Running Head: SYSTEMATIC ERROR in the DETECTION
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sign Language Typology Series
SIGN LANGUAGE TYPOLOGY SERIES The Sign Language Typology Series is dedicated to the comparative study of sign languages around the world. Individual or collective works that systematically explore typological variation across sign languages are the focus of this series, with particular emphasis on undocumented, underdescribed and endangered sign languages. The scope of the series primarily includes cross-linguistic studies of grammatical domains across a larger or smaller sample of sign languages, but also encompasses the study of individual sign languages from a typological perspective and comparison between signed and spoken languages in terms of language modality, as well as theoretical and methodological contributions to sign language typology. Interrogative and Negative Constructions in Sign Languages Edited by Ulrike Zeshan Sign Language Typology Series No. 1 / Interrogative and negative constructions in sign languages / Ulrike Zeshan (ed.) / Nijmegen: Ishara Press 2006. ISBN-10: 90-8656-001-6 ISBN-13: 978-90-8656-001-1 © Ishara Press Stichting DEF Wundtlaan 1 6525XD Nijmegen The Netherlands Fax: +31-24-3521213 email: [email protected] http://ishara.def-intl.org Cover design: Sibaji Panda Printed in the Netherlands First published 2006 Catalogue copy of this book available at Depot van Nederlandse Publicaties, Koninklijke Bibliotheek, Den Haag (www.kb.nl/depot) To the deaf pioneers in developing countries who have inspired all my work Contents Preface........................................................................................................10 -

Sign Language Endangerment and Linguistic Diversity Ben Braithwaite
RESEARCH REPORT Sign language endangerment and linguistic diversity Ben Braithwaite University of the West Indies at St. Augustine It has become increasingly clear that current threats to global linguistic diversity are not re - stricted to the loss of spoken languages. Signed languages are vulnerable to familiar patterns of language shift and the global spread of a few influential languages. But the ecologies of signed languages are also affected by genetics, social attitudes toward deafness, educational and public health policies, and a widespread modality chauvinism that views spoken languages as inherently superior or more desirable. This research report reviews what is known about sign language vi - tality and endangerment globally, and considers the responses from communities, governments, and linguists. It is striking how little attention has been paid to sign language vitality, endangerment, and re - vitalization, even as research on signed languages has occupied an increasingly prominent posi - tion in linguistic theory. It is time for linguists from a broader range of backgrounds to consider the causes, consequences, and appropriate responses to current threats to sign language diversity. In doing so, we must articulate more clearly the value of this diversity to the field of linguistics and the responsibilities the field has toward preserving it.* Keywords : language endangerment, language vitality, language documentation, signed languages 1. Introduction. Concerns about sign language endangerment are not new. Almost immediately after the invention of film, the US National Association of the Deaf began producing films to capture American Sign Language (ASL), motivated by a fear within the deaf community that their language was endangered (Schuchman 2004). -
Passenger Information Using a Sign Language Avatar Individual Travel Assistance for Passengers with Special Needs in Public Transport
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Institute of Transport Research:Publications STRATEGIES Travel Assistance Photo: Helmer Photo: Passenger information using a sign language avatar Individual travel assistance for passengers with special needs in public transport Public transport, passenger information, travel assistance, information and communication technology, reduced mobility, accessibility, inclusion Public transport operators are legally obliged to ensure equal access to transportation services. This includes equal access to information and communication related to those services. Deaf passengers mostly prefer to communicate in sign language. For this reason, the specific needs of deaf and hard-of- hearing passengers still are not adequately addressed – despite the tremendous efforts public transport operators have put in providing accessible communication services to their passengers. This article describes a novel approach to passenger information in sign language based on the automatic translation of natural (written) language text into sign language. This includes the use of a sign language avatar to display the information to deaf and hard-of-hearing passengers. Authors: Lars Schnieder, Georg Tschare ublic transport operators provide nature and causes of disruptions [2]. The tion on the Rights of Persons with Disabili- real-time passenger information passenger information system may be used ties oblige all ratifying countries to ensure via electronic information systems both physically within a transportation hub that persons with disabilities have the in order to keep passengers up to as well as remotely via mobile devices used opportunity to live independently and par- Pdate about the current status of the public by the passengers. -

Sign Language Acronyms
Sign language acronyms Throughout the Manual, the following abbreviations for sign languages are used (some of which are acronyms based on the name of the sign language used in the respective countries): ABSL Al Sayyid Bedouin Sign Language AdaSL Adamorobe Sign Language (Ghana) ASL American Sign Language Auslan Australian Sign Language BSL British Sign Language CSL Chinese Sign Language DGS German Sign Language (Deutsche Gebärdensprache) DSGS Swiss-German Sign Language (Deutsch-Schweizerische Gebärdensprache) DTS Danish Sign Language (Dansk Tegnsprog) FinSL Finnish Sign Language GSL Greek Sign Language HKSL Hong Kong Sign Language HZJ Croatian Sign Language (Hrvatski Znakovni Jezik) IPSL Indopakistani Sign Language Inuit SL Inuit Sign Language (Canada) Irish SL Irish Sign Language Israeli SL Israeli Sign Language ÍTM Icelandic Sign Language (Íslenskt táknmál) KK Sign Language of Desa Kolok, Bali (Kata Kolok) KSL Korean Sign Language LIS Italian Sign Language (Lingua dei Segni Italiana) LIU Jordanian Sign Language (Lughat il-Ishaara il-Urdunia) LSA Argentine Sign Language (Lengua de Señas Argentina) Libras Brazilian Sign Language (Língua de Sinais Brasileira) LSC Catalan Sign Language (Llengua de Signes Catalana) LSCol Colombian Sign Language (Lengua de Señas Colombiana) LSE Spanish Sign Language (Lengua de Signos Española) LSF French Sign Language (Langue des Signes Française) LSQ Quebec Sign Language (Langue des Signes Québécoise) NGT Sign Language of the Netherlands (Nederlandse Gebarentaal) NicSL Nicaraguan Sign Language NS Japanese Sign Language (Nihon Syuwa) NSL Norwegian Sign Language NZSL New Zealand Sign Language DOI 10.1515/9781501511806-003, © 2017 Josep Quer, Carlo Cecchetto, Caterina Donati, Carlo Geraci, Meltem Kelepir, Roland Pfau, and Markus Steinbach, published by De Gruyter. -

Sign Language Legislation in the European Union 4
Sign Language Legislation in the European Union Mark Wheatley & Annika Pabsch European Union of the Deaf Brussels, Belgium 3 Sign Language Legislation in the European Union All rights reserved. No part of this book may be reproduced or transmitted by any person or entity, including internet search engines or retailers, in any form or by any means, electronic or mechanical, including photocopying, recording, scanning or by any information storage and retrieval system without the prior written permission of the authors. ISBN 978-90-816-3390-1 © European Union of the Deaf, September 2012. Printed at Brussels, Belgium. Design: Churchill’s I/S- www.churchills.dk This publication was sponsored by Significan’t Significan’t is a (Deaf and Sign Language led ) social business that was established in 2003 and its Managing Director, Jeff McWhinney, was the CEO of the British Deaf Association when it secured a verbal recognition of BSL as one of UK official languages by a Minister of the UK Government. SignVideo is committed to delivering the best service and support to its customers. Today SignVideo provides immediate access to high quality video relay service and video interpreters for health, public and voluntary services, transforming access and career prospects for Deaf people in employment and empowering Deaf entrepreneurs in their own businesses. www.signvideo.co.uk 4 Contents Welcome message by EUD President Berglind Stefánsdóttir ..................... 6 Foreword by Dr Ádám Kósa, MEP ................................................................ -

TEFL for Deaf Pupils in Norwegian Bilingual Schools: Can Deaf Primary School Pupils Acquire a Foreign Sign Language?
PATRICIA PRITCHARD British to-handed alphabet TEFL for deaf pupils in Norwegian bilingual schools: Can deaf primary school pupils acquire a foreign sign language? Norwegian one-handed alphabet Masters Thesis in Special Education Dept. of Education, Faculty of Social Sciences & Technology Management, Norwegian University of Science & Technology, Trondheim, Norway December 2004 Summary TEFL for deaf pupils in Norwegian bilingual schools: Can deaf primary school pupils acquire and understand a foreign sign language? Both hearing and deaf people in Norway need skills in English to cope with the demands of modern society. The question is how can deaf pupils best acquire English? A National Curriculum was implemented in 1997 (L97) based on sign bilingualism and a socio-cultural approach to language learning. British Sign Language (BSL) was introduced into the English syllabus for Primary School deaf pupils as a first step in foreign language learning, before the introduction of English. The curriculum for deaf pupils (EfDP) was implemented without research underpinning and further education of in-service teachers, although some teaching aids were produced. This study looks at the BSL receptive skills of Norwegian Deaf pupils in class 4. and tries to pinpoint variables that played a part in their acquisition of BSL. The study makes use of theories created for hearing children acquiring a second spoken language. This is seen as defensible because they deal with the acquisition of languages of the same modality. A quantitative method was chosen to answer the research question of whether deaf Norwegian pupils in class 4 understood BSL and three language tests were used to measure their BSL receptive skills. -

Marcin Mizak Sign Language – a Real and Natural Language
LUBELSKIE MATERIAŁY NEOFILOLOGICZNE NR 35, 2011 Marcin Mizak Sign Language – A Real and Natural Language 1. Introduction It seems reasonable to begin a discussion on the “realness” and “naturalness” of sign language by comparing it to other human languages of whose “real” and “natural” status there can be no doubt whatsoever. They will be our reference point in the process of establishing the status of sign language. The assumption being made in this paper is that all real and natural languages share certain characteristics with one another, that they all behave in a certain way and that certain things happen to all of them. If it transpires that the same characteristics and behaviours are also shared by sign language and that whatever happens to real and natural languages also happens to sign language then the inevitable conclusion follows: sign language is indeed a real and natural language 1. 2. The number of languages in the world One of the first things to be noticed about real and natural languages is their great number. Ethnologue: Languages of the World , one of the most reliable and comprehensive encyclopedic reference publications, catalogues in its 16 th edition of 2009 6,909 known living languages in 1 The designation “sign language,” as used in this article, refers to the languages used within communities of the deaf. American Sign Language, for example, is a sign language in this sense. Artificially devised systems, such as Signed English, or Manual English, are not sign languages in this sense. Sign Language – A Real and Natural Language 51 the world today 2. -

Jutta Ransmayr Monolingual Country? Multilingual Society
Jutta Ransmayr Monolingual country? Multilingual society. Aspects of language use in public administration in Austria. o official languages o languages spoken in Austria o numbers of speakers Federal Constitutional Law Art. 8 (1) German is the official language of the Republic without prejudice to the rights provided by Federal law for linguistic minorities. (2) The Republic of Austria (the Federation, Länder and municipalities) is committed to its linguistic and cultural diversity which has evolved in the course of time and finds its expression in the autochthonous ethnic groups. The language and culture, continued existence and protection of these ethnic groups shall be respected, safeguarded and promoted. (3) The Austrian Sign Language (Österreichische Gebärdensprache,ÖGS) is a language in its own right, recognized in law. For details, see the relevant legal provisions. Official language(s) of the Republic of Austria 1. German 2. Languages of the Austrian autochthonous ethnic groups 3. Austrian sign language Resident population – everyday language – nationality (2001) Everyday language Resident population Austrian citizens total: 8.032.926 total: 7.322.000 German 7.115.780 6.991.388 88,58% 95,48% Languages of the Austrian autochthonous 119.667 82.522 ethnic groups 1,49% 1,13% Austrian sign language approx. 10.000 Languages of the former Yugoslav states 348.629 41.944 4,34% 0,57% Turkish, Kurdish 185.578 61.167 2,31% 0,84% World languages 79.514 43.469 0,99% 0,59% Languages of resident population 2001 in % German languages of autochthonous -
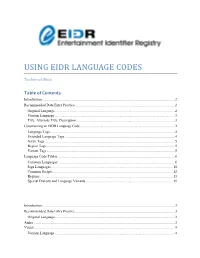
Using Eidr Language Codes
USING EIDR LANGUAGE CODES Technical Note Table of Contents Introduction ................................................................................................................................................... 2 Recommended Data Entry Practice .............................................................................................................. 2 Original Language..................................................................................................................................... 2 Version Language ..................................................................................................................................... 3 Title, Alternate Title, Description ............................................................................................................. 3 Constructing an EIDR Language Code ......................................................................................................... 3 Language Tags .......................................................................................................................................... 4 Extended Language Tags .......................................................................................................................... 4 Script Tags ................................................................................................................................................ 5 Region Tags ............................................................................................................................................. -

Deaf Learning": Using a Visual Method to Teach Written Language to the Deaf
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Archivio istituzionale della ricerca - Università degli Studi di Venezia Ca' Foscari "DEAF LEARNING": USING A VISUAL METHOD TO TEACH WRITTEN LANGUAGE TO THE DEAF Marlene Hilzensauer1, Klaudia Krammer2, Laura Volpato3, Melanie Chan4 1Centre for Sign Language and Deaf Communication, Alpen-Adria-Universität Klagenfurt (Austria) 2Centre for Sign Language and Deaf Communication, Alpen-Adria-Universität Klagenfurt (Austria) 3Department of Linguistics and Comparative Cultural Studies, Ca’ Foscari University, Venice (Italy) 4Centre for Sign Language and Deaf Communication, Alpen-Adria-Universität Klagenfurt (Austria) Abstract The majority of deaf people prefer to use the visual channel for communication, choosing a national sign language instead of a spoken language. In many countries, Deaf education is still not bilingual, therefore deaf people frequently have problems with learning and using the written language of their country. The Erasmus+ project "Deaf Learning" addresses the need for a visually-oriented written language course for the levels from A1 to B2. The main target group is that of young deaf adults aged 16 to 25 years. A secondary target group are older deaf people who are interested in improving their written language competence. Keywords: Deaf education, Written language teaching, Sign language, Interactive course. 1. Introduction Most deaf people use one of the national sign languages as their first or preferred language. Unfortunately, in most European schools, the language of instruction is still the spoken/written language of that country. This poses huge problems for deaf students. As they do not have access to the acoustic channel, they can suffer serious consequences in their national language acquisition process (Caselli, Maragna, & Volterra, 1994; Volterra, Capirci, & Cappelli, 2001; Chesi, 2006; Bertone & Volpato, 2012). -

The Power of Language Policy: the Legal Recognition of Sign Languages and the Aspirations of Deaf Communities Jyväskylä: University of Jyväskylä, 2016, 134 P
JYVÄSKYLÄ STUDIES IN HUMANITIES 301 Maartje De Meulder The Power of Language Policy The Legal Recognition of Sign Languages and the Aspirations of Deaf Communities JYVÄSKYLÄ STUDIES IN HUMANITIES 301 Maartje De Meulder The Power of Language Policy The Legal Recognition of Sign Languages and the Aspirations of Deaf Communities Esitetään Jyväskylän yliopiston humanistisen tiedekunnan suostumuksella julkisesti tarkastettavaksi Historica-rakennuksen salissa H320 joulukuun 16. päivänä 2016 kello 12. Academic dissertation to be publicly discussed, by permission of the Faculty of Humanities of the University of Jyväskylä, in building Historica, auditorium H320, on December 16, 2016 at 12 o’clock noon. UNIVERSITY OF JYVÄSKYLÄ JYVÄSKYLÄ 2016 The Power of Language Policy The Legal Recognition of Sign Languages and the Aspirations of Deaf Communities JYVÄSKYLÄ STUDIES IN HUMANITIES 301 Maartje De Meulder The Power of Language Policy The Legal Recognition of Sign Languages and the Aspirations of Deaf Communities UNIVERSITY OF JYVÄSKYLÄ JYVÄSKYLÄ 2016 Editors Ritva Takkinen Department of Languages, University of Jyväskylä Pekka Olsbo, Annikki Järvinen Publishing Unit, University Library of Jyväskylä Jyväskylä Studies in Humanities Editorial Board Editor in Chief Heikki Hanka, Department of Art and Culture Studies, University of Jyväskylä Petri Karonen, Department of History and Ethnology, University of Jyväskylä Paula Kalaja, Department of Languages, University of Jyväskylä Petri Toiviainen, Department of Music, University of Jyväskylä Tarja Nikula, Centre for Applied Language Studies, University of Jyväskylä Epp Lauk, Department of Communication, University of Jyväskylä URN:ISBN: 978-951-39-6876-2 ISBN 978-951-39-6876-2 (PDF) ISSN 1459-4331 ISBN 978-951-39-6875-5 (nid.) ISSN 1459-4323 Copyright © 2016, by University of Jyväskylä Jyväskylä University Printing House, Jyväskylä 2016 ABSTRACT De Meulder, Maartje The power of language policy: The legal recognition of sign languages and the aspirations of deaf communities Jyväskylä: University of Jyväskylä, 2016, 134 p. -

Constructed Action in American Sign Language: a Look at Second Language Learners in a Second Modality
Rochester Institute of Technology RIT Scholar Works Articles Faculty & Staff Scholarship 11-12-2019 Constructed Action in American Sign Language: A Look at Second Language Learners in a Second Modality Kim B. Kurz Rochester Institute of Technology Kellie Mullaney Corrine Occhino Rochester Institute of Technology Follow this and additional works at: https://scholarworks.rit.edu/article Recommended Citation Kurz, K.B.; Mullaney, K.; Occhino, C. Constructed Action in American Sign Language: A Look at Second Language Learners in a Second Modality. Languages 2019, 4, 90. This Article is brought to you for free and open access by the Faculty & Staff Scholarship at RIT Scholar Works. It has been accepted for inclusion in Articles by an authorized administrator of RIT Scholar Works. For more information, please contact [email protected]. languages Article Constructed Action in American Sign Language: A Look at Second Language Learners in a Second Modality Kim B. Kurz 1,*, Kellie Mullaney 1 and Corrine Occhino 2 1 Department of American Sign Language & Interpretation Education, Rochester Institute of Technology, National Technical Institute for the Deaf, Rochester, NY 14623, USA; [email protected] 2 Center on Cognition and Language, Rochester Institute of Technology, National Technical Institute for the Deaf, Rochester, NY 14623, USA; [email protected] * Correspondence: [email protected] Received: 20 April 2019; Accepted: 31 October 2019; Published: 12 November 2019 Abstract: Constructed action is a cover term used in signed language linguistics to describe multi-functional constructions which encode perspective-taking and viewpoint. Within constructed action, viewpoint constructions serve to create discourse coherence by allowing signers to share perspectives and psychological states.