Chapter 7 Body Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diapositiva 1
Thoracic Cage and Thoracic Inlet Professor Dr. Mario Edgar Fernández. Parts of the body The Thorax Is the part of the trunk betwen the neck and abdomen. Commonly the term chest is used as a synonym for thorax, but it is incorrect. Consisting of the thoracic cavity, its contents, and the wall that surrounds it. The thoracic cavity is divided into 3 compartments: The central mediastinus. And the right and left pulmonary cavities. Thoracic Cage The thoracic skeleton forms the osteocartilaginous thoracic cage. Anterior view. Thoracic Cage Posterior view. Summary: 1. Bones of thoracic cage: (thoracic vertebrae, ribs, and sternum). 2. Joints of thoracic cage: (intervertebral joints, costovertebral joints, and sternocostal joints) 3. Movements of thoracic wall. 4. Thoracic cage. Thoracic apertures: (superior thoracic aperture or thoracic inlet, and inferior thoracic aperture). Goals of the classes Identify and describe the bones of the thoracic cage. Identify and describe the joints of thoracic cage. Describe de thoracic cage. Describe the thoracic inlet and identify the structures passing through. Vertebral Column or Spine 7 cervical. 12 thoracic. 5 lumbar. 5 sacral 3-4 coccygeal Vertebrae That bones are irregular, 33 in number, and received the names acording to the position which they occupy. The vertebrae in the upper 3 regions of spine are separate throughout the whole of life, but in sacral anda coccygeal regions are in the adult firmly united in 2 differents bones: sacrum and coccyx. Thoracic vertebrae Each vertebrae consist of 2 essential parts: An anterior solid segment: vertebral body. The arch is posterior an formed of 2 pedicles, 2 laminae supporting 7 processes, and surrounding a vertebral foramen. -

Cranial Suture Mesenchymal Stem Cells: Insights and Advances
biomolecules Review Cranial Suture Mesenchymal Stem Cells: Insights and Advances Bo Li 1, Yigan Wang 1, Yi Fan 2, Takehito Ouchi 3 , Zhihe Zhao 1,* and Longjiang Li 4,* 1 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Orthodontics, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China; [email protected] (B.L.); [email protected] (Y.W.) 2 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Cariology and Endodontics, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China; [email protected] 3 Department of Physiology, Tokyo Dental College, Tokyo 1010061, Japan; [email protected] 4 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Head and Neck Oncology, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China * Correspondence: [email protected] (Z.Z.); [email protected] (L.L.) Abstract: The cranial bones constitute the protective structures of the skull, which surround and protect the brain. Due to the limited repair capacity, the reconstruction and regeneration of skull defects are considered as an unmet clinical need and challenge. Previously, it has been proposed that the periosteum and dura mater provide reparative progenitors for cranial bones homeostasis and injury repair. In addition, it has also been speculated that the cranial mesenchymal stem cells reside in the perivascular niche of the diploe, namely, the soft spongy cancellous bone between the interior and exterior layers of cortical bone of the skull, which resembles the skeletal stem cells’ distribution pattern of the long bone within the bone marrow. -

Modelling Suture Ossification: a View from the Cranial Capsule
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Masters Theses Graduate School 8-1992 Modelling Suture Ossification: A View from the Cranial Capsule Hugh Bryson Matternes University of Tennessee, Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_gradthes Part of the Anthropology Commons Recommended Citation Matternes, Hugh Bryson, "Modelling Suture Ossification: A View from the Cranial Capsule. " Master's Thesis, University of Tennessee, 1992. https://trace.tennessee.edu/utk_gradthes/4192 This Thesis is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Masters Theses by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a thesis written by Hugh Bryson Matternes entitled "Modelling Suture Ossification: A View from the Cranial Capsule." I have examined the final electronic copy of this thesis for form and content and recommend that it be accepted in partial fulfillment of the requirements for the degree of Master of Arts, with a major in Anthropology. Richard L. Jantz, Major Professor We have read this thesis and recommend its acceptance: Lyle W. Konigsberg, William M. Bass Accepted for the Council: Carolyn R. Hodges Vice Provost and Dean of the Graduate School (Original signatures are on file with official studentecor r ds.) To the Graduate Council: -

Cranial Sutures & Funny Shaped Heads: Radiological Diagnosis
Objectives • The objectives of this presentation are to: – Review the imaging features of normal cranial sutures – Identify the characteristics of abnormal skull shape on imaging – Review the characteristics of the most common non- syndromic and syndromic causes of craniosynostosis Anatomical Review Anatomical Review • The bony plates of the skull communicate at the cranial sutures • The anterior fontanelle occurs where the coronal & metopic sutures meet • The posterior fontanelle occurs where the sagittal & lambdoid sutures meet Anatomical Review • The main cranial sutures & fontanelles include: Metopic Suture Anterior Fontanelle Coronal Sutures Squamosal Sutures Posterior Fontanelle Sagittal Suture Lambdoid Sutures Anatomical Review • Growth of the skull occurs perpendicular to the cranial suture • This is controlled by a complex signalling system including: – Ephrins (mark the suture boundary) – Fibroblast growth factor receptors (FGFR) – Transcription factor TWIST Anatomical Review • The cranial sutures are important for rapid skull growth in-utero & infancy • The cranial sutures can usually be visualised on imaging into late adulthood Normal Radiological Appearances Normal Radiological Appearances • The cranial sutures can be visualised on plain radiographs • Standard views include: – PA – Lateral – Townes PA Skull radiograph Sagittal Suture Left Coronal Suture Right CoronalRight lambdoidSutureSuture Metopic Suture Left lambdoid Suture Townes View Sagittal Suture Left Coronal Suture Right Coronal Suture Right Lambdoid Suture Left -

A Heads up on Craniosynostosis
Volume 1, Issue 1 A HEADS UP ON CRANIOSYNOSTOSIS Andrew Reisner, M.D., William R. Boydston, M.D., Ph.D., Barun Brahma, M.D., Joshua Chern, M.D., Ph.D., David Wrubel, M.D. Craniosynostosis, an early closure of the growth plates of the skull, results in a skull deformity and may result in neurologic compromise. Craniosynostosis is surprisingly common, occurring in one in 2,100 children. It may occur as an isolated abnormality, as a part of a syndrome or secondary to a systemic disorder. Typically, premature closure of a suture results in a characteristic cranial deformity easily recognized by a trained observer. it is usually the misshapen head that brings the child to receive medical attention and mandates treatment. This issue of Neuro Update will present the diagnostic features of the common types of craniosynostosis to facilitate recognition by the primary care provider. The distinguishing features of other conditions commonly confused with craniosynostosis, such as plagiocephaly, benign subdural hygromas of infancy and microcephaly, will be discussed. Treatment options for craniosynostosis will be reserved for a later issue of Neuro Update. Types of Craniosynostosis Sagittal synostosis The sagittal suture runs from the anterior to the posterior fontanella (Figure 1). Like the other sutures, it allows the cranial bones to overlap during birth, facilitating delivery. Subsequently, this suture is the separation between the parietal bones, allowing lateral growth of the midportion of the skull. Early closure of the sagittal suture restricts lateral growth and creates a head that is narrow from ear to ear. However, a single suture synostosis causes deformity of the entire calvarium. -
Thorax Is Upper Part of Trunk •Study of Thorax by Studying: –Wall of the Thorax –Contents of Thorax Wall of Thorax
Thoracic cage Intercostal Space Blood vessels & Nerves. General Overview •Thorax is upper part of trunk •Study of thorax by studying: –Wall of the thorax –Contents of thorax Wall of thorax •Skeletal framework-Thoracic cage •Muscles, membrane & ligaments Thoracic cage Thoracic Cage • Conical in shape with truncated apex • Boundaries: • Anteriorly : Sternum • Posteriorly: Twelve Thoracic Vertebrae • On sides : Twelve pairs of Ribs & Costal Cartilages Thoracic cage • The thoracic wall is covered from outside to inside by • skin • superficial facia • deep fascia & • extrinsic muscle. • Muscles of the upper limb: • Pectoralis major Pectoralis minor • Trapezius, Serratus anterior, lattisimus dorsi • Levator scapulae, Rhomboideus major & minor • Serratus posterior superior & Inferior. • Muscles of the abdomen: • Rectus abdominis & external oblique • Muscle of the back: Erector spinae Ribs • True Ribs: articulating with sternum anteriorly – Vertebrosternal ribs: 1-7 ribs • False Ribs: Do not articulate with sternum anteriorly – Vertebrochondral ribs: 8-10 ribs – Floating ribs: 11-12 ribs Ribs First & 12th ribs Apertures of thorax • Superior Aperture (Inlet of Thorax) communicates thorax & neck. Structures passing between neck & thorax are contents of inlet. Partly covered by suprapleural membrane. • Inferior Aperture: Closed by Diaphragm. Structures passing between thorax & Abdomen pass through openings in diaphragm Joints of thorax Joints Joints Joints of thorax • Intervertebral joints: joints between bodies of vertebrae. It is Symphyseal type of joint. • Joint between articular processes of vertebrae is Plane synovial joint • Costovertebral joint: It is plane synovial joint between rib & vertebrae. • Manubriosternal joint: Between manubrium & Body of sternum, Symphyseal joint. • Xiphisternal joint: Between body of sternum & xiphoid process, symphyseal joint Joints of thorax • Sternocostal joints: – First Sternocostal joint between first rib & sternum is primary cartilaginous joint which is responsible for movement of sternum during respiration. -

The Sima De Los Huesos Crania: Analysis of the Cranial Breakage Patterns
Journal of Archaeological Science 72 (2016) 25e43 Contents lists available at ScienceDirect Journal of Archaeological Science journal homepage: http://www.elsevier.com/locate/jas The Sima de los Huesos Crania: Analysis of the cranial breakage patterns * Nohemi Sala a, b, c, , Ana Pantoja-Perez c, a, d, Juan Luis Arsuaga c, d, Adrian Pablos e, f, a, c, Ignacio Martínez a, c a Area de Antropología Física, Departamento de Ciencias de la Vida, Universidad de Alcala, Madrid, Spain € b Institut für Ur- und Frühgeschichte und Archaologie€ des Mittelalters Abteilung für Altere Urgeschichte und Quartar€ okologie,€ Eberhard-Karls Universitat€ Tübingen, Schloss Hohentübingen, 72070 Tübingen, Germany c Centro Mixto UCM-ISCIII de Evolucion y Comportamiento Humanos, Madrid, Spain d Departamento de Paleontología, Facultad Ciencias Geologicas, Universidad Complutense de Madrid, Spain e Centro Nacional de Investigacion sobre Evolucion Humana-CENIEH, Burgos, Spain f Paleoanthropology, Senckenberg Center for Human Evolution and Paleoenvironment, Eberhard Karls Universitat€ Tübingen, Germany article info abstract Article history: The Sima de los Huesos (SH) site has provided the largest collection of hominin crania in the fossil record, Received 29 March 2016 offering an unprecedented opportunity to perform a complete Forensic-Taphonomic study on a popu- Received in revised form lation from the Middle Pleistocene. The fractures found in seventeen crania from SH display a post- 1 June 2016 mortem fracturation pattern, which occurred in the dry bone stage and is compatible with collective Accepted 3 June 2016 burial assemblages. Nevertheless, in addition to the postmortem fractures, eight crania also display some Available online 14 June 2016 typical perimortem traumas. By using CT images we analyzed these fractures in detail. -

A) UNIAXIAL* SYNOVIAL JOINTS Type
Color Code Important JOINTS Doctors Notes Editing file Notes/Extra explanation Objectives By the end of the lecture, students should be able to: Define the term “Joint” . Describe the classification of the 3 types of joints & give an example of each. Describe the characteristics of synovial joints. Describe the classification of synovial joints & give an example of each. List factors maintaining stability of joints. Recite “Hilton’s law” for nerve supply of joints. Definition What is a joint? It is the site where two or more bones meet together. Another def. : it is the meeting of two or more articulating joints Classification of joints Joints are classified according to the tissues that lie between the bones into: A. Fibrous B. Cartilaginous C. Synovial 1) Fibrous Joints The articulating surfaces are joined by fibrous connective tissue, where No or very mild movement. 1. Skull sutures: Temporary (as it ossify later) 2. Inferior tibiofibular joints (syndesmosis): minimal movement, permanent joints. 3. Gomphosis: dental alveolar joints. Articulation between root of the tooth with mandible or maxilla مهمة اﻷمثلة تجي عليها أسئلة )المثال وﻷي نوع( • 2) Cartilaginous Joints When two bones are joined by cartilage the formed joint is called “cartilaginous joint” and are classified into 2 types: o Primary Cartilaginous (synchondrosis): o The bones are united by a plate or a bar of hyaline cartilage. o No movement, temporary joints (ossify later). o Example: plate of hyaline cartilage o Between the Epiphysis and the Diaphysis of a growing bone. hyaline cartilage. o Between the First Rib and the Sternum (1st sternocostal joint). Any articulating surface will has a plate of hyaline cartilage plate of fibrocartilage (The rest of the sternocostal joints are synovial plane joints.) o Secondary Cartilaginous: o The bones are united by a plate of fibrocartilage. -
Crista Galli (Part of Cribriform Plate of Ethmoid Bone)
Alveolar margins alveolar margins coronal suture coronal suture coronoid process crista galli (part of cribriform plate of ethmoid bone) ethmoid bone ethmoid bone ethmoid bone external acoustic meatus external occipital crest external occipital protuberance external occipital protuberance frontal bone frontal bone frontal bone frontal sinus frontal squama of frontal bone frontonasal suture glabella incisive fossa inferior nasal concha inferior nuchal line inferior orbital fissure infraorbital foramen internal acoustic meatus lacrimal bone lacrimal bone lacrimal fossa lambdoid suture lambdoid suture lambdoid suture mandible mandible mandible mandibular angle mandibular condyle mandibular foramen mandibular notch mandibular ramus mastoid process of the temporal bone mastoid process of the temporal bone maxilla maxilla maxilla mental foramen mental foramen middle nasal concha of ethmoid bone nasal bone nasal bone nasal bone nasal bone occipital bone occipital bone occipital bone occipitomastoid suture occipitomastoid suture occipitomastoid suture occipital condyle optic canal optic canal palatine bone palatine process of maxilla parietal bone parietal bone parietal bone parietal bone perpendicular plate of ethmoid bone pterygoid process of sphenoid bone sagittal suture sella turcica of sphenoid bone Sphenoid bone (greater wing) spehnoid bone (greater wing) sphenoid bone (greater wing) sphenoid bone (greater wing) sphenoid sinus sphenoid sinus squamous suture squamous suture styloid process of temporal bone superior nuchal line superior orbital fissure supraorbital foramen (notch) supraorbital margin sutural bone temporal bone temporal bone temporal bone vomer bone vomer bone zygomatic bone zygomatic bone. -
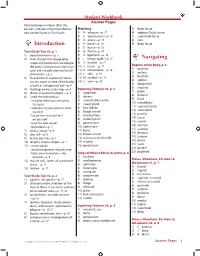
Student Workbook Answer Pages Italicized Page Numbers After the Answers Indicate Where the Informa- Matching 5) Deep Fascia Tion Can Be Found in Trail Guide
Student Workbook Answer Pages Italicized page numbers after the answers indicate where the informa- Matching 5) deep fascia tion can be found in Trail Guide. 1) N adipose—p. 17 6) adipose (fatty) tissue 2) F aponeurosis—p. 13 7) superficial fascia 3) D artery—p. 16 8) skin 4) H bone—p. 10 9) deep fascia Introduction 5) E bursa—p. 16 Tour Guide Tips #1, p. 1 6) B fascia—p. 14 1) bony landmarks—p. 2 7) G ligament—p. 13 2) Even though the topography, 8) I lymph node—p. 17 Navigating shape and proportion are unique, 9) A muscle—p. 11 Regions of the Body, p. 6 the body’s composition and struc- 10) J nerve—p. 17 1) pectoral tures are virtually identical on all 11) K retinaculum—p. 15 2) axillary individuals.—p. 2 12) L skin—p. 10 3) brachial 3) To examine or explore by touch- 13) M tendon—p. 13 4) cubital ing (an organ or area of the body), 14) C vein—p. 16 5) abdominal usually as a diagnostic aid—p. 4 6) inguinal 4) locating, aware, assessing—p. 4 Exploring Textures #1, p. 3 7) pubic 5) directs movement, depth.—p. 4 1) epidermis 8) femoral 6) • read the information 2) dermis 9) facial • visualize what you are trying 3) arrector pili muscle 10) mandibular to access 4) sweat gland 11) supraclavicular • verbalize to your partner what 5) hair follicle 12) antecubital you feel 6) blood vessels 13) patellar • locate the structure first 7) muscle fibers 14) crural on yourself 8) endomysium 15) cranial • read the text aloud 9) perimysium 16) cervical • be patient—p. -

Craniosynostosis (Sometimes Called Craniostenosis) Is a Disorder in Which There Is Early Fusion of the Sutures of the Skull in Childhood
Craniosynostosis (sometimes called craniostenosis) is a disorder in which there is early fusion of the sutures of the skull in childhood. It produces an abnormally shaped head and, at times, appearance of the face. The deformity varies significantly depending on the suture or sutures involved. Surgical correction may be necessary to improve appearance and provide space for the growing brain. Anatomy • The bones of the skull are the frontal, parietal, temporal, occipital, and sphenoid bones (Figure 1) • The place where two bones come together is called a suture • At birth the adjacent bones override each other to allow the infant to pass through the birth canal. hinges called sutures, which allow the head to pass through the birth canal As the child grows the sutures allow for skull expansion to accommodate the growing brain. • The brain doubles in size by age 6 months and again at age 2 years. These sutures normally begin to fuse around 2 years of age along with the closure of the fontanel (soft spot) • The seam where two skull bones fuse together is called a suture. The major sutures are called sagittal, coronal, metopic and lambdoid (Figure 2) • The sutures are completely fused by 6-8 yrs of age • Within the skull lie: 1. Brain 2. Meninges o The dura is a membrane that lines the inside of the skull o The pia-arachnoid is a filmy membrane that covers the brain 3. Blood vessels of the brain 4. Cerebrospinal fluid (CSF), a watery fluid that is produced by and bathes the brain Figure 1 - Anatomy of the skull in an infant Figure 2 - Infant skull showing the position showing the various bones that fuse of the major sutures. -
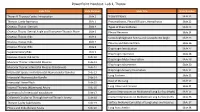
Powerpoint Handout: Lab 1, Thorax
PowerPoint Handout: Lab 1, Thorax Slide Title Slide Number Slide Title Slide Number Thorax & Thoracic Cavity: Introduction Slide 2 Visceral Pleura Slide 21 Thoracic Cavity Apertures Slide 3 Pneumothorax, Pleural Effusion, Hemothorax Slide 22 Osseous Thorax: Sternum Slide 4 Types of Pneumothorax Slide 23 Osseous Thorax: Sternal Angle and Transverse Thoracic Plane Slide 5 Pleural Recesses Slide 24 Osseous Thorax: Ribs Slide 6 Costodiaphragmatic Recess and Costophrenic Angle Slide 25 Osseous Thorax: Ribs Slide 7 Pleurisy and Referred Pain Slide 26 Osseous Thorax: Ribs Slide 8 Diaphragm Introduction Slide 27 Supernumerary Ribs Slide 9 Diaphragm Apertures Slide 28 Osseous Thorax: Rib Joints Slide 10 Diaphragm Motor Innervation Slide 29 Muscular Thorax: Intercostal Muscles Slide 11 Diaphragm Movements Slide 30 Muscular Thorax: Intercostal Muscles (Continued) Slide 12 Diaphragm Sensory Innervation Slide 31 Intercostal Spaces and Intercostal Neurovascular Bundles Slide 13 Lung Surfaces Slide 32 Intercostal Neurovascular Bundle Slide 14 Root of the Lung Slide 33 Intercostal Nerve Block Slide 15 Slide 34 Internal Thoracic (Mammary) Artery Slide 16 Lung Lobes and Fissures Summary of of Intercostal Vasculature Slide 17 Contact Impressions on Mediastinal Lung Surface (Right) Slide 35 Collateral Circulation Through Internal Thoracic Artery Slide 18 Contact Impressions on Mediastinal Lung Surface (Left) Slide 36 Thoracic Cavity Subdivisions Slide 19 Surface Anatomy Correlates of Lung Lobes and Fissures Slide 37 Pleura and Endothoracic Fascia Slide 20 Lung Auscultation Slide 38 Thorax & Thoracic Cavity: Introduction The thorax refers to the region of the body between the neck https://3d4medic.al/enFsQOFf and the abdomen. The thoracic cavity is an irregularly shaped cylinder enclosed by the musculoskeletal walls of the thorax and the diaphragm.