agency Limited. Details of such licences (for reprographic reproduction) may be obtained from the Copyright Licensing Agency Ltd of Saffron House, 6-10 Kirby Street, London, EC1N 8TS. A catalogue record of this book is available from the British Library ISBN-13: 978-0-33-523746-3 ISBN-10: 0-33-523746-0 Library of Congress Cataloging-in-Publication Data CIP data applied for Typeset by Graphicraft Limited, Hong Kong Printed in Italy by Rotolito Lombarda, Italy Fictitious names of companies, products, people, University characters and/or of Dundee data that may be used herein (in case studies or in examples) are not intended to represent any real individual, company, product or event. -
Compulsive Disorder
A thesis submitted in fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY, Discipline of Psychiatry, The University of Sydney. 7th April 2012. SYMPTOM-BASED SUBTYPES OF OBSESSIVE- COMPULSIVE DISORDER. Student: Dr Vlasios Brakoulias MB,BS (Hon), M(Psychiatry), FRANZCP Clinical lecturer and Staff Specialist in Psychiatry Department of Psychiatry Nepean Clinical School Level 5 South Block Nepean Hospital PO Box 63 Penrith NSW 2751 e-mail: [email protected] Tel: 61 2 4734 2585 Fax: 61 2 4734 3343 Research Supervisor: A/Professor Vladan Starcevic Associate Professor and Department Head Department of Psychiatry Nepean Clinical School Nepean Hospital Associate Research Supervisor: Professor Philip Boyce Professor and Department Head Department of Psychiatry Western Clinical School Westmead Hospital Institutions: Sydney West Area Health Service Department of Psychiatry University of Sydney Nepean Clinical School Nepean Anxiety Disorders Unit Date of Commencement: 5th March, 2007 on Part-time basis. Statement of Originality This thesis is submitted to The University of Sydney in fulfillment of the requirements for the Degree of Doctor of Philosophy. The work presented in this thesis is, to the best of my knowledge and belief, original. I hereby declare that I have not submitted this material either in full or in part, for a degree at this or any other institution. _____________________ ____________________ Vlasios Brakoulias Date 2 3 ABSTRACT Obsessive-compulsive disorder (OCD) is heterogeneous in its presentation and quests to clarify the best way to subtype OCD have remained elusive. This thesis aims to assess for symptom-based OCD subtypes in a sample of patients with OCD and to describe the characteristics of these OCD symptom subtypes. -

Anxiety and Phobias
A Special Health Report from Harvard Medical School Coping with ANXIETY AND PHOBIAS In this report • Recognizing and treating common anxiety disorders • The most effective medications and therapies • Managing panic attacks • Advice for worriers Harvard • Anxiety and sleep: Tips for Medical overcoming insomnia School Price: $24.00 Coping with Anxiety and Phobias A Special Health Report Harvard Medical School Publications Faculty Medical Advisor Special Health Reports Michael Mufson, M.D. Harvard Medical School publishes Special Assistant Professor of Psychiatry Health Reports on a wide range of topics. To Harvard Medical School order other reports or additional copies of this report, please see the order form at the back of this report. Editor Ann Marie Dadoly To obtain multiple-copy discount rates, please write or call: Writer Consumer Health Publishing Group Susan Gilbert Attn: SR Bulk Orders 1100 Summer St., 2nd Floor Editor, Special Health Reports Stamford, CT 06905 Kathleen Cahill Allison (203) 975-8854, ext. 110 Newsletters Illustrator Harvard Medical School publishes the Scott Leighton following monthly newsletters: Harvard Health Letter Copy Editor Harvard Heart Letter James Clyde Sellman Harvard Men’s Health Watch Harvard Women’s Health Watch Production Coordinator Harvard Mental Health Letter Amy E. Yeager Books Published by Harvard Medical School Books published by Harvard Medical School Anthony L. Komaroff, M.D., Editor in Chief include: The Arthritis Action Program: An Integrated Plan of Traditional and Complementary Therapies (Simon and Schuster, 2000) Eat, Drink, and Be Healthy: The Harvard Medical School Guide to Healthy Eating (Simon and Schuster, 2001) Harvard Medical School Family Health Guide (Simon and Schuster, 1999) Healthy Women, Healthy Lives: A Guide to Copyright © 2002 by the President and Fellows of Preventing Disease from the Landmark Nurses’ Harvard College. -

Anxiety Disorders
Anxiety Disorders Program Support Notes by: Reproducing these support notes Jo Basnett B.Ed You may download and print one copy of these support notes from our website for your Executive Producer: reference. Further copying or printing must be Simon Garner B.Ed, Dip reported to CAL as per the Copyright Act Management 1968 . © Video Education Australasia Pty Ltd 2011 Video Education America - Phone 1-866-727-080 - Preview programs online www.VEAvideo.com Anxiety Disorders For Teachers Introduction An anxiety disorder is generally present when a person’s emotional reaction is out of proportion to the level of worry or the anticipated threat, and this anxiety causes a general problem with everyday functioning. There are six different types of anxiety disorders and people can have more than one anxiety disorder at any one time. Anxiety disorders are one of the most common mental health disorders, affecting an increasing amount of adults and teenagers each year. This program will examine the causes, symptoms, and treatments for each of the six types. Expert interviewees and sufferers share their experiences and expertise in this informative program. Timeline 00:00:00 What is an anxiety disorder? 00:04:42 Generalized anxiety disorders and panic disorders 00:09:11 Post traumatic stress disorder 00:12:23 Obsessive compulsive disorder and phobias 00:15:58 Young people and anxiety 00:20:50 Credits 00:21:49 end program Related Titles Dark Days – Shedding Light on Depression Global Health and Human Development Adult Health and Development Health Risks to the World’s Young Recommended Resources http://www.freedomfromfear.org http://au.reachout.com/find/articles/anxiety http://www.anxietyonline.org.au/ http://youth.wyndham.vic.gov.au/gui/files/Orygen%20-%20Anxiety%20%26%20Young%20People.pdf 2 © Video Education Australasia Pty Ltd 2011 Reproducing these support notes You may download and print one copy of these support notes from our website for your reference. -
Thuët Ng÷ Sinh Häc Anh - Viöt
MAI §×NH Y£N, Vò V¡N Vô, L£ §×NH L¦¥NG ThuËt ng÷ sinh häc Anh - viÖt Hµ néi - 2006 A A. flavus A. flavus AA - viÕt t¾t cña Arachidonic Acid aAI-1 aAI-1 ab initio gene prediction abambulacral thiÕu ch©n mót, thiÕu ch©n èng ABC viÕt t¾t cña Association of Biotechnology Companies ABC Transport Proteins protein vËn chuyÓn ABC ABC Transporters nh©n tè vËn chuyÓn ABC abdomen bông, phÇn bông abdominal limbs (c¸c) phÇn phô bông abdominal muscle c¬ bông abdominal pores (c¸c) lç bông abdominal reflex ph¶n x¹ bông abductor c¬ gi¹ng, c¬ duçi abiogenesis (sù) ph¸t sinh phi sinh häc abiotic (thuéc) phi sinh häc, kh«ng sèng abiotic stresses c¨ng th¼ng phi sinh häc ABO blood group substances (c¸c) chÊt nhãm m¸u ABO ABO blood group system hÖ thèng nhãm m¸u ABO abomasum d¹ mói khÕ aboral xa miÖng, ®èi miÖng abortifacient chÊt ph¸ thai abortion 1. (sù) sÈy thai, truþ thai 2. thui chét abrin abrin abscess (sù) ¸p xe abscisic acid axit abscisic abscission (sù) rông absolute configuration cÊu h×nh tuyÖt ®èi absolute refractory period thêi kú bÊt øng tuyÖt ®èi absolute threshold ng−ìng tuyÖt ®èi absorbance chÊt hÊp thô absorbed dose liÒu l−ìng hÊp thô absorption (sù) hÊp thu absorption spectrum phæ hÊp thô abundance ®é phong phó abyssal (thuéc) ®¸y biÓn s©u th¼m abyssal zone vïng n−íc s©u abyssopelagic (thuéc) vïng s©u ®¹i d−¬ng 2 abzymes abzym Ac- CoA Ac- CoA Acanthocephala ngµnh Giun ®Çu mãc acanthozooid thÓ gai Acarina bé Ve bÐt acarophily thÝch ve rÖp acarophitisrn quan hÖ céng sinh ve-rÖp acaulescent (cã) th©n ng¾n acauline kh«ng th©n acaulose kh«ng th©n acceptor junction site ®iÓm liªn kÕt accept¬ accession thªm vµo, bæ sung accessorius 1.