A Joint Or Articulation Is a Place in the Body Where Two Bones Come Together
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Suture Mesenchymal Stem Cells: Insights and Advances
biomolecules Review Cranial Suture Mesenchymal Stem Cells: Insights and Advances Bo Li 1, Yigan Wang 1, Yi Fan 2, Takehito Ouchi 3 , Zhihe Zhao 1,* and Longjiang Li 4,* 1 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Orthodontics, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China; [email protected] (B.L.); [email protected] (Y.W.) 2 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Cariology and Endodontics, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China; [email protected] 3 Department of Physiology, Tokyo Dental College, Tokyo 1010061, Japan; [email protected] 4 State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, Department of Head and Neck Oncology, West China Hospital of Stomatology, Sichuan University, Chengdu 610041, China * Correspondence: [email protected] (Z.Z.); [email protected] (L.L.) Abstract: The cranial bones constitute the protective structures of the skull, which surround and protect the brain. Due to the limited repair capacity, the reconstruction and regeneration of skull defects are considered as an unmet clinical need and challenge. Previously, it has been proposed that the periosteum and dura mater provide reparative progenitors for cranial bones homeostasis and injury repair. In addition, it has also been speculated that the cranial mesenchymal stem cells reside in the perivascular niche of the diploe, namely, the soft spongy cancellous bone between the interior and exterior layers of cortical bone of the skull, which resembles the skeletal stem cells’ distribution pattern of the long bone within the bone marrow. -

Pictorial Essay
EDUCATIONAL REVIEW ER_024 Pictorial essay. ZATTAR-RAMOS, L.C.1* LEÃO, R.V. 1 CAVALCANTI, C.F.A.1 BORDALO-RODRIGUES, M.1 1 LEITE, C.C. HOSPITAL SÍRIO-LIBANÊS, 1 São Paulo – SP, Brazil. CERRI, G.G. *[email protected] 1Department of Radiology ▶ DISCLOSURE PARAGRAPHS: - The authors of this educational review declare no relationships with any companies, whose products or services may be related to the subject matter of the article. - The authors state that this work has not received any funding. ▶ INTRODUCTION: - Sternal abnormalities are commonly seen in clinical practice. - In addition to the numerous anatomical variations and congenital anomalies, the sternum and sternoclavicular joints can be affected by various pathological conditions such as trauma, infection, tumors, degenerative and inflammatory changes. - This study aims to demonstrate and illustrate such conditions, as the knowledge of its characteristics and imaging findings are essential for correct diagnosis and patient management. ▶ DISCUSSION: - Sternum injuries are common and should be properly recognized and characterized; using different imaging methods we will illustrate the variations of normality, congenital abnormalities and characteristic radiographic findings of sternal lesions highlighting: psoriatic arthritis, inflammatory osteitis, SAPHO syndrome, neoplastic, traumatic and degenerative lesions. ▶ ANATOMY: STERNUM: Flat bone, with 3 parts: *MANUBRIUM: superior central (jugular) notch and 2 lateral fossae that articulate with the MANUBRIUM clavicles. Also articulates with the 1o and 2o ribs and the body of the sternum. - Atachments: sternohyoideus, sternothyroideus, subclavius, pectoralis major, transversus thoracis and sternocleidomastoideus muscles. BODY OF *BODY OF THE STERNUM: articulates with the THE manubrium, xiphoid process and with the 2o STERNUM through 7o ribs. -

Displacement of the Temporomandibular Joint Disk: Correlation Between Clinical Findings and MRI Characteristics
Applied RESEA R CH Displacement of the Temporomandibular Joint Disk: Correlation Between Clinical Findings and MRI Characteristics Contact Author Zeev V. Maizlin, MD; Nicoleta Nutiu, MD; Peter B. Dent, MD; Patrick M. Vos, MD; Dr. Maizlin David M. Fenton, MD; John M. Kirby, MBBCh; Parag Vora, MBBS; Email: [email protected] Jean H. Gillies, MD; Jason J. Clement, MD ABSTRACT Background and Objective: Disk displacement frequently causes dysfunction of the temporomandibular joint (TMJ). Magnetic resonance imaging (MRI) of the TMJ is 95% accurate in the assessment of disk position and form. Various restorative procedures are used for treatment of disk displacement. However, several authors have noted a lack of correlation between MRI findings of disk displacement and the extent of pain and dysfunction of the TMJ. The purpose of this study was to evaluate whether MRI findings of various degrees of disk displacement could be correlated with the presence of clinical signs and symptoms in patients with a clinical disorder of the TMJ. Materials and Methods: One hundred and forty-four TMJs (in 72 patients) were imaged. Displacement of the posterior band in relation to the condyle was quantified as mild or significant. Results: Disk displacement was found in 45 (54%) of the 84 symptomatic joints and 13 (22%) of the 60 asymptomatic joints. Among the 84 symptomatic joints, 31 (37%) had disk displacement with reduction and 14 (17%) had disk displacement without reduction. In the latter group, 11 (79%) of the 14 joints had significant displacement of the posterior band (8 or 9 o’clock) and 21% had mild displacement of the posterior band (10 o’clock). -

Dynamic Musculoskeletal Biomechanics in the Human Jaw
DYNAMIC MUSCULOSKELETAL BIOMECHANICS IN THE HUMAN JAW by CHRISTOPHER CHARLES PECK BDS, The University of Sydney, 1988 MSc(Dent), The University of Sydney, 1995 A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY in THE FACULTY OF GRADUATE STUDIES (Department of Oral Biology) We accept this thesis as confonning to the required standard 'THE UNIVERSITY OF BRITISH COLUMBIA NOVEMBER 1999 ® Christopher Charles Peck, 1999 In presenting this thesis in partial fulfilment of the requirements for an advanced degree at the University of British Columbia, I agree that the Library shall make it freely available for reference and study. I further agree that permission for extensive copying of this thesis for scholarly purposes may be granted by the head of my department or by his or her representatives. It is understood that copying or publication of this thesis for financial gain shall not be allowed without my written permission. Department of Q/-«J "fct'ftlo^ ( 0>oJ W^oJfL £cwu,o The University of British Columbia Vancouver, Canada Date 2°V .NW*—\ \^ DE-6 (2/88) ABSTRACT The high prevalence of functional disorders in the human jaw emphasises the need to understand better its dynamic behaviour. In the present studies, dynamic mathematical models based on typical physical properties of the human jaw and skeletal muscles have been developed. In the first three studies, a model of the entire jaw was created and utilised to predict jaw elasticity and viscosity, and to simulate muscle-driven symmetrical and asvmmetrical jaw movements. Specifically these models were constructed without "ligaments" (temporomandibular capsule or other accessory jaw ligaments) to determine whether or not plausible motion could be simulated in their absence. -

Dynamic Weight-Bearing Magnetic Resonance in the Clinical Diagnosis of Internal Temporomandibular Joint Disorders
634 Review Article Dynamic Weight-bearing Magnetic Resonance in the Clinical Diagnosis of Internal Temporomandibular Joint Disorders Silvana Giannini, MD1 Giorgio Chiogna, MD2 Rosario Francesco Balzano, MD3 Giuseppe Guglielmi, MD3 1 Department of Radiology, Casa di Cura Villa Stuart Sports Clinic, Address for correspondence Silvana Giannini, MD, Department of Università degli Studi di Roma “Foro Italico,” Rome, Italy Radiology, Casa di Cura Villa Stuart Sports Clinic, 00135 Rome, Italy 2 Department of Surgical and Dental Sciences, Fondazione Don Carlo (e-mail: [email protected]). Gnocchi, Rome, Italy 3 Department of Clinical and Experimental Medicine, University School of Medicine, Foggia, Italy Semin Musculoskelet Radiol 2019;23:634–642. Abstract Temporomandibular joint (TMJ) disorders can be painful and cause functional limi- tations and bone changes. Deeper clinical knowledge of the pathologies related to the TMJ has always been hindered by the difficult identification of the causes that limit its movement. Weight-bearing magnetic resonance imaging (WBMRI) can reproduce the articular movement in orthostasis and allows the evaluation of joint movement. Keywords WBMRI, compared with other procedures such as double-type condylography and ► temporomandibular real-time dynamic ultrasound, helps to better identify tissue characteristics of the joint articular glenoid-condylar surfaces, articular space, disk position on both the open and ► weight-bearing MRI closed mouth, and the locoregional musculotendinous area. WBMRI also identifies -

Modelling Suture Ossification: a View from the Cranial Capsule
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Masters Theses Graduate School 8-1992 Modelling Suture Ossification: A View from the Cranial Capsule Hugh Bryson Matternes University of Tennessee, Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_gradthes Part of the Anthropology Commons Recommended Citation Matternes, Hugh Bryson, "Modelling Suture Ossification: A View from the Cranial Capsule. " Master's Thesis, University of Tennessee, 1992. https://trace.tennessee.edu/utk_gradthes/4192 This Thesis is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Masters Theses by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a thesis written by Hugh Bryson Matternes entitled "Modelling Suture Ossification: A View from the Cranial Capsule." I have examined the final electronic copy of this thesis for form and content and recommend that it be accepted in partial fulfillment of the requirements for the degree of Master of Arts, with a major in Anthropology. Richard L. Jantz, Major Professor We have read this thesis and recommend its acceptance: Lyle W. Konigsberg, William M. Bass Accepted for the Council: Carolyn R. Hodges Vice Provost and Dean of the Graduate School (Original signatures are on file with official studentecor r ds.) To the Graduate Council: -

Cranial Sutures & Funny Shaped Heads: Radiological Diagnosis
Objectives • The objectives of this presentation are to: – Review the imaging features of normal cranial sutures – Identify the characteristics of abnormal skull shape on imaging – Review the characteristics of the most common non- syndromic and syndromic causes of craniosynostosis Anatomical Review Anatomical Review • The bony plates of the skull communicate at the cranial sutures • The anterior fontanelle occurs where the coronal & metopic sutures meet • The posterior fontanelle occurs where the sagittal & lambdoid sutures meet Anatomical Review • The main cranial sutures & fontanelles include: Metopic Suture Anterior Fontanelle Coronal Sutures Squamosal Sutures Posterior Fontanelle Sagittal Suture Lambdoid Sutures Anatomical Review • Growth of the skull occurs perpendicular to the cranial suture • This is controlled by a complex signalling system including: – Ephrins (mark the suture boundary) – Fibroblast growth factor receptors (FGFR) – Transcription factor TWIST Anatomical Review • The cranial sutures are important for rapid skull growth in-utero & infancy • The cranial sutures can usually be visualised on imaging into late adulthood Normal Radiological Appearances Normal Radiological Appearances • The cranial sutures can be visualised on plain radiographs • Standard views include: – PA – Lateral – Townes PA Skull radiograph Sagittal Suture Left Coronal Suture Right CoronalRight lambdoidSutureSuture Metopic Suture Left lambdoid Suture Townes View Sagittal Suture Left Coronal Suture Right Coronal Suture Right Lambdoid Suture Left -

A Heads up on Craniosynostosis
Volume 1, Issue 1 A HEADS UP ON CRANIOSYNOSTOSIS Andrew Reisner, M.D., William R. Boydston, M.D., Ph.D., Barun Brahma, M.D., Joshua Chern, M.D., Ph.D., David Wrubel, M.D. Craniosynostosis, an early closure of the growth plates of the skull, results in a skull deformity and may result in neurologic compromise. Craniosynostosis is surprisingly common, occurring in one in 2,100 children. It may occur as an isolated abnormality, as a part of a syndrome or secondary to a systemic disorder. Typically, premature closure of a suture results in a characteristic cranial deformity easily recognized by a trained observer. it is usually the misshapen head that brings the child to receive medical attention and mandates treatment. This issue of Neuro Update will present the diagnostic features of the common types of craniosynostosis to facilitate recognition by the primary care provider. The distinguishing features of other conditions commonly confused with craniosynostosis, such as plagiocephaly, benign subdural hygromas of infancy and microcephaly, will be discussed. Treatment options for craniosynostosis will be reserved for a later issue of Neuro Update. Types of Craniosynostosis Sagittal synostosis The sagittal suture runs from the anterior to the posterior fontanella (Figure 1). Like the other sutures, it allows the cranial bones to overlap during birth, facilitating delivery. Subsequently, this suture is the separation between the parietal bones, allowing lateral growth of the midportion of the skull. Early closure of the sagittal suture restricts lateral growth and creates a head that is narrow from ear to ear. However, a single suture synostosis causes deformity of the entire calvarium. -

The Distal Radioulnar Joint
90 Bulletin of the NYU Hospital for Joint Diseases 2009;67(1):90-6 The Distal Radioulnar Joint Peter C. Tsai, M.D., and Nader Paksima, D.O., M.P.H. Abstract gular fibrocartilage (TFC), the volar and dorsal radioulnar The distal radioulnar joint (DRUJ) acts in concert with the ligaments, the capsule, and the ulnar collateral ligament. proximal radioulnar joint to control forearm rotation. The DRUJ Extrinsic stability is achieved through static and dynamic is stabilized by the triangular fibrocartilage complex (TFCC). forces. The extensor carpi ulnaris (ECU) subsheath and the This complex of fibrocartilage and ligaments support the joint interosseous membrane (IOM) are assisted by the pronator through its arc of rotation, as well as provide a smooth surface quadratus, which actively compresses the ulnar head into for the ulnar side of the carpus. TFCC and DRUJ injuries are the sigmoid notch, and by the flexors and extensors of the part of the common pattern of injuries we see with distal radius forearm, which dynamically compress the DRUJ. fractures. While much attention has been paid to the treatment The bony and ligamentous restraints of the DRUJ en- of the distal radius fractures, many of the poor outcomes are able controlled pronation and supination.1 Though slightly due to untreated or unrecognized injuries to the DRUJ and its asymmetric to the ulnar head, the sigmoid notch has been components. shown to contribute approximately 20% of the stability of the DRUJ.2,3 The larger radius of curvature of the sigmoid he distal radioulnar joint (DRUJ) has been extensively notch results in a shallow concavity in comparison to the studied; however, much debate remains concern- convex ulnar head. -

The Sima De Los Huesos Crania: Analysis of the Cranial Breakage Patterns
Journal of Archaeological Science 72 (2016) 25e43 Contents lists available at ScienceDirect Journal of Archaeological Science journal homepage: http://www.elsevier.com/locate/jas The Sima de los Huesos Crania: Analysis of the cranial breakage patterns * Nohemi Sala a, b, c, , Ana Pantoja-Perez c, a, d, Juan Luis Arsuaga c, d, Adrian Pablos e, f, a, c, Ignacio Martínez a, c a Area de Antropología Física, Departamento de Ciencias de la Vida, Universidad de Alcala, Madrid, Spain € b Institut für Ur- und Frühgeschichte und Archaologie€ des Mittelalters Abteilung für Altere Urgeschichte und Quartar€ okologie,€ Eberhard-Karls Universitat€ Tübingen, Schloss Hohentübingen, 72070 Tübingen, Germany c Centro Mixto UCM-ISCIII de Evolucion y Comportamiento Humanos, Madrid, Spain d Departamento de Paleontología, Facultad Ciencias Geologicas, Universidad Complutense de Madrid, Spain e Centro Nacional de Investigacion sobre Evolucion Humana-CENIEH, Burgos, Spain f Paleoanthropology, Senckenberg Center for Human Evolution and Paleoenvironment, Eberhard Karls Universitat€ Tübingen, Germany article info abstract Article history: The Sima de los Huesos (SH) site has provided the largest collection of hominin crania in the fossil record, Received 29 March 2016 offering an unprecedented opportunity to perform a complete Forensic-Taphonomic study on a popu- Received in revised form lation from the Middle Pleistocene. The fractures found in seventeen crania from SH display a post- 1 June 2016 mortem fracturation pattern, which occurred in the dry bone stage and is compatible with collective Accepted 3 June 2016 burial assemblages. Nevertheless, in addition to the postmortem fractures, eight crania also display some Available online 14 June 2016 typical perimortem traumas. By using CT images we analyzed these fractures in detail. -
Chapter 7 Body Systems
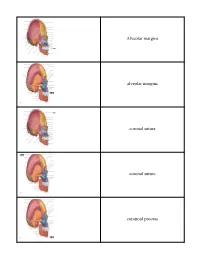
Identification and Palpation of Individual Joints of the Body 1 Joints of the Skull Cranial sutures 2 The four cranial sutures are the coronal suture, the sagittal suture, the squamous suture, and the lambdoidal suture. The coronal suture is located on the top of the skull above the eyebrows. The sagittal suture is midway between the top of the ear and the eye. The squamous suture arcs above the ear, and the lambdoidal suture is behind the ear, just above the mastoid process in an arc superiorly and posteriorly. Joints of the Skull Temporomandibular joint 4 The temporomandibular joint consists of the temporal bone and mandible and is a synovial modified hinge joint. The TMJ is one of the strongest joints in the body and is the only biarticular joint in the body. Joints of the Shoulder Glenohumeral joint 6 The glenohumeral joint is the main joint in the shoulder and the most mobile joint in the human body. The previous figure shows the ligaments of the shoulder. Joints of the Shoulder Sternoclavicular joint 8 The movements of the sternoclavicular joint follow the movements of the scapula and clavicle because no muscle works directly on this joint. A decrease or loss of mobility in this joint directly affects shoulder movement. This joint is the only direct connection between the axial skeleton and the shoulder girdle and arm. Joints of the Shoulder Acromioclavicular 10 Although a small joint, the acromioclavicular joint is important for shoulder movements. Some people do not have an acromioclavicular joint because the bones have fused. Joints of the Elbow Ulnohumeral and radiohumeral joints 12 These two joints allow flexion and extension. -
Crista Galli (Part of Cribriform Plate of Ethmoid Bone)
Alveolar margins alveolar margins coronal suture coronal suture coronoid process crista galli (part of cribriform plate of ethmoid bone) ethmoid bone ethmoid bone ethmoid bone external acoustic meatus external occipital crest external occipital protuberance external occipital protuberance frontal bone frontal bone frontal bone frontal sinus frontal squama of frontal bone frontonasal suture glabella incisive fossa inferior nasal concha inferior nuchal line inferior orbital fissure infraorbital foramen internal acoustic meatus lacrimal bone lacrimal bone lacrimal fossa lambdoid suture lambdoid suture lambdoid suture mandible mandible mandible mandibular angle mandibular condyle mandibular foramen mandibular notch mandibular ramus mastoid process of the temporal bone mastoid process of the temporal bone maxilla maxilla maxilla mental foramen mental foramen middle nasal concha of ethmoid bone nasal bone nasal bone nasal bone nasal bone occipital bone occipital bone occipital bone occipitomastoid suture occipitomastoid suture occipitomastoid suture occipital condyle optic canal optic canal palatine bone palatine process of maxilla parietal bone parietal bone parietal bone parietal bone perpendicular plate of ethmoid bone pterygoid process of sphenoid bone sagittal suture sella turcica of sphenoid bone Sphenoid bone (greater wing) spehnoid bone (greater wing) sphenoid bone (greater wing) sphenoid bone (greater wing) sphenoid sinus sphenoid sinus squamous suture squamous suture styloid process of temporal bone superior nuchal line superior orbital fissure supraorbital foramen (notch) supraorbital margin sutural bone temporal bone temporal bone temporal bone vomer bone vomer bone zygomatic bone zygomatic bone.