Quantitative Analysis of Iris Parameters in Keratoconus Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Microscopic Anatomy of the Eye Dog Cat Horse Rabbit Monkey Richard R Dubielzig Mammalian Globes Mammalian Phylogeny General Anatomy Dog
Microscopic Anatomy of the eye Dog Cat Horse Rabbit Monkey Richard R Dubielzig Mammalian globes Mammalian Phylogeny General Anatomy Dog Arterial Blood Vessels of the Orbit General Anatomy Dog * Horizontal section Long Posterior Ciliary a. Blood enters the globe Short Post. Ciliary a Long Post. Ciliary a. Anterior Ciliary a. Blood Supply General Anatomy Dog Major arterial circle of the iris Orbital Anatomy Dog Brain Levator Dorsal rectus Ventral rectus Zygomatic Lymph node Orbital Anatomy Dog Orbital Anatomy Dog Cartilaginous trochlea and the tendon of the dorsal oblique m. Orbital Anatomy Dog Rabbit Orbital Anatomy Dog Zygomatic salivary gland mucinous gland Orbital Anatomy Dog Gland of the Third Eyelid Eye lids (dog) Eye lids (dog) Meibomian glands at the lid margin Holocrine secretion Eye lids (primate) Upper tarsal plate Lower tarsal plate Eye lids (rabbit) The Globe The Globe Dog Cat Orangutan Diurnal Horse Diurnal Cornea Epithelium Stromal lamellae Bowman’s layer Dolphin Descemet’s m Endothelium TEM of surface epithelium Cornea Doubling of Descemet’s Vimentin + endothelium Iris Walls: The vertebrate eye Iris Sphincter m. Dilator m Blue-eye, GFAP stain Iris Collagen Iris Cat Sphinctor m. Dilator m. Iris Cat Phyomelanocytes Iris Equine Corpora nigra (Granula iridica) seen in ungulates living without shade Ciliary body Pars plicata Ciliary muscle Pars plana Ciliary body Zonular ligaments Ciliary body Primarily made of fibrillin A major component of elastin Ciliary body Alcian Blue staining acid mucopolysaccharides: Hyaluronic acid Ciliary -

The Complexity and Origins of the Human Eye: a Brief Study on the Anatomy, Physiology, and Origin of the Eye
Running Head: THE COMPLEX HUMAN EYE 1 The Complexity and Origins of the Human Eye: A Brief Study on the Anatomy, Physiology, and Origin of the Eye Evan Sebastian A Senior Thesis submitted in partial fulfillment of the requirements for graduation in the Honors Program Liberty University Spring 2010 THE COMPLEX HUMAN EYE 2 Acceptance of Senior Honors Thesis This Senior Honors Thesis is accepted in partial fulfillment of the requirements for graduation from the Honors Program of Liberty University. ______________________________ David A. Titcomb, PT, DPT Thesis Chair ______________________________ David DeWitt, Ph.D. Committee Member ______________________________ Garth McGibbon, M.S. Committee Member ______________________________ Marilyn Gadomski, Ph.D. Assistant Honors Director ______________________________ Date THE COMPLEX HUMAN EYE 3 Abstract The human eye has been the cause of much controversy in regards to its complexity and how the human eye came to be. Through following and discussing the anatomical and physiological functions of the eye, a better understanding of the argument of origins can be seen. The anatomy of the human eye and its many functions are clearly seen, through its complexity. When observing the intricacy of vision and all of the different aspects and connections, it does seem that the human eye is a miracle, no matter its origins. Major biological functions and processes occurring in the retina show the intensity of the eye’s intricacy. After viewing the eye and reviewing its anatomical and physiological domain, arguments regarding its origins are more clearly seen and understood. Evolutionary theory, in terms of Darwin’s thoughts, theorized fossilization of animals, computer simulations of eye evolution, and new research on supposed prior genes occurring in lower life forms leading to human life. -

Eyes and Pupillary Assessment
Eye and Pupillary Assessment GFR Training January 29, 2017 What are some things you should look for? Pupil Size Pupil Shape Reactivity Tracking Redness Trauma What assessment questions may provide more information? Sudden blurry vision? Difficult to focus? Sudden double vision? Sudden loss of vision? Seeing things? Seeing black spots? Flashes of light? Any eye pain? Sudden, severe headaches? Any recent trauma? Anatomy What might happen if there is damage to the ciliary body or the nerves that control the ciliary body? Muscles in the iris control pupil size: What is the pupil? What might happen if there is damage to these muscles or to the nerves that control them? Eye Muscles and Nerves Normal Eyes Unusual Eyes Description Condition Unilateral Dilated Pupil III Nerve Compression Bilateral Dilated Pupils Midbrain Injury Irregular Pupils Orbital Trauma Conjugate Gaze Frontal Lobe Lesion Deviation Small / Pinpoint Pontine Injury, Opiate Administration Pupils of Different Sizes Irregular/Misshapen Pupils Abnormal Tracking/Movement When scanning a room, reading, etc., human eyes move in a rapid, jerky fashion. This is called saccadic eye movements. When following (tracking) a single object, eye movements should be smooth and not saccadic. With serious head injuries, eyes often exhibit abnormal tracking movements. Jerky Tracking Other things to look for: Slow tracking Unilateral tracking Lack of tracking (no control or no movement at all) ***Be sure to check both vertically and horizontally!!*** Eyes pointing in different directions Bruising Skull Fracture Broken Nose Possible Causes? Trauma Globe Rupture Protect Swelling Ice Foreign Objects One time GFD had a call for a middle-aged man who was using a power drill, and somehow the drill ended up in his eye. -

Iris Mammillations: Significance and Associations
IRIS MAMMILLATIONS: SIGNIFICANCE AND ASSOCIATIONS 2 l NICOLA K. RAGGEL2, 1. ACHESON and A. LINN MURPHREE Los Angeles and London SUMMARY mammiform (nipple- or teat-like) protuberances. Iris mammillations are rarely described, distinctive Iris mammillations are an occasional finding with few previous reports. They are most commonly villiform protuberances that can cover the iris. In the l--6 majority of reported cases they are unilateral and found in association with melanosis oculi, with or sporadic, and are seen in association with oculodermal without periocular skin involvement in a naevus of melanosis. In past literature and current clinical Ota. They are thus often less precisely referred to as practice they are frequently confused with tbe iris iris melanosis, a term which should best be reserved nodules seen in neurofibromatosis type 1. Their clinical for increased pigmentation of the iris, irrespective of significance is not established, although it has been the presence of iris elevations overlying the pigmen 7 suggested that iris mammillations may be an external ted areas. This is supported by the rare descriptions sign of ocular hypertension or intraocular malignancy. of iris elevations in the absence of any increased iris We report a series of 9 patients between the ages of 3 pigmentation?,8 and 28 years with iris mammillations. The mammilla Iris mammillations are usually unilateral, often tions appear as regularly spaced, deep brown, smooth, presenting as heterochromia iridis. Occasional bilat 7 conical elevations on the iris, of uniform height or eral cases have been described. ,8 Iris mammillations increasing in height as the pupil margin is approached. -
Eye Based Authentication: Iris and Retina Detection
The University of Saskatchewan Department of Computer Science Technical Report #2011-04 Eye Based Authentication: Iris and Retina Recognition Minhaz Fahim Zibran 2009 Department of Computer Science The University of Saskatchewan, Canada Abstract Biometric authentication comes in play to release the users from the difficulties of remembering and protecting passwords as required by traditional authenti- cation systems. Among all the biometrics in use today, eye biometrics (iris and retina) offers the highest level of uniqueness, universality, permanence, and ac- curacy. Despite these convincing properties of iris and retina biometrics, they have not been in widespread use. Moreover, humans have more or less a natural ability to recognize individuals staring at the person's eye. So, it is interesting to investigate to what extent the eye based biometrics (iris and retina recog- nition) are capable of distinguishing individuals, and what factors are there, which hinder the adoption of these technologies. This report presents a comparative study on iris and retina biometrics based on literature review. The study aims to investigate the two biometrics, conduct a comparative analysis in a fair level of technical detail, and identify the challenges and future possibilities towards their ubiquitous use. In presenting the findings, the study contributes in three ways: (1) This report may serve as a tutorial of eye biometric for those who are new in the area, (2) The comparison between iris and retina biometrics will be helpful for individuals and organizations in choosing the appropriate eye biometric for use in their context. (3) The technical, security, and usability issues identified by the study reveal avenue for further research in order to improve eye biometrics. -

Pupil Iris Ciliary Body
Eye iris pupil ciliary body Eyeball Anterior segment Posterior segment Pars caeca retinae Eyeball Corpus ciliare Procesus ciliares Sclera Iris Cornea Eyebulb wall Posterior Anterior segment segment Tunica externa Sclera Cornea (fibrosa) Tunica media Chorioidea Iris, Corpus (vasculosa) ciliare Tunica interna Pars optica Pars caeca (nervosa) retinae retinae Eyeball Fibrous tunic - tunica externa oculi • Cornea • Sclera limbus conjunctiva Cornea 1. Stratified squamous epithelium 2. Bowman´s membrane-anterior limiting lamina 3. Substantia propria cornae − 200 - 250 layers of regularly organized collagen fibrils − fibrocytes /keratocytes/ 4. Descemet´s membrane-posterior limiting lamina − the basement membrane of the posterior endothelium − Posterior endothelium − simple squamous epithelium Cornea Vascular tunic - tunica media oculi - Choroid ch - loose c.t. with network of blood vessels, numerous pigment cells c - Ciliary body - loose c.t. with smooth muscle cells – musculus i ciliaris /accomodation/ - ciliary processes – generate aqueous humor - Iris - central opening of the iris - the pupil Choroid 1. Lamina suprachoroidea /lamina fusca sclerae/ 2. Lamina vasculosa 3. Lamina chorocapillaris 4. Lamina vitrea /Bruch´s membrane/ L. suprachoroidea - perichoroidal space with melanocytes, collagen and elastic sclera fibers, fibroblasts, macrophages, lymphocytes L. vasculosa – blood supply – parallelní veins – c. ciliare choroid L. chorocapilaris – capillary plexus for retina L. vitrea – five layers, including balsal retina lamina of chorid endothelium and retinal pigment epithelium, collagen and elastic fibers. Choroid Ciliary body - structure ciliary processes m. ciliaris ciliary epithelium - outer cell layer is pigmented, inner cell layer is nonpigmented (pars caeca retinae) Ciliary body Epithelium two layers – basal, pigmented (fuscin), surface w/o pigment - Continuous with optical part of retina = pars caeca retinae processus ciliares m. -

Anatomy & Physiology Vocabulary List
Anatomy & Physiology Vocabulary List http://www.preventblindness.org/vlc/how_we_see.htm Anterior Chamber: space in front portion of the eye between the cornea and the iris and lens, which is filled with aqueous humor Aqueous Humor: a clear, watery fluid that fills the front part of the eye between the cornea, lens and iris. Binocular Vision: coordinated use of the two eyes to see a single fused 3D image Choroid: the middle layer of the eyeball which contains veins and arteries that furnishes nourishment to the eye, especially the retina. Conjunctiva: a mucous membrane that lines the eyelids and covers the front part of the eyeball. Cornea: the transparent outer portion of the eyeball that transmits light to the retina. Ciliary Body: a ring of tissue between the iris and the choroid consisting of muscles and blood vessels that changes the shape of the lens and manufactures aqueous humor Fovea: A tiny spot located in the macula that is the area of clearest vision on the retina. Iris: the colored, circular part of the eye in front of the lens. It controls the size of the pupil. Lens: the transparent disc in the middle of the eye behind the pupil that brings rays of light into focus on the retina. Macula: is a small area of the retina located near the optic nerve at the back of the eye. It is responsible for our central, most acute vision. Optic Disk: head of optic nerve, the meeting of all retinal nerve fibers in the retina Optic Nerve: the importantt nerve tha carries messages from the retina to the brain. -

Forward and Inward Movement of the Ciliary Muscle Apex with Accommodation in Adults
Forward and Inward Movement of the Ciliary Muscle Apex with Accommodation in Adults THESIS Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Trang Pham Prosak Graduate Program in Vision Science The Ohio State University 2014 Master's Examination Committee: Melissa D. Bailey, OD, PhD, Advisor Donald O. Mutti, OD, PhD Marjean Kulp, OD, PhD Copyright by Trang Pham Prosak 2014 Abstract Purpose: to study the inward and forward movement of the ciliary muscle during accommodation and to investigate the effects of one hour of reading on the ciliary muscle behavior in young adults. Methods: Subjects included 23 young adults with a mean age of 23.7 ± 1.9 years. Images of the temporal ciliary muscle of the right eye were obtained using the Visante™ Anterior Segment Ocular Coherence Tomography while accommodative response was monitored simultaneously by the Power-Refractor. Four images were taken at each accommodative response level (0, 4.0 and 6.0 D) before and after one hour of reading. Ciliary muscle thickness was measured at every 0.25 mm posterior to the scleral spur. SSMAX, which is the distance between scleral spur and the thickest point of the muscle (CMTMAX), was also measured. The change in the ciliary muscle thickness and SSMAX with accommodation from 0 to 4.0 D and 0 to 6.0 D was calculated. Paired t-tests were used to determine if the ciliary muscle thickness and SSMAX for the 4.0 and 6.0 diopters of accommodative response were different after one hour of reading. -

HYPERPLASIA of the ANTERIOR LAYER of the IRIS STROMA*T by MALCOLM N
Br J Ophthalmol: first published as 10.1136/bjo.49.10.516 on 1 October 1965. Downloaded from Brit. J. Ophthal. (1965) 49, 516 HYPERPLASIA OF THE ANTERIOR LAYER OF THE IRIS STROMA*t BY MALCOLM N. LUXENBERG From the Bascom Palmer Eye Institute, Department of Ophthalmology, University of Miami School ofMedicine, Miami, Florida THE purpose of this report is to present the clinical and histopathological findings in a case of marked bilateral persistence of the anterior portion of the foetal vascular system. A brief review of the embryogenesis of the lesion is presented with photo- graphic correlation of the clinical and pathological findings. Case Report A 51-year-old Negro male developed painless progressive loss of vision in both eyes in the course of one month. There was no history of previous eye disease or injuries. The patient's vision was previously normal. General examination and past medical history yielded no information. No copyright. family history was available. Examination.-The visual acuity was hand movements in each eye, with left exotropia. The visual fields were full to light projection. Slit-lamp examination revealed a few fine white punctate opacities centrally in the left cornea at the level of Bowman's membrane or anterior stroma. A few areas of brownish pigmentation were present on the corneal endothelium nasally in the right eye and temporally in the left eye. The anterior chamber was of normal depth. Arising from the iris surface in the region of the collarette in both eyes was a projection of the iris stroma in an anterior and central direction. -

Ouabain-Sensitive Na-K Atpase Response in the Rabbit Iris-Ciliary Body After Lensectomy-Vitrectomy
Investigative Ophthalmology & Visual Science, Vol. 33, No. 1, January 1992 Copyright © Association for Research in Vision and Ophthalmology Ouabain-Sensitive Na-K ATPase Response in the Rabbit Iris-Ciliary Body After Lensectomy-Vitrectomy Takezo Mito, Sei-ichi Ishiguro, and Makoto Tomai We studied ouabain-sensitive Na-K adenosine triphosphatase (ATPase) activities in the iris-ciliary body of rabbit eyes after lensectomy-vitrectomy. Changes in enzyme activities were quantitatively investigated in the plasma membrane of iris-ciliary body at 0 or 7 hours and at days 1,3,7, and 14. The specific activity of Na-K ATPase rose to significantly higher levels than the control value at 7 hours following surgery, but returned to the baseline value after 7 days. In addition, we evaluated enzyme activities after lensectomy-vitrectomy during which SF6 or silicone oil was injected. The specific activ- ity of Na-K ATPase following the injection of SF6 or silicone oil was significantly higher than the control value at 7 hours and did not return to the normal value even after 14 days. Consensual reaction, demonstrated by increased Na-K ATPase activity, also was found in the contralateral unoperated eyes of SF6- and silicone oil-injected rabbits. The increased Na-K ATPase activity in the iris-ciliary body after experimental surgery may play an important role in restoring swollen tissues. Invest Ophthalmol Vis Sci 33:172-177,1992 Ouabain-sensitive Na-K adenosine triphosphatase lateral unoperated eyes after surgery. Moreover, we (ATPase) may contribute to the regulation of cell vol- compared those findings with the results of lensec- ume and the maintenance and regulation of the intra- tomy-vitrectomy during which SF6 or silicone oil was cellular and extracellular ionic environment.1 Further- injected. -
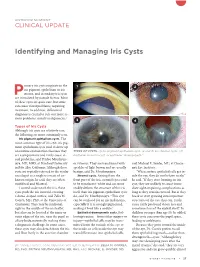
Identifying and Managing Iris Cysts
ANTERIOR SEGMENT CLINICAL UPDATE Identifying and Managing Iris Cysts rimary iris cysts originate in the 1 2 iris pigment epithelium or iris Pstroma, and secondary iris cysts are stimulated by outside factors. Most of these cysts are quite rare, but some can cause visual problems, requiring treatment. In addition, differential diagnosis is crucial to rule out more se rious problems, mainly malignancies.1 3 4 Types of Iris Cysts Although iris cysts are relatively rare, the following are more commonly seen. Iris pigment epithelium cysts. The most common type of iris cyst, iris pig ment epithelium cysts tend to show up on routine examinations because they TYPES OF CYSTS. (1) Iris pigment epithelium cyst. (2 and 3) Iris stromal cysts. (4) are asymptomatic and rarely cause vi Epithelial inclusion cyst, or epithelial “downgrowth.” sual problems, said Prithvi Mruthyun jaya, MD, MHS, at Stanford University or vitreous. They are translucent with said Michael E. Snyder, MD, at Cincin in Palo Alto, California. Although these speckles of light brown and are usually nati Eye Institute. cysts are typically referred to the ocular benign, said Dr. Mruthyunjaya. “When surface epithelial cells get in oncologist as a single iris mass of un Stromal cysts. Arising from the side the eye, they do not behave nicely,” known origin, he said, they are often front part of the iris, stromal cysts tend he said. “If they start forming an iris multifocal and bilateral. to be translucentwhite and can more cyst, they are unlikely to cause imme Located underneath the iris, these readily deform the struc ture of the iris diate sightimpairing complications as cysts push the iris forward, creating itself than iris pigment epithelium cysts long as they remain encased. -

Correlation Between Presence of Primary Iris- and Cilliary Body Cysts and Intraocular Pressure
European Review for Medical and Pharmacological Sciences 2017; 21: 3985-3989 Correlation between presence of primary iris- and cilliary body cysts and intraocular pressure R. ZHU, L. CHENG, D.-M. WANG Institute of Xuzhou Eye Prevention and Control, Department of Ophthalmology, the First People’s Hospital of Xuzhou City, Jiangsu Province, China Abstract. – OBJECTIVE: The objective of this diagnostic imaging test that makes it possible to study was to examine the correlation between visualize the anterior segment of the eye inclu- the presence of primary iris-ciliary cysts and the ding the cornea, iris, and ciliary body1. An UBM intraocular pressure. PATIENTS AND METHODS: exam allows to ophthalmologists to view parts of Sixty patients with the eye including iris and ciliary cysts that would short-sightedness undergoing routine examina- 2 tion for laser vision correction in our hospital otherwise not be visible . in 2003 were enrolled. Patients with known high It has been found in clinical practice that pa- intraocular pressure and risk of glaucoma were tients with iris and ciliary cysts usually experien- excluded from the study. A total of 119 eyes ce no severe symptoms and required no special were examined by the Ultrasound Biomicroscope treatment. However, their intraocular pressure (UBM), and the presence of the primary iris-ciliary may be slightly higher than normal, though iris cysts was confirmed. Intraocular pressure was measured by using a blowing tonometer for each and ciliary cysts also occurred in people with 3 eye in triplicate. Through Pentacam correction of normal intraocular pressure . It was reported that intraocular pressure using the Ehlers formula, the cysts were the main cause of glaucoma and closu- influence of the thickness of central cornea on re glaucoma was secondary to iris-ciliary cysts.