20.201 Mechanisms of Drug Action the Liver and Metabolism
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Liver • Gallbladder
NORMAL BODY Microscopic Anatomy! Accessory Glands of the GI Tract,! lecture 2! ! • Liver • Gallbladder John Klingensmith [email protected] Objectives! By the end of this lecture, students will be able to: ! • trace the flow of blood and bile within the liver • describe the structure of the liver in regard to its functions • indicate the major cell types of the liver and their functions • distinguish the microanatomy of exocrine and endocrine function by the hepatocytes • explain the functional organization of the gallbladder at the cellular level (Lecture plan: overview of structure and function, then increasing resolution of microanatomy and cellular function) Liver and Gallbladder Liver October is “Liver Awareness Month” -- http://www.liverfoundation.org Liver • Encapsulated by CT sheath and mesothelium • Lobes largely composed of hepatocytes in parenchyma • Receives blood from small intestine and general circulation Major functions of the liver • Production and secretion of digestive fluids to small intestine (exocrine) • Production of plasma proteins and lipoproteins (endocrine) • Storage and control of blood glucose • Detoxification of absorbed compounds • Source of embyronic hematopoiesis The liver lobule • Functional unit of the parenchyma • Delimited by CT septa, invisible in humans (pig is shown) • Surrounds the central vein • Bordered by portal tracts Central vein, muralia and sinusoids Parenchyma: Muralia and sinusoids • Hepatocyte basolateral membrane faces sinusoidal lumen • Bile canaliculi occur between adjacent hepatocytes • Cords anastomose Vascularization of the liver • Receives veinous blood from small intestine via portal vein • Receives freshly oxygenated blood from hepatic artery • Discharges blood into vena cava via hepatic vein Blood flow in the liver lobes • flows in via the portal vein and hepatic artery • oozes through the liver lobules to central veins • flows out via the hepatic vein Portal Tract! (aka portal triad) • Portal venule • Hepatic arteriole • Bile duct • Lymph vessel • Nerves • Connective tissue Central vein! (a.k.a. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -
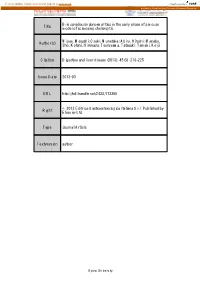
Title Bile Canalicular Abnormalities in the Early Phase of a Mouse
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Bile canalicular abnormalities in the early phase of a mouse Title model of sclerosing cholangitis. Miyao, Masashi; Ozeki, Munetaka; Abiru, Hitoshi; Manabe, Author(s) Sho; Kotani, Hirokazu; Tsuruyama, Tatsuaki; Tamaki, Keiji Citation Digestive and liver disease (2013), 45(3): 216-225 Issue Date 2013-03 URL http://hdl.handle.net/2433/173350 © 2012 Editrice Gastroenterologica Italiana S.r.l. Published by Right Elsevier Ltd. Type Journal Article Textversion author Kyoto University 1 Bile canalicular abnormalities in the early phase of a mouse model of sclerosing cholangitis Masashi Miyao1M.D.; Munetaka Ozeki1Ph.D.; Hitoshi Abiru1B.S.; Sho Manabe1B.S.; Hirokazu Kotani1M.D.; Tatsuaki Tsuruyama2 M.D. and Keiji Tamaki1 M.D. 1Department of Forensic Medicine and Molecular Pathology, Kyoto University Graduate School of Medicine 2Center for Anatomical Studies, Kyoto University Graduate School of Medicine Corresponding author: Keiji Tamaki. Telephone: +81 75 753 4474. Fax: +81 75 761 9591. E-mail: [email protected]. Department of Forensic Medicine and Molecular Pathology, Kyoto University Graduate School of Medicine, Yoshida-Konoe-cho, Sakyo-ku, Kyoto 606-8501, Japan Conflict of Interest: The authors declare no conflict of interest. Word count: 3484 words (excluding abstract, references, figures). 2 Abstract Background: The bile canaliculus is the smallest and first biliary channel and is formed by two or three adjacent hepatocytes. Previous studies of chronic cholangiopathies such as primary sclerosing cholangitis have focused on the bile ductules. However, little is known about the pathological alterations in bile canaliculi in the early phase of cholangiopathies. -

Motility of Bile Canaliculi in the Living Animal: Implications for Bile Flow Norihito Watanabe, Nobuhiro Tsukada, Charles R
Motility of Bile Canaliculi in the Living Animal: Implications for Bile Flow Norihito Watanabe, Nobuhiro Tsukada, Charles R. Smith, and M. James Phillips Research Institute and Departments of Pathology and Pediatrics, The Hospital for Sick Children and University of Toronto, Toronto, Ontario, Canada M5G 1X8 Abstract. Modem fluorescence microscopic techniques direction towards the portal bile ducts. Contractions were used to image the bile canalicular, system in the were not seen in the network of canaliculi on the sur- intact rat liver, in vivo. By combining the use of sodi- face of the liver. Cytochalasin B administration resulted um fluorescein secretion into bile, with digitally en- in reduced canalicular motility, progressive dilation of hanced fluorescence microscopy and time-lapse video, zone 1 canaliculi, and impairment of bile flow. Cana- it was possible to capture and record the canalicular licular dilations invariably involved the branch points motility events that accompany the secretion of bile in of the canalicular network. The findings add substan- life. Active bile canalicular contractions were found tively to previous in vitro studies using couplets, and predominantly in zone 1 (periportal) hepatocytes of suggest that canalicular contractions contribute physio- the liver. The contractile movements were repetitive, logically to bile flow in the liver. forceful, and appeared unidirectional moving bile in a TIN, myosin and associated proteins involved in con- tile collapses of canaliculi resulting from secretory pressure tractile movements have been found in smooth muscle with rupture of canaliculi (9, 11, 30, 35). In this report, we and nonmuscle cells (1, 16, 18, 24, 42, 43, 56, 61, have taken advantage of the biliary secretion of sodium 65). -

26 April 2010 TE Prepublication Page 1 Nomina Generalia General Terms
26 April 2010 TE PrePublication Page 1 Nomina generalia General terms E1.0.0.0.0.0.1 Modus reproductionis Reproductive mode E1.0.0.0.0.0.2 Reproductio sexualis Sexual reproduction E1.0.0.0.0.0.3 Viviparitas Viviparity E1.0.0.0.0.0.4 Heterogamia Heterogamy E1.0.0.0.0.0.5 Endogamia Endogamy E1.0.0.0.0.0.6 Sequentia reproductionis Reproductive sequence E1.0.0.0.0.0.7 Ovulatio Ovulation E1.0.0.0.0.0.8 Erectio Erection E1.0.0.0.0.0.9 Coitus Coitus; Sexual intercourse E1.0.0.0.0.0.10 Ejaculatio1 Ejaculation E1.0.0.0.0.0.11 Emissio Emission E1.0.0.0.0.0.12 Ejaculatio vera Ejaculation proper E1.0.0.0.0.0.13 Semen Semen; Ejaculate E1.0.0.0.0.0.14 Inseminatio Insemination E1.0.0.0.0.0.15 Fertilisatio Fertilization E1.0.0.0.0.0.16 Fecundatio Fecundation; Impregnation E1.0.0.0.0.0.17 Superfecundatio Superfecundation E1.0.0.0.0.0.18 Superimpregnatio Superimpregnation E1.0.0.0.0.0.19 Superfetatio Superfetation E1.0.0.0.0.0.20 Ontogenesis Ontogeny E1.0.0.0.0.0.21 Ontogenesis praenatalis Prenatal ontogeny E1.0.0.0.0.0.22 Tempus praenatale; Tempus gestationis Prenatal period; Gestation period E1.0.0.0.0.0.23 Vita praenatalis Prenatal life E1.0.0.0.0.0.24 Vita intrauterina Intra-uterine life E1.0.0.0.0.0.25 Embryogenesis2 Embryogenesis; Embryogeny E1.0.0.0.0.0.26 Fetogenesis3 Fetogenesis E1.0.0.0.0.0.27 Tempus natale Birth period E1.0.0.0.0.0.28 Ontogenesis postnatalis Postnatal ontogeny E1.0.0.0.0.0.29 Vita postnatalis Postnatal life E1.0.1.0.0.0.1 Mensurae embryonicae et fetales4 Embryonic and fetal measurements E1.0.1.0.0.0.2 Aetas a fecundatione5 Fertilization -
Digestive Glands
Digestive glands Department of Histology and Embryology of Jilin university ----Jiang Wenhua 1.general description of digestive glands Small digestive glands oesophageal glands gastric glands pyloric glands intestinal glands large digestive glands salivary glands pancreas liver Function: excretion digestive juice incretion 2 salivary glands 2.1.The General Structure of Salivary Glands being composed of acinus and duct striated ducts mucous acinus intercalated ducts serous acinus serous demilune Schematic drawing of the structure of Salivary Glands 2.1.1 acinus (1) serous acinus (2) mucous acinus (3) mixed acinus serous acinus • Serous cells are usually pyramidal in shape, with a broad base and a narrow apical surface .They exhibit characteristics of protein-secreting cells. Adjacent secretory cells are joined together and usually form a spherical mass of cells called acinus, with a lumen in the center . striated ducts mucous acinus intercalated ducts serous acinus serous demilune Schematic drawing of the structure of Salivary Glands mucous cells Mucous cells are usually cuboidal to columnar in shape; their nuclei are oval and pressed toward the bases of the cells. They exhibit the characteristics of mucus-secreting cells , containing glycoproteins important for the moistening and lubricating functions of the saliva. striated ducts mucous acinus intercalated ducts serous acinus serous demilune Schematic drawing of the structure of Salivary Glands The cytoplasm stains lighter in an H and E preparation.large mucigen granules are present -
The Biliary System, Second Edition the Biliary System
WAN G • ET AL G • ET WAN Colloquium Lectures on Series ISSN: 2154-560X Integrated Systems Physiology From Molecule to Function to Disease LIFE SCIENCES Series Editors: D. Neil Granger, LSU Health Sciences, Shreveport Joey Granger, University of Mississippi Medical Center The Biliary System, Second Edition The Biliary System David Q.-H. Wang, Saint Louis University, USA THE BILIAR Brent A. Neuschwander-Tetri, Saint Louis University, USA Piero Portincasa, Saint Louis University and University of Bari Medical School, Italy Second Edition The biliary system is a complex network of microscopic and macroscopic structures involved in the formation of bile, an aqueous fluid in which a considerable amount of otherwise immiscible cholesterol is transported by other Y SYSTEM Y lipids such as bile acids and phospholipids. This book summarizes current understanding of the molecular and cellular mechanisms of cholesterol and bile acid metabolism, as well as the physical-chemistry of biliary lipids, with an emphasis on biliary lipid metabolism that is regulated by nuclear receptors in the hepatobiliary system. By guiding readers through the various aspects of anatomy, physiology, and biochemistry of all “players” involved in bile formation, this book is intended to be a manageable, easy-to-study compendium of recent EDITION SECOND , progresses in understanding the molecular mechanisms of cholesterol and bile acid metabolism. The authors clearly explain the molecular and cellular pathways that regulate hepatic lipid metabolism, and present color figures, tables, and flowcharts that explain the fundamental mechanisms of lipid synthesis and secretion, bile formation, the enterohepatic circulation, and intestinal absorption of biliary components. Moreover, the consequences of the complex events involving lipid metabolism in the hepatobiliary system are reviewed, with a focus on the translational value of current basic research in health and disease. -

Nomina Histologica Veterinaria
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

Ahmad CHARANEK the Bile Canaliculus Revisited
ANNÉE 2015 THÈSE / UNIVERSITÉ DE RENNES 1 sous le sceau de l’Université Européenne de Bretagne pour le grade de DOCTEUR DE L’UNIVERSITÉ DE RENNES 1 Mention : Biologie et Sciences de la Santé École doctorale Vie-Agro-Santé présentée par Ahmad CHARANEK Préparée dans l’Unité de Recherche INSERM UMR 991 «Foie, Métabolismes et Cancer» (Pharmacie) Thèse soutenue à Rennes The Bile Canaliculus le 10 Juin 2015 devant le jury composé de : Revisited: Pr Chantal HOUSSET Professeur des Universités Morphological And Université de Paris 6 / rapporteur Pr Marc PALLARDY Functional Professeur des Universités Université de Paris 11 / rapporteur Alterations Induced Pr Pierre BRISSOT Professeur des Universités By Cholestatic Université de Rennes 1 / examinateur Dr Richard WEAVER Drugs In HepaRG Scientific Director INSTITUT DE RECHERCHES INTERNATIONALES SERVIER / examinateur Cells Dr Christiane GUGUEN-GUILLOUZO Directeur de Recherches Emérite Inserm Université de Rennes 1 / examinateur Pr André GUILLOUZO Professeur des Universités Université de Rennes 1 / directeur de thèse 1 The test of our progress is not whether we add more to the abundance of those who have much; it is whether we provide enough for those who have little. Franklin Delano Roosevelt 2 Acknowledgment Foremost, I would like to express my sincere gratitude to my supervisor Pr. André Guillouzo, for his constant guidance, continuous encouragement, and patience along the thesis preparation. I am grateful to the trust he gave me, and the moral support he provided. I highly appreciate his confidence in my ambitious goals, and his enormous efforts to provide me with all the required facilities. I am so thankful for his priceless advices that will pave the road for my future career. -

Bile Canaliculi Can Be Seen Between the Hepatocytes
DIGESTIVE GLANDS II Mr. Babatunde D.E Liver ❖ Is the second largest organ in the body. ❖ Is composed of a single type of parenchymal cell, the hepatocyte. Hepatocyte ❖ Possess a myriad of both endocrine and exocrine functions. Figure 16—18. Ultrastructure of a hepatocyte. RER, rough endoplasmic reticulum; SER, smooth endoplasmic reticulum. x10,000. Glisson’s Capsule ❖ Is composed of thin connective tissue that subdivides the liver into lobes and lobules. Blood Supply ❖ Of the liver is derived from two sources: abdominal aorta, via the hepatic artery; portal vein, which brings nutrient-laden blood from the alimentary tract and the spleen. Porta Hepatis ❖ Is the region where the hepatic artery and the portal vein enter and the hepatic ducts leave the liver. Drainage ❖ Of blood is via the hepatic vein. ❖ Hepatic vein is formed by the union of numerous sublobular veins. ❖ Sublobular veins collect blood from the central vein of each classical liver lobule. Bile ❖ Leaves the liver via the hepatic ducts. ❖ Is delivered to the gallbladder. Liver Lobules ❖ There are three types of liver lobules: classical (hexagonal in histologic section); portal lobule (triangular in histological section); liver acinus of Rappaport (liver acinus; diamond shaped in histologic section). CENTRAL VEIN PORTAL CANAL Classical Lobule ❖ Is based on the pig’s liver, where connective tissue elements clearly delineate it. ❖ Portal area (portal canal; triad) is present at each corner of the lobule. ❖ Portal area contains branches of the portal vein, hepatic artery, bile duct, and lymph vessel. Figure 16—12. Three- dimensional aspect of the normal liver. In the upper center is the central vein; in the lower center, the portal vein. -

Expression and Compartmentalization of Integral Plasma Membrane Proteins by Hepatocytes and Their Progenitors in the Rat Pancreas
Expression and compartmentalization of integral plasma membrane proteins by hepatocytes and their progenitors in the rat pancreas JAMES R. BARTLES1'*, M. SAMBASIVA RAO2, LIQIN ZHANG1, BARBARA E. FAYOS1, CHERYL L. NEHME1 and JANARDAN K. REDDY2 Departments oflCell, Molecular and Structural Biology and 2Pathology, Northwestern University Medical School, 303 East Chicago Avenue, Chicago, Illinois 60611, USA * Author for correspondence Summary A combination of Western blotting, Northern blotting analogy to their respective localizations on hepato- and immunofluorescence was used to examine the cytes in liver, rat hepatic lectin-1 was concentrated expression and compartmentalization of plasma on those surfaces exposed to the pancreatic matrix at membrane proteins by those hepatocyte-like cells the periphery of the hepatocyte clusters (the basal that arise in the pancreases of rats subjected to surface equivalent), whereas HA 321 was concen- sequential dietary copper depletion and repletion. trated on those surfaces exposed to adjacent hepato- The pancreatic hepatocytes were found to: (1) ex- cytes within the clusters. The hepatocyte plasma press several integral membrane proteins known to membrane proteins were found to be expressed in be concentrated within the apical, lateral or basolat- the pancreas at different times during the copper eral domains of the plasma membranes of hepato- depletion/repletion protocol: for example, rat hep- cytes in liver; and (2) compartmentalize the mem- atic lectin-1 and the bulk of the HA 4 were expressed brane proteins to equivalent plasma membrane relatively late in the protocol, only after large domains, despite the organization of these cells into numbers of pancreatic hepatocytes had appeared; clusters instead of highly vascularized plates.