Process Evaluation of Community Based-Maternal and Neonatal Care Program in Rural Nepal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ethnicity, Education and Equality in Nepal
HIMALAYA, the Journal of the Association for Nepal and Himalayan Studies Volume 36 Number 2 Article 6 December 2016 New Languages of Schooling: Ethnicity, Education and Equality in Nepal Uma Pradhan University of Oxford, [email protected] Follow this and additional works at: https://digitalcommons.macalester.edu/himalaya Recommended Citation Pradhan, Uma. 2016. New Languages of Schooling: Ethnicity, Education and Equality in Nepal. HIMALAYA 36(2). Available at: https://digitalcommons.macalester.edu/himalaya/vol36/iss2/6 This work is licensed under a Creative Commons Attribution-Noncommercial 4.0 License This Research Article is brought to you for free and open access by the DigitalCommons@Macalester College at DigitalCommons@Macalester College. It has been accepted for inclusion in HIMALAYA, the Journal of the Association for Nepal and Himalayan Studies by an authorized administrator of DigitalCommons@Macalester College. For more information, please contact [email protected]. New Languages of Schooling: Ethnicity, Education, and Equality in Nepal Uma Pradhan Mother tongue education has remained this attempt to seek membership into a controversial issue in Nepal. Scholars, multiple groups and display of apparently activists, and policy-makers have favored contradictory dynamics. On the one hand, the mother tongue education from the standpoint practices in these schools display inward- of social justice. Against these views, others looking characteristics through the everyday have identified this effort as predominantly use of mother tongue, the construction of groupist in its orientation and not helpful unified ethnic identity, and cultural practices. in imagining a unified national community. On the other hand, outward-looking dynamics Taking this contention as a point of inquiry, of making claims in the universal spaces of this paper explores the contested space of national education and public places could mother tongue education to understand the also be seen. -

The Tatoeba Translation Challenge--Realistic Data Sets For
The Tatoeba Translation Challenge – Realistic Data Sets for Low Resource and Multilingual MT Jorg¨ Tiedemann University of Helsinki [email protected] https://github.com/Helsinki-NLP/Tatoeba-Challenge Abstract most important point is to get away from artificial This paper describes the development of a new setups that only simulate low-resource scenarios or benchmark for machine translation that pro- zero-shot translations. A lot of research is tested vides training and test data for thousands of with multi-parallel data sets and high resource lan- language pairs covering over 500 languages guages using data sets such as WIT3 (Cettolo et al., and tools for creating state-of-the-art transla- 2012) or Europarl (Koehn, 2005) simply reducing tion models from that collection. The main or taking away one language pair for arguing about goal is to trigger the development of open the capabilities of learning translation with little or translation tools and models with a much without explicit training data for the language pair broader coverage of the World’s languages. Using the package it is possible to work on in question (see, e.g., Firat et al.(2016a,b); Ha et al. realistic low-resource scenarios avoiding arti- (2016); Lakew et al.(2018)). Such a setup is, how- ficially reduced setups that are common when ever, not realistic and most probably over-estimates demonstrating zero-shot or few-shot learning. the ability of transfer learning making claims that For the first time, this package provides a do not necessarily carry over towards real-world comprehensive collection of diverse data sets tasks. -

Map by Steve Huffman; Data from World Language Mapping System
Svalbard Greenland Jan Mayen Norwegian Norwegian Icelandic Iceland Finland Norway Swedish Sweden Swedish Faroese FaroeseFaroese Faroese Faroese Norwegian Russia Swedish Swedish Swedish Estonia Scottish Gaelic Russian Scottish Gaelic Scottish Gaelic Latvia Latvian Scots Denmark Scottish Gaelic Danish Scottish Gaelic Scottish Gaelic Danish Danish Lithuania Lithuanian Standard German Swedish Irish Gaelic Northern Frisian English Danish Isle of Man Northern FrisianNorthern Frisian Irish Gaelic English United Kingdom Kashubian Irish Gaelic English Belarusan Irish Gaelic Belarus Welsh English Western FrisianGronings Ireland DrentsEastern Frisian Dutch Sallands Irish Gaelic VeluwsTwents Poland Polish Irish Gaelic Welsh Achterhoeks Irish Gaelic Zeeuws Dutch Upper Sorbian Russian Zeeuws Netherlands Vlaams Upper Sorbian Vlaams Dutch Germany Standard German Vlaams Limburgish Limburgish PicardBelgium Standard German Standard German WalloonFrench Standard German Picard Picard Polish FrenchLuxembourgeois Russian French Czech Republic Czech Ukrainian Polish French Luxembourgeois Polish Polish Luxembourgeois Polish Ukrainian French Rusyn Ukraine Swiss German Czech Slovakia Slovak Ukrainian Slovak Rusyn Breton Croatian Romanian Carpathian Romani Kazakhstan Balkan Romani Ukrainian Croatian Moldova Standard German Hungary Switzerland Standard German Romanian Austria Greek Swiss GermanWalser CroatianStandard German Mongolia RomanschWalser Standard German Bulgarian Russian France French Slovene Bulgarian Russian French LombardRomansch Ladin Slovene Standard -

The Maulana Who Loved Krishna
SPECIAL ARTICLE The Maulana Who Loved Krishna C M Naim This article reproduces, with English translations, the e was a true maverick. In 1908, when he was 20, he devotional poems written to the god Krishna by a published an anonymous article in his modest Urdu journal Urd -i-Mu’all (Aligarh) – circulation 500 – maulana who was an active participant in the cultural, H ū ā which severely criticised the British colonial policy in Egypt political and theological life of late colonial north India. regarding public education. The Indian authorities promptly Through this, the article gives a glimpse of an Islamicate charged him with “sedition”, and demanded the disclosure of literary and spiritual world which revelled in syncretism the author’s name. He, however, took sole responsibility for what appeared in his journal and, consequently, spent a little with its surrounding Hindu worlds; and which is under over one year in rigorous imprisonment – held as a “C” class threat of obliteration, even as a memory, in the singular prisoner he had to hand-grind, jointly with another prisoner, world of globalised Islam of the 21st century. one maund (37.3 kgs) of corn every day. The authorities also confi scated his printing press and his lovingly put together library that contained many precious manuscripts. In 1920, when the fi rst Indian Communist Conference was held at Kanpur, he was one of the organising hosts and pre- sented the welcome address. Some believe that it was on that occasion he gave India the slogan Inqilāb Zindabād as the equivalent to the international war cry of radicals: “Vive la Revolution” (Long Live The Revolution). -

The Forms of Seeking Accepting and Denying Permissions in English and Awadhi Language
THE FORMS OF SEEKING ACCEPTING AND DENYING PERMISSIONS IN ENGLISH AND AWADHI LANGUAGE A Thesis Submitted to the Department of English Education In Partial Fulfilment for the Masters of Education in English Submitted by Jyoti Kaushal Faculty of Education Tribhuwan University, Kirtipur Kathmandu, Nepal 2018 THE FORMS OF SEEKING ACCEPTING AND DENYING PERMISSIONS IN ENGLISH AND AWADHI LANGUAGE A Thesis Submitted to the Department of English Education In Partial Fulfilment for the Masters of Education in English Submitted by Jyoti Kaushal Faculty of Education Tribhuwan University, Kirtipur Kathmandu, Nepal 2018 T.U. Reg. No.:9-2-540-164-2010 Date of Approval Thesis Fourth Semester Examination Proposal: 18/12/2017 Exam Roll No.: 28710094/072 Date of Submission: 30/05/2018 DECLARATION I hereby declare that to the best of my knowledge this thesis is original; no part of it was earlier submitted for the candidate of research degree to any university. Date: ..…………………… Jyoti Kaushal i RECOMMENDATION FOR ACCEPTANCE This is to certify that Miss Jyoti Kaushal has prepared this thesis entitled The Forms of Seeking, Accepting and Denying Permissions in English and Awadhi Language under my guidance and supervision I recommend this thesis for acceptance Date: ………………………… Mr. Raj Narayan Yadav Reader Department of English Education Faculty of Education TU, Kirtipur, Kathmandu, Nepal ii APPROVAL FOR THE RESEARCH This thesis has been recommended for evaluation from the following Research Guidance Committee: Signature Dr. Prem Phyak _______________ Lecturer & Head Chairperson Department of English Education University Campus T.U., Kirtipur, Mr. Raj Narayan Yadav (Supervisor) _______________ Reader Member Department of English Education University Campus T.U., Kirtipur, Mr. -

INCLUSIVE GOVERNANCE a Study on Participation and Representation After Federalization in Nepal
STATE OF INCLUSIVE GOVERNANCE A Study on Participation and Representation after Federalization in Nepal Central Department of Anthropology Tribhuvan University Kirtipur, Kathmandu, Nepal B I STATE OF INCLUSIVE GOVERNANCE STATE OF INCLUSIVE GOVERNANCE STATE OF INCLUSIVE GOVERNANCE A Study on Participation and Representation after Federalization in Nepal Binod Pokharel Meeta S. Pradhan SOSIN Research Team Project Coordinator Dr. Dambar Chemjong Research Director Dr. Mukta S. Tamang Team Leaders Dr. Yogendra B. Gurung Dr. Binod Pokharel Dr. Meeta S. Pradhan Dr. Mukta S. Tamang Team Members Dr. Dhanendra V. Shakya Mr. Mohan Khajum Advisors/Reviewers Dr. Manju Thapa Tuladhar Mr. Prakash Gnyawali B I STATE OF INCLUSIVE GOVERNANCE STATE OF INCLUSIVE GOVERNANCE STATE OF INCLUSIVE GOVERNANCE A Study on Participation and Representation after Federalization in Nepal Copyright@2020 Central Department of Anthropology Tribhuvan University This study is made possible by the support of the American People through the United States Agency for International Development (USAID). The contents of this report are the sole responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government or Tribhuvan University. Published By Central Department of Anthropology (CDA) Tribhuvan University (TU) Kirtipur, Kathmandu, Nepal Tel: + 977-0-4334832 Email: [email protected] Website: anthropologytu.edu.np First Published: October 2020 400 Copies Cataloguing in Publication Data Pokharel, Binod. State of inclusive governance: a study on participation and representation after federalization in Nepal / Binod Pokharel, Meeta S. Pradhan.- Kirtipur : Central Department of Anthropology, Tribhuvan University, 2020. Xx, 164p. : Col. ill. ; Cm. ISBN 978-9937-0-7864-1 1. -
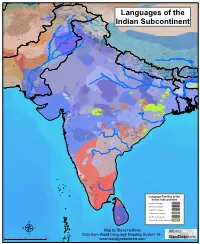
Map by Steve Huffman Data from World Language Mapping System 16
Tajiki Tajiki Tajiki Shughni Southern Pashto Shughni Tajiki Wakhi Wakhi Wakhi Mandarin Chinese Sanglechi-Ishkashimi Sanglechi-Ishkashimi Wakhi Domaaki Sanglechi-Ishkashimi Khowar Khowar Khowar Kati Yidgha Eastern Farsi Munji Kalasha Kati KatiKati Phalura Kalami Indus Kohistani Shina Kati Prasuni Kamviri Dameli Kalami Languages of the Gawar-Bati To rw al i Chilisso Waigali Gawar-Bati Ushojo Kohistani Shina Balti Parachi Ashkun Tregami Gowro Northwest Pashayi Southwest Pashayi Grangali Bateri Ladakhi Northeast Pashayi Southeast Pashayi Shina Purik Shina Brokskat Aimaq Parya Northern Hindko Kashmiri Northern Pashto Purik Hazaragi Ladakhi Indian Subcontinent Changthang Ormuri Gujari Kashmiri Pahari-Potwari Gujari Bhadrawahi Zangskari Southern Hindko Kashmiri Ladakhi Pangwali Churahi Dogri Pattani Gahri Ormuri Chambeali Tinani Bhattiyali Gaddi Kanashi Tinani Southern Pashto Ladakhi Central Pashto Khams Tibetan Kullu Pahari KinnauriBhoti Kinnauri Sunam Majhi Western Panjabi Mandeali Jangshung Tukpa Bilaspuri Chitkuli Kinnauri Mahasu Pahari Eastern Panjabi Panang Jaunsari Western Balochi Southern Pashto Garhwali Khetrani Hazaragi Humla Rawat Central Tibetan Waneci Rawat Brahui Seraiki DarmiyaByangsi ChaudangsiDarmiya Western Balochi Kumaoni Chaudangsi Mugom Dehwari Bagri Nepali Dolpo Haryanvi Jumli Urdu Buksa Lowa Raute Eastern Balochi Tichurong Seke Sholaga Kaike Raji Rana Tharu Sonha Nar Phu ChantyalThakali Seraiki Raji Western Parbate Kham Manangba Tibetan Kathoriya Tharu Tibetan Eastern Parbate Kham Nubri Marwari Ts um Gamale Kham Eastern -

Unit 31 Indian Languages and Literature
UNIT 31 INDIAN LANGUAGES AND LITERATURE Structure 31.0 Objectives 31.1 Introduction 31.2 Arabic and Persian 31.3 Sanskrit 31.4 North India 31.4.1 Hindi 31.4.2 Urdu 31.4.3 Punjabi 3 1.5 Western India 31.5.1 %uj& 315.2 Marathi 31.6 Eastern India 31.6.1 Bengali 31.6.2 Asaunek 31.6.3 Ckiya 3 1.7 South Indian Languages 31.7.1 Td 31.7.2 Teluy 31.7.3 Kamada 31.7.4 Malayalam 31.8 Let Us Sum Up 31.9 Key Words 31.10 Answers to Cbeck Your Progress Exercises In this unit, we will discuss the languages and literatme tbat flourished m India during the 16th to mid 18th centuries. Aftea gomg through this unit you will: ,. be able to appreciate the variety and richness of literam produced during the period under study; know about the main literary works in India in the following languages: Arabic, Persian, Urdu, Sanskrit, HiLdi, Punjabi, Bengali, Assamese, Oriya, Tamil, Telugu, Malayalam and Kannada; and .a be familiar wit. some of the main historians, writers and poets writing in the above languages. ' cr 31.1 INTRODUCTION The Mughal rule created some semblance of political unity m India. Further, it not only encouraged an integtated internal matket and an increase m foreign trade, but also generated an atmosphere of creative intellectual activity. Apart from the Empexors, the Mughal princes and nobles, too, patronised literary activity. Tbe regional com.of the Rajput Rajas and the ' Deccan and South Indian rulers also did not lag bebind. -

Nepal Early Grade Reading Materials Assessment
NEPAL EARLY GRADE READING MATERIALS ASSESSMENT A Report Submitted to United States Agency for International Development (USAID) Nepal Maharajgunj, Kathmandu, Nepal Submitted by Research Management Cell (RMC) Kathmandu Shiksha Campus (KSC) Ramshah Path, Kathmandu, Nepal May 9, 2014 1 Study Team Core Team SN Name of the Consultant Position/Area of Expertise 1 Prof. Dr Prem Narayan Aryal Team Leader and Early Childhood Development Expert 2 Prof. Dr Yogendra Prasad Yadava Team Member and Linguist 3 Prof. Dr Ram Krishna Maharjan Team Member and Educationist 4 Prof. Dr Hemang Raj Adhikari Team Member and Nepali Language Subject Expert 5 Dr Sushan Acharya Team Member and Gender, Child and Social Inclusion Expert 6 Mr Karnakhar Khatiwada Team Member and Linguist 7 Mr Bhagwan Aryal Team Member and Educationist 8 Mr Shatrughan Prasad Gupta Project Manager and Educationist Advisory Input - Prof. Dr Basu Dev Kafle Subject Experts (Evaluators) SN Name of the Nepali Language Name of the Mother Tongue Language Subject Experts Subject Experts 1 Prof. Dr Hemang Raj Nepali Mr Surya Prasad Yadav Maithili Adhikari 2 Prof. Dr Madhav Bhattarai Nepali Mr Jeevan Kumar Maharjan Nepal Bhasa 3 Prof. Dr Kedar Sharma Nepali Mr Padam Rai Bantawa 4 Prof. Maheshwor Neupane Nepali Mr Purna Bahadur Gharti Magar Athara Magarat 5 Prof. Dr Sanat Kumar Wasti Nepali Mr Jai Prakash Lal Srivastav Awadhi 2 6 Dr Madhav Prasad Poudel Nepali Mr Khenpo Gyurme Tsultrim Mugali 7 Mr Diwakar Dhungel Nepali Ms Bagdevi Rai Chamling 8 Mr Ganesh Prasad Bhattarai Nepali Mr Krishna Raj Sarbahari Tharu 9 Mr Hari Prasad Niraula Nepali Mr Rajesh Prasad Sah Bajjika 10 Ms Rajni Dhimal Nepali Dr Lal-Shyãkarelu Rapacha Sunuwar 11 Prof. -

Godna (Body Tattooing) Tradition of Awadh- from Mythology to Modernity
9ROXPH,,,,VVXH,9-XQH,661 GODNA (BODY TATTOOING) TRADITION OF AWADH- FROM MYTHOLOGY TO MODERNITY Dr. Neetu Singh Assistant Professor, Department Of Anthropology Vidyant Hindu PG College Lucknow India This paper has been presented in SSEASR (South and South East Asian Association for the Study of Culture and Religion) Conference, 4th -6th June 2015 at Colombo, SriLanka Abstract Traditional body tattooing is called Godna in Awadh. Body tattooing (Godna) is believed to be the adaptation of a primitive form of art in India. The art of godna is closely related to religion and considered rites of passage in nondwij castes of Awadhi region. This art comprises permanent ornamentation of the body with tattoos made by Godarins or Maharins. The belief says that godna marks are the only ornamentation which remains with them after the death and tattooed god, symbol or name will help as supernatural aid in the time of crisis, not in lifetime but even after their death. This was popular among women though some of the men in Awadh also have this art on their body. This art may provide insight into a people world view of this region. According to myth and history godna is age old tradition. Female figurines found in Bharahut dated 200 BCE had godna in their hand, leg and face1i. The record of human history shows that godna have served in various functions as rites of passage, marks of status and rank, symbols of religious and spiritual devotion, decorations for bravery etc. In modern times body tattooing became the symbol of fashion and religious significance is losing its meaning. -

Languages of India Being a Reprint of Chapter on Languages
THE LANGUAGES OF INDIA BEING A :aEPRINT OF THE CHAPTER ON LANGUAGES CONTRIBUTED BY GEORGE ABRAHAM GRIERSON, C.I.E., PH.D., D.LITT., IllS MAJESTY'S INDIAN CIVIL SERVICE, TO THE REPORT ON THE OENSUS OF INDIA, 1901, TOGETHER WITH THE CENSUS- STATISTIOS OF LANGUAGE. CALCUTTA: OFFICE OF THE SUPERINTENDENT OF GOVERNMENT PRINTING, INDIA. 1903. CALcuttA: GOVERNMENT OF INDIA. CENTRAL PRINTING OFFICE, ~JNGS STRERT. CONTENTS. ... -INTRODUCTION . • Present Knowledge • 1 ~ The Linguistio Survey 1 Number of Languages spoken ~. 1 Ethnology and Philology 2 Tribal dialects • • • 3 Identification and Nomenolature of Indian Languages • 3 General ammgemont of Chapter • 4 THE MALAYa-POLYNESIAN FAMILY. THE MALAY GROUP. Selung 4 NicobaresB 5 THE INDO-CHINESE FAMILY. Early investigations 5 Latest investigations 5 Principles of classification 5 Original home . 6 Mon-Khmers 6 Tibeto-Burmans 7 Two main branches 7 'fibeto-Himalayan Branch 7 Assam-Burmese Branch. Its probable lines of migration 7 Siamese-Chinese 7 Karen 7 Chinese 7 Tai • 7 Summary 8 General characteristics of the Indo-Chinese languages 8 Isolating languages 8 Agglutinating languages 9 Inflecting languages ~ Expression of abstract and concrete ideas 9 Tones 10 Order of words • 11 THE MON-KHME& SUB-FAMILY. In Further India 11 In A.ssam 11 In Burma 11 Connection with Munds, Nicobar, and !lalacca languages 12 Connection with Australia • 12 Palaung a Mon- Khmer dialect 12 Mon. 12 Palaung-Wa group 12 Khaasi 12 B2 ii CONTENTS THE TIllETO-BuRMAN SUll-FAMILY_ < PAG. Tibeto-Himalayan and Assam-Burmese branches 13 North Assam branch 13 ~. Mutual relationship of the three branches 13 Tibeto-H imalayan BTanch. -

A History of Nepal John Whelpton Index More Information
Cambridge University Press 0521804701 - A History of Nepal John Whelpton Index More information Index Note: Readers seeking information about particular individuals or events should also consult the ‘Key events’ (pp. x–xviii) and ‘Biographical notes’ (pp. 238–51) sections. The index also omits names of ethnic groups or castes which appear only in table 1.1 (pp. 9–10). abortion, 164 Armenians, 28 Acham, 58, 218 army Acharya, Tanka Prasad, 67, 68, 82–3, 88, 90, 94, contemporary role, 207, 225 155 deployment against Maoists, 218 personal attitudes, 155, 158–63 in early period, 50 as prime minister, 91–2, 133, 168–73 Arniko Rajmarg, 137 Adhikari, Man Mohan, 113, 193 Arthashastra, 252,n.8 administrative system, 129 Arun River, 13, 75, 179 affirmative action, 118 Arya Samaj, 79–80 see also reservations ascetics, 26, 30, 52, 80 Afghanistan, 44, 65 Ashrit, Jivraj, 190 Afghans, 15 Asian Development Bank, 128 Agincourt, Battle of, 38 Assam, 2, 13, 15–16, 112 Agricultural Perspective Plan, 201, 230 assimilation, 3, 11 agricultural tools industry, 133 Auckland, Lord, 44 agriculture, 1, 12, 15, 23, 26 aul, 14, 27 after 1951, 122, 126, 129, 134, 140–4, 200–1, Australia, 134, 148 230–2 Austroasiatic language family, 12 in early period, 16–18 Awadhi language, 15, 186 research in, 135 after unification, 54–5, 74 Back to the Village National Campaign, 108, 109 agro-industry, 147–8 Baglung, 55, 60 air transport, 79, 130, 138–9 Bagmati River, 157 Al Beruni, 180 bahudaliya janbad, 197 alcohol, use of, 159–60, 226–7 Bairagis, 52 All India Gorkha League, 75 baisi