Miltefosine Administration in Cats with Refractory Sporotrichosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Potassium Iodide (KI): Instructions for Children
Potassium Iodide (KI): Instructions for Children The thyroid gland in children is very sensitive to the effects of radioactive iodine. In the event of a nuclear emergency, it is important for adults to understand how to prepare the proper dosage of potassium iodide (KI) for young children. The following information will help you to give KI to your children properly. Children over 12 years to 18 years 2 tablets (whole or crushed) (130 mg) (who weigh at least 150 pounds) Children over 12 years to 18 years 1 tablet (whole or crushed) or 8 teaspoons (65 mg) (who weigh less than 150 pounds) Children over 3 years to 12 years 1 tablet (whole or crushed) or 8 teaspoons (65 mg) Children over 1 month to 3 years 4 teaspoons (32.5 mg) Babies at birth to 1 month 2 teaspoons (16.25 mg) Tablets can be crushed and mixed in many liquids. To take the tablet in liquid solution, use dosing directions under “Making a Potassium Iodide Liquid Mixture.” Take KI only as directed by public officials. Do not take more than 1 dose in 24 hours. More will not help you. Too much medicine may increase the chances of side effects. Making a Potassium Iodide Liquid Mixture 1. Put one 65 mg KI tablet into a small bowl and grind it into a fine powder using the back of a metal teaspoon against the inside of the bowl. The powder should not have any large pieces. 2. Add 4 teaspoons of water to the crushed KI powder in the bowl and mix until the KI powder is dissolved in the water. -

Determination of Iodate in Iodised Salt by Redox Titration
College of Science Determination of Iodate in Iodised Salt by Redox Titration Safety • 0.6 M potassium iodide solution (10 g solid KI made up to 100 mL with distilled water) • 0.5% starch indicator solution Lab coats, safety glasses and enclosed footwear must (see below for preparation) be worn at all times in the laboratory. • 250 mL volumetric flask Introduction • 50 mL pipette (or 20 and 10 mL pipettes) • 250 mL conical flasks New Zealand soil is low in iodine and hence New Zealand food is low in iodine. Until iodised salt was • 10 mL measuring cylinder commonly used (starting in 1924), a large proportion • burette and stand of school children were reported as being affected • distilled water by iodine deficiency – as high as 60% in Canterbury schools, and averaging 20 − 40% overall. In the worst cases this deficiency can lead to disorders such as Method goitre, and impaired physical and mental development. 1. Preparation of 0.002 mol L−1 sodium thiosulfate In earlier times salt was “iodised” by the addition of solution: Accurately weigh about 2.5 g of solid potassium iodide; however, nowadays iodine is more sodium thiosulfate (NaS2O3•5H2O) and dissolve in commonly added in the form of potassium iodate 100 mL of distilled water in a volumetric flask. (This gives a 0.1 mol L−1 solution). Then use a pipette to (KIO3). The Australia New Zealand Food Standards Code specifies that iodised salt must contain: “equivalent to transfer 10 mL of this solution to a 500 mL volumetric no less than 25 mg/kg of iodine; and no more than 65 flask and dilute by adding distilled water up to the mg/kg of iodine”. -

Potassium Iodide (KI) Preparation and Dosing Instructions for Use During a Nuclear Emergency to Make KI Solution (Liquid Form), Using Two 65 Mg KI Tablets
Potassium Iodide (KI) Preparation and Dosing Instructions for Use During a Nuclear Emergency To Make KI Solution (Liquid Form), using two 65 mg KI Tablets If government authorities declare that a radiation emergency has occurred, you may have been exposed to radioactive iodine. Potassium iodide can prevent thyroid cancer in people who have been exposed to radioactive iodine. Potassium iodide is also known as KI. Children who have been exposed to radioactive iodine have a greater risk of thyroid cancer than adults do. You may need to make a KI solution (liquid form) for anyone who cannot swallow tablets. This sheet explains how to make and give the KI solution. FDA-approved KI tablets come in 65 mg and 130 mg strengths. Instructions for preparing the KI solution using two 65 mg tablets are given below. To Make the Potassium Iodide (KI) Solution You Will Need: Two 65 mg KI tablets Teaspoon Small bowl Four teaspoons of water Four teaspoons of a drink. We recommend any one of the following: ■ White milk ■ Chocolate milk ■ Orange juice ■ Soda (For example, cola) ■ Infant formula ■ Raspberry syrup ■ Water Directions for Making the Potassium Iodide (KI) Solution: Step 1. Soften the KI tablets: Put two 65 mg KI tablets into a small bowl. Add four teaspoons of water. Soak the tablets for one minute. Step 2. Crush the softened KI tablets: Use the back of the teaspoon to crush the tablets in the water. At the end of this step, there should not be any large pieces of KI. This makes the KI and water mixture. -

Calcium Chloride
Iodine Livestock 1 2 Identification of Petitioned Substance 3 4 Chemical Names: 7553-56-2 (Iodine) 5 Iodine 11096-42-7 (Nonylphenoxypolyethoxyethanol– 6 iodine complex) 7 Other Name: 8 Iodophor Other Codes: 9 231-442-4 (EINECS, Iodine) 10 Trade Names: CAS Numbers: 11 FS-102 Sanitizer & Udderwash 12 Udder-San Sanitizer and Udderwash 13 14 Summary of Petitioned Use 15 The National Organic Program (NOP) final rule currently allows the use of iodine in organic livestock 16 production under 7 CFR §205.603(a)(14) as a disinfectant, sanitizer and medical treatment, as well as 7 CFR 17 §205.603(b)(3) for use as a topical treatment (i.e., teat cleanser for milk producing animals). In this report, 18 updated and targeted technical information is compiled to augment the 1994 Technical Advisory Panel 19 (TAP) Report on iodine in support of the National Organic Standard’s Board’s sunset review of iodine teat 20 dips in organic livestock production. 21 Characterization of Petitioned Substance 22 23 Composition of the Substance: 24 A variety of substances containing iodine are used for antisepsis and disinfection. The observed activity of 25 these commercial disinfectants is based on the antimicrobial properties of molecular iodine (I2), which 26 consists of two covalently bonded atoms of elemental iodine (I). For industrial uses, I2 is commonly mixed 27 with surface-active agents (surfactants) to enhance the water solubility of I2 and also to sequester the 28 available I2 for extended release in disinfectant products. Generally referred to as iodophors, these 29 “complexes” consist of up to 20% I2 by weight in loose combination with nonionic surfactants such as 30 nonylphenol polyethylene glycol ether (Lauterbach & Uber, 2011). -

World Health Organization Model List of Essential Medicines, 21St List, 2019
World Health Organizatio n Model List of Essential Medicines 21st List 2019 World Health Organizatio n Model List of Essential Medicines 21st List 2019 WHO/MVP/EMP/IAU/2019.06 © World Health Organization 2019 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. World Health Organization Model List of Essential Medicines, 21st List, 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. -

Queensland Health List of Approved Medicines
Queensland Health List of Approved Medicines Drug Form Strength Restriction abacavir * For use in accord with PBS Section 100 indications * oral liquid See above 20 mg/mL See above tablet See above 300 mg See above abacavir + lamivudine * For use in accord with PBS Section 100 indications * tablet See above 600 mg + 300 mg See above abacavir + lamivudine + * For use in accord with PBS Section 100 indications * zidovudine tablet See above 300 mg + 150 mg + 300 mg See above abatacept injection 250 mg * For use in accord with PBS Section 100 indications * abciximab (a) Interventional Cardiologists for complex angioplasty (b) Interventional and Neuro-interventional Radiologists for rescue treatment of thromboembolic events that occur during neuroendovascular procedures. * Where a medicine is not TGA approved, patients should be made fully aware of the status of the medicine and appropriate consent obtained * injection See above 10 mg/5 mL See above abiraterone For use by medical oncologists as per the PBS indications for outpatient and discharge use only tablet See above 250 mg See above 500 mg See above acamprosate Drug and alcohol treatment physicians for use with a comprehensive treatment program for alcohol dependence with the goal of maintaining abstinence. enteric tablet See above 333 mg See above acarbose For non-insulin dependent diabetics with inadequate control despite diet; exercise and maximal tolerated doses of other anti-diabetic agents tablet See above 50 mg See above 100 mg See above acetazolamide injection 500 mg tablet 250 mg acetic acid ear drops 3% 15mL solution 2% 100mL green 3% 1 litre 6% 1 Litre 6% 200mL Generated on: 30-Aug-2021 Page 1 of 142 Drug Form Strength Restriction acetylcysteine injection For management of paracetamol overdose 2 g/10 mL See above 6 g/30 mL See above aciclovir cream Infectious disease physicians, haematologists and oncologists 5% See above eye ointment For use on the advice of Ophthalmologists only. -
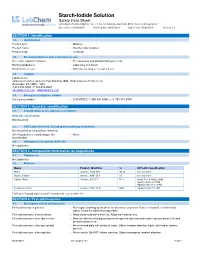
Starch-Iodide Solution Safety Data Sheet According to Federal Register / Vol
Starch-Iodide Solution Safety Data Sheet according to Federal Register / Vol. 77, No. 58 / Monday, March 26, 2012 / Rules and Regulations Date of issue: 05/08/2015 Revision date: 04/25/2018 Supersedes: 05/08/2015 Version: 1.1 SECTION 1: Identification 1.1. Identification Product form : Mixtures Product name : Starch-Iodide Solution Product code : LC25330 1.2. Recommended use and restrictions on use Use of the substance/mixture : For laboratory and manufacturing use only. Recommended use : Laboratory chemicals Restrictions on use : Not for food, drug or household use 1.3. Supplier LabChem Inc Jackson's Pointe Commerce Park Building 1000, 1010 Jackson's Pointe Court Zelienople, PA 16063 - USA T 412-826-5230 - F 724-473-0647 [email protected] - www.labchem.com 1.4. Emergency telephone number Emergency number : CHEMTREC: 1-800-424-9300 or +1-703-741-5970 SECTION 2: Hazard(s) identification 2.1. Classification of the substance or mixture GHS-US classification Not classified 2.2. GHS Label elements, including precautionary statements Not classified as a hazardous chemical. Other hazards not contributing to the : None. classification 2.4. Unknown acute toxicity (GHS US) Not applicable SECTION 3: Composition/Information on ingredients 3.1. Substances Not applicable 3.2. Mixtures Name Product identifier % GHS -US classification Water (CAS-No.) 7732-18-5 99.32 Not classified Starch, Soluble (CAS-No.) 9005-25-8 0.5 Not classified Salicylic Acid (CAS-No.) 69-72-7 0.13 Acute Tox. 4 (Oral), H302 Aquatic Acute 3, H402 Aquatic Chronic 3, H412 Potassium Iodide (CAS-No.) 7681-11-0 0.05 Aquatic Acute 2, H401 Full text of hazard classes and H-statements : see section 16 SECTION 4: First-aid measures 4.1. -

Potassium Iodide (KI) Use During a Radiological Emergency
Potassium Iodide (KI) Use during a Radiological Emergency What is potassium iodide? Potassium iodide (KI) is a salt available as an over-the-counter medicine to help protect the thyroid gland if a person is exposed to radioactive iodine. It can be used as a supplement to evacuation and sheltering in the event radioactive iodine is released in a nuclear power plant accident. During a radiological emergency, potassium iodide should only be taken when directed the State Health Commissioner or designee. What is the role of potassium iodide in a nuclear power plant accident? Potassium iodide, if taken in an appropriate dosage and in a timely manner, can block uptake of radioactive iodine by the thyroid gland and reduce the risk of thyroid cancer. Radioactive iodine is one of the major contaminants that could be released in a nuclear power plant accident. Exposure to radioactive iodine through ingestion or inhalation can increase the risk of developing thyroid cancer in humans, especially in children, who are more likely to develop thyroid cancer following exposure to radioactive iodine. What is the thyroid? The thyroid is a gland located in the neck, below the Adam’s apple. It makes and stores hormones that help regulate heart rate, blood pressure, body temperature, and metabolism (the rate at which food is converted to energy). Thyroid hormones also help children grow and develop. The thyroid uses iodine to make its hormones. How does potassium iodide protect against thyroid cancer? The thyroid gland requires certain levels and forms of iodine to function properly and can store certain amounts. -

Comparative Evaluation of the Efficacy and Safety of Two Doses Of
Original article Comparative evaluation of the efficacy and safety of two doses of terbinafine (500 and 1000 mg day)1) in the treatment of cutaneous or lymphocutaneous sporotrichosis Vergleichende Bewertung der Wirksamkeit und Sicherheit zweier Terbinafin-Dosierungen (500 und 1000 mg/Tag) in der Therapie der kutanen und lymphokutanen Sporotrichose S. W. Chapman,1 P. Pappas,2 C. Kauffmann,3 E. B. Smith,4 R. Dietze,5 N. Tiraboschi-Foss,6 A. Restrepo,7 A. B. Bustamante,8 C. Opper,2,9 S. Emady-Azar10 and R. Bakshi10 1University of Mississippi Medical Center, Jackson, MS, USA, 2University of Alabama, Birmingham, AL, USA, 3University of Michigan Medical School and Veteran Affairs Medical Centre, Ann Arbour, MI, USA, 4University of New Mexico, Albuquerque, NM, USA, 5Nu´cleo de Doenc¸as Infecciosas, Universidade Ferderal do Espirito Santo, Vitoria, Brazil, 6University of Sa˜o Paulo, Ribeira˜o Preto, Sa˜o Paulo, Brazil, 7National University of Columbia, Medellin, Columbia, 8Instituto de Medicina Tropical ‘Alexander von Humboldt’, Universidad Peruana Cayetano Heredia, Lima, Peru, 9Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA and 10Novartis Pharma AG, Basel, Switzerland Summary The aim of this study was to evaluate the safety and efficacy of oral terbinafine (500 and 1000 mg day)1) in the treatment of cutaneous or lymphocutaneous sporotrichosis. A culture for Sporothrix schenckii was required for inclusion into this multicentre, randomized, double-blind, parallel-group study. Patients received either 250 mg b.i.d. or 500 mg b.i.d. oral terbinafine for up to a maximum of 24 weeks and were assessed up to 24 weeks post-treatment. -

Complete List of Chemicals These Chemicals Are Stored in an Adjacent Area
Possible Hazards for FSCI - 210 Finger Print Dust (pulverized volcanic rock) Cyanoacrylate (super glue) Dried blood smears (human and canine) Hydrogen peroxide drops Ethyl alcohol drops Phenolphthalein drops Complete List of Chemicals These chemicals are stored in an adjacent area. Any could be used for another course in the same lab room as FSCI - 210 but at a different time. Exposure is possible but not probable. Acetanilide Ammonium Dichromate Acetic Acid, Glacial Ammonium Hydroxide Acetic Acid, 0.01M, 0.1M, 1M Ammonium Nitrate Acetic Anhydride Ammonium Nitrate, 0.1M Acetone Ammonium Oxalate Acrylic Acid Monohydrate Adhesive Side Powder, Dark Ammonium Persulfate Albumin, Egg Amyl Alcohol Alka-Seltzer Argon Spectrum Tubes All-Purpose Cleaner Arsenic Trioxide Aluminum (Foil) Ascorbic Acid (Vitamin C) Aluminum (Wire) Aspirin (Acetylsalicylic Acid) Aluminum Nitrate – 9-hydrate Barium Chloride-anhydrous Aminobenzoic Acid, 3- Barium Chloride-2-hydrate Ammonia (household) Barium Hydroxide – Anhydrous Ammonia Tablets #1, #2 Barium Hydroxide – 8-hydrate Ammonium Acetate Barium Nitrate Ammonium Acetate, 0.1M Basic Yellow Ammonium Bicarbonate Benzil Ammonium Chloride Benzoic Acid Benzophenone Copper(II) Nitrate–2½-hydrate Bleach Copper(II) Sulfate–Anhydrous Bogen Universal Indicator Copper(II) Sulfate–5-hydrate Boiling Chips, pumice Cyanoacrylate Cyclohexane Boric Acid Cyclohexanol Boric Acid, 0.1M Cyclohexanone Brass Cyclohexene Bromcresol Green Indicator Deet (N,N-diethyl-m-toluamide) Bromoethane (Ethyl Bromide) Dessicant Bromothymol Blue Dichlorobenzene-p -

8. Regulations and Advisories
IODINE 309 8. REGULATIONS AND ADVISORIES The international, national, and state regulations and guidelines regarding stable iodine in air, water, and other media are summarized in Table 8-1. The regulations regarding radioactive iodine are summarized in Tables 8-2 and 8-3. No MRLs were derived for inhalation exposure to stable or radioactive iodine. Oral MRLs of 0.01 mg/kg/day were derived for both acute- and chronic-duration exposures. No oral MRL was derived for intermediate-duration exposure. The EPA has not classified iodine for human carcinogenicity, nor has the EPA derived reference concentrations (RfCs) or reference doses (RfDs) for stable or radioactive iodine (IRIS 2000). IODINE 310 8. REGULATIONS AND ADVISORIES Table 8-1. Regulations and Guidelines Applicable to Stable Iodine Agency Description Information References INTERNATIONAL Guidelines: IARC Carcinogenicity classification No data NATIONAL Regulations and Guidelines: a. Air ACGIH STEL (ceiling) 0.1 ppm ACGIH 2000 NIOSH REL (ceiling) 0.1 ppm NIOSH 2001 IDLH 2.0 ppm OSHA PEL (ceiling)—general industry 0.1 ppm OSHA 2001b 29CFR1910.1000 PEL (ceiling)—construction industry 0.1 ppm OSHA 2001a 29CFR1926.55 PEL (ceiling)—shipyard industry 0.1 ppm OSHA 2001c 29CFR1915.1000 b. Water EPA Effluent limitation guidelines; Effluent reduction EPA 2001b inorganic chemicals manufacturing attainable by the 40CFR415.432 point source category for iodine application of BPT; no production discharge of process wastewater pollutants to navigable waters c. Food FDA Drug products containing certain -

A Prospective Case Series Evaluating Efficacy and Safety of Combination of Itraconazole and Potassium Iodide in Rhinofacial Coni
Tropical medicine rounds Aprospectivecaseseriesevaluatingefficacyandsafetyof combination of itraconazole and potassium iodide in rhinofacial conidiobolomycosis Manish Gupta1, MS, Tarun Narang2, MD, Rupinder Jeet Kaur3, MD, Ashwani Manhas4, MD, Uma Nahar Saikia5, MD, and Sunil Dogra2, MD, MANAMS, FRCP 1Department of ENT, Gian Sagar Medical Abstract College & Hospital, Banur District, Patiala, Background Rhinofacial conidiobolomycosis (RFC) is an uncommon subcutaneous fungal 2 Punjab, Department of Dermatology, infection producing painless swelling with grotesque deformity of the face. Although there Venereology and Leprology, Post Graduate are case reports and small case series; there are very few prospective studies evaluating Institute of Medical Education & Research, Chandigarh, 3Department of Pathology, treatment outcome and long-term follow-up. Gian Sagar Medical College & Hospital, Objective To evaluate the safety and efficacy of combination of itraconazole (200 mg Banur District, Patiala, Punjab, twice daily) and saturated solution of potassium iodide (SSKI) in patients with RFC. 4 Department of Microbiology, Gian Sagar Methods Ten patients of RFC were studied over a period of 5 years. Diagnosis was Medical College & Hospital, Banur District, confirmed by clinical, histopathological, and microbiological evaluation. Conidiobolus was Patiala, Punjab, and 5Department of Histopathology, Post Graduate Institute of cultured in four cases and in the rest of the cases, the histopathology was suggestive of Medical Education & Research, RFC.