Liver • Gallbladder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Inhibitory Smads Suppress Pancreatic Stellate Cell Activation Through Negative Feedback in Chronic Pancreatitis
384 Original Article Page 1 of 10 Inhibitory Smads suppress pancreatic stellate cell activation through negative feedback in chronic pancreatitis Hao Lin1,2#^, Beibei Dong3#, Liang Qi3, Yingxiang Wei4, Yusha Zhang5, Xiaotian Cai5, Qi Zhang5, Jia Li4, Ling Li2,3 1Department of Clinical Science and Research, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, China; 2Institute of Pancreas, Southeast University, Nanjing, China; 3Department of Endocrinology, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, China; 4Department of Ultrasound, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, China; 5School of Medicine, Southeast University, Nanjing, China Contributions: (I) Conception and design: H Lin, L Li; (II) Administrative support: H Lin, Y Zhang, X Cai, Q Zhang, J Li; (III) Provision of study materials or patients: H Lin, B Dong; (IV) Collection and assembly of data: H Lin, B Dong, L Qi, Y Wei; (V) Data analysis and interpretation: H Lin, B Dong; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. #These authors contributed equally to this work. Correspondence to: Hao Lin. Department of Clinical Science and Research, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, China. Email: [email protected]; Ling Li. Department of Endocrinology, Zhongda Hospital, School of Medicine, Southeast University, Nanjing 210009, China. Email: [email protected]. Background: Activation of pancreatic stellate cells (PSCs) is a key cause of chronic pancreatitis (CP), while inhibition of transforming growth factor-β (TGF-β) signaling renders PSCs inactive. Inhibitory Smads (I-Smads) impede TGF-β intracellular signaling and may provide a way to alleviate CP. Thus, we aimed to investigate the molecular mechanism of I-Smads in CP animals and freshly-isolated PSCs. -

Loss of Glp2r Signaling Activates Hepatic Stellate Cells and Exacerbates Diet-Induced Steatohepatitis in Mice
Loss of Glp2r signaling activates hepatic stellate cells and exacerbates diet-induced steatohepatitis in mice Shai Fuchs, … , Dianne Matthews, Daniel J. Drucker JCI Insight. 2020;5(8):e136907. https://doi.org/10.1172/jci.insight.136907. Research Article Endocrinology Metabolism Graphical abstract Find the latest version: https://jci.me/136907/pdf RESEARCH ARTICLE Loss of Glp2r signaling activates hepatic stellate cells and exacerbates diet-induced steatohepatitis in mice Shai Fuchs,1,2 Bernardo Yusta,1 Laurie L. Baggio,1 Elodie M. Varin,1 Dianne Matthews,1 and Daniel J. Drucker1,3 1Lunenfeld Tanenbaum Research Institute, Mount Sinai Hospital, Toronto, Ontario, Canada. 2The Hospital for Sick Children and 3Department of Medicine, University of Toronto, Toronto, Ontario, Canada. A glucagon-like peptide-2 (GLP-2) analog is used in individuals with intestinal failure who are at risk for liver disease, yet the hepatic actions of GLP-2 are not understood. Treatment of high- fat diet–fed (HFD-fed) mice with GLP-2 did not modify the development of hepatosteatosis or hepatic inflammation. In contrast, Glp2r–/– mice exhibited increased hepatic lipid accumulation, deterioration in glucose tolerance, and upregulation of biomarkers of hepatic inflammation. Both mouse and human liver expressed the canonical GLP-2 receptor (GLP-2R), and hepatic Glp2r expression was upregulated in mice with hepatosteatosis. Cell fractionation localized the Glp2r to hepatic stellate cells (HSCs), and markers of HSC activation and fibrosis were increased in livers of Glp2r–/– mice. Moreover, GLP-2 directly modulated gene expression in isolated HSCs ex vivo. Taken together, these findings define an essential role for the GLP-2R in hepatic adaptation to nutrient excess and unveil a gut hormone-HSC axis, linking GLP-2R signaling to control of HSC activation. -

Human Hepatic Stellate Cell Line (LX-2) Exhibits Characteristics of Bone Marrow-Derived Mesenchymal Stem Cells
Experimental and Molecular Pathology 91 (2011) 664–672 Contents lists available at SciVerse ScienceDirect Experimental and Molecular Pathology journal homepage: www.elsevier.com/locate/yexmp Human hepatic stellate cell line (LX-2) exhibits characteristics of bone marrow-derived mesenchymal stem cells Andrielle Castilho-Fernandes a,b,⁎, Danilo Candido de Almeida a,b, Aparecida Maria Fontes a,b, Fernanda Ursoli Ferreira Melo b, Virgínia Picanço-Castro b, Marcela Cristina Freitas a,b, Maristela D. Orellana a,b, Patricia V.B. Palma b, Perry B. Hackett c, Scott L. Friedman d, Dimas Tadeu Covas a,b a Faculty of Medicine of Ribeirão Preto, Department of Clinical Medicine, University of São Paulo, Av. Bandeirantes, 3900 (6° andar do HC) Ribeirão Preto 14048-900, Brazil b Center for Cell Therapy and Regional Blood Center of Ribeirão Preto, National Institute of Science and Technology in Stem Cell and Cell Therapy, Rua Tenente Catão Roxo, 2501, Ribeirão Preto 14051-140, Brazil c Department of Genetics, Cell Biology, and Development, University of Minnesota, 6-160 Jackson Hall, 321 Church St. SE, Minneapolis 55455, USA d Mount Sinai School of Medicine, Icahn Medical Institute, 11th Floor, Room 11-70C, 1425 Madison Avenue, NY 10029, USA article info abstract Article history: The LX-2 cell line has characteristics of hepatic stellate cells (HSCs), which are considered pericytes of the hepatic Received 15 March 2011 microcirculatory system. Recent studies have suggested that HSCs might have mesenchymal origin. We have and in revised form 2 September 2011 performed an extensive characterization of the LX-2 cells and have compared their features with those of mes- Available online 9 September 2011 enchymal cells. -

Isolation of Small Polarized Bile Duct Units A
Proc. Natl. Acad. Sci. USA Vol. 92, pp. 6527-6531, July 1995 Physiology Isolation of small polarized bile duct units A. MENNONE*, D. ALVAROt, W. CHO*, AND J. L. BOYER*t *Department of Medicine and Liver Center, Yale University School of Medicine, P.O. Box 208019, 333 Cedar Street, New Haven, CT (06520-8019; and tViale Dell'Universita' 37, 00185 Rome, Italy Communicated by Edward Adelberg, New Haven, CT, February 27, 1995 ABSTRACT Fragments of small interlobular bile ducts BB salt, forskolin, dideoxyforskolin, and N6,2'-O-dibutyryl- averaging 20 ,um in diameter can be isolated from rat liver. adenosine 3' :5 '-cyclic monophosphate (dibutyryl cAMP; These isolated bile duct units form luminal spaces that are Bt2cAMP) were purchased from Sigma. 2,7-Bis(carboxy- impermeant to dextran-40 and expand in size when cultured methyl)-5-(and-6)-carboxyfluorescein, acetomethyl ester in 10 ,uM forskolin for 24-48 hr. Secretion is Cl- and HCO3 (BCECF-AM), and H2DIDS were obtained from Molecular dependent and is stimulated by forskolin > dibutyryl cAMP Probes. Matrigel was from Collaborative Research, collage- > secretin but not by dideoxyforskolin, as assessed by video nase D was from Boehringer Mannheim Biochemicals, and imaging techniques. Secretin stimulates Cl-/HCOi exchange Pronase was from Calbiochem. Liebowitz-15 (L-15), minimum activity, and intraluminal pH increases after forskolin ad- essential medium (MEM), a-MEM, L-glutamine, gentamicin, ministration. These studies establish that small polarized and fetal calf serum were from GIBCO. N-(,y-1-Glutamyl)-4- physiologically intact interlobular bile ducts can be isolated methoxy-2-naphthylamide was obtained from Polyscience. -

Regulation of Liver Fibrosis Via Alteration of Hepatic
REGULATION OF LIVER FIBROSIS VIA ALTERATION OF HEPATIC STELLATE CELL ACTIVATION DURING LIVER REPAIR A Dissertation by KELLY MARIE MCDANIEL Submitted to the Office of Graduate and Professional Studies of Texas A&M University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY Chair of Committee, Gianfranco Alpini Committee Members, Fanyin Meng Shannon Glaser Cynthia Meininger Head of Program, Warren Zimmer August 2017 Major Subject: Medical Sciences Copyright 2017. Kelly Marie McDaniel ABSTRACT Cholestatic liver diseases including primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC) and alcoholic-induced hepatobiliary damage are growing problems in the United States as well as worldwide. There are no successful treatments for these diseases that ultimately develop into cirrhosis and end stage liver diseases with no treatment but liver transplantation. We used the cholestatic bile-duct ligated (BDL) mouse liver to examine treatment with small or large cholangiocytes, a mouse model that mimics some features of PSC to study treatment with stem cell-derived extracellular vesicles and a mouse model of alcoholic liver disease to show the important role of let-7. After treatment, liver tissues/cells were analyzed for fibrosis, inflammation, endodermal markers and hepatic stellate cell activation. Mechanisms of action were evaluated further in vitro through the use of hepatic cell lines. We showed that small cholangiocyte treatment reduced fibrosis, biliary mass and stellate cell activation through enhanced expression of FoxA2. We additionally showed that treatment of cultured human stellate cell lines with cholangiocyte supernatants from small cholangiocyte- treated BDL mice showed increased senescence and decreased fibrosis and inflammation. -

Recently Discovered Interstitial Cell Population of Telocytes: Distinguishing Facts from Fiction Regarding Their Role in The
medicina Review Recently Discovered Interstitial Cell Population of Telocytes: Distinguishing Facts from Fiction Regarding Their Role in the Pathogenesis of Diverse Diseases Called “Telocytopathies” Ivan Varga 1,*, Štefan Polák 1,Ján Kyseloviˇc 2, David Kachlík 3 , L’ubošDanišoviˇc 4 and Martin Klein 1 1 Institute of Histology and Embryology, Faculty of Medicine, Comenius University in Bratislava, 813 72 Bratislava, Slovakia; [email protected] (Š.P.); [email protected] (M.K.) 2 Fifth Department of Internal Medicine, Faculty of Medicine, Comenius University in Bratislava, 813 72 Bratislava, Slovakia; [email protected] 3 Institute of Anatomy, Second Faculty of Medicine, Charles University, 128 00 Prague, Czech Republic; [email protected] 4 Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava, 813 72 Bratislava, Slovakia; [email protected] * Correspondence: [email protected]; Tel.: +421-90119-547 Received: 4 December 2018; Accepted: 11 February 2019; Published: 18 February 2019 Abstract: In recent years, the interstitial cells telocytes, formerly known as interstitial Cajal-like cells, have been described in almost all organs of the human body. Although telocytes were previously thought to be localized predominantly in the organs of the digestive system, as of 2018 they have also been described in the lymphoid tissue, skin, respiratory system, urinary system, meninges and the organs of the male and female genital tracts. Since the time of eminent German pathologist Rudolf Virchow, we have known that many pathological processes originate directly from cellular changes. Even though telocytes are not widely accepted by all scientists as an individual and morphologically and functionally distinct cell population, several articles regarding telocytes have already been published in such prestigious journals as Nature and Annals of the New York Academy of Sciences. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

Arteriohepatic Dysplasia
ANNALS OF CLINICAL AND LABORATORY SCIENCE, Vol. 14, No. 6 Copyright © 1984, Institute for Clinical Science, Inc. Arteriohepatic Dysplasia (Alagille’s Syndrome): A Common Cause of ConJugated Hyperbilirubinemia ELLEN KAHN, M.D.* and FREDRIC DAUM, M.D.f *Department of Laboratories and Department of Pediatrics, f Division of Pediatric Gastroenterology, Department of Pediatrics, North Shore University Hospital, Manhasset, NY 11030 Cornell University Medical College, New York, NY 10021 ABSTRACT Syndromatic paucity of interlobular bile ducts is a common cause of conjugated hyperbilirubinemia in children. The clinical presentation is not always obvious. Therefore, the liver biopsy may be a useful diagnostic tool in the definition of this entity. The hepatic and biliary morphology of five children with arteriohepatic dysplasia (Alagille’s syndrome) is described. Prior to diagnosis, four un derwent Kasai procedures after intraoperative cholangiograms failed to demonstrate patency of the extrahepatic bile ducts. In three patients, a focal proximal hypoplasia of the common hepatic duct was demonstrated. Hypoplasia of the gallbladder occurred in two patients. Hepatic features of seQuential liver biopsies obtained in the five patient^ were divided into early and late changes. From birth to four months of age, the pathology consisted of cholestasis and bile duct destruction. After four months of age, there was persistent cholestasis, paucity of interlobular bile ducts and portal fibrosis. The etiology of arteriohepatic dysplasia is unclear. The main pathoge nic mechanisms are discussed. It is felt that the syndromatic duct paucity represents an acquired primary ductal defect resulting from a genetically determined immune response to as yet undefined agent or agents. Introduction and may not be obvious in the newborn. -

University of Southampton Research Repository Eprints Soton
University of Southampton Research Repository ePrints Soton Copyright © and Moral Rights for this thesis are retained by the author and/or other copyright owners. A copy can be downloaded for personal non-commercial research or study, without prior permission or charge. This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the copyright holder/s. The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the copyright holders. When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given e.g. AUTHOR (year of submission) "Full thesis title", University of Southampton, name of the University School or Department, PhD Thesis, pagination http://eprints.soton.ac.uk University of Southampton Faculty of Medicine, Health and Biological Sciences Pancreatic Research Group An investigation into soluble growth factors of TIMP-1, IGF-1 and Insulin on Pancreatic stellate cell survival Dr Manish Patel DM Thesis February 2014 University of Southampton An investigation into soluble growth factors of TIMP-1, IGF-1 and Insulin on Pancreatic stellate cell survival Faculty of Medicine, Health and Biological Sciences During pancreatic injury, the pancreatic stellate cell(PSC) become activated to a myofibroblast-like phenotype, proliferate and are known to be the major source of matrix which characterise pancreatic fibrosis in chronic pancreatitis and pancreatic cancer. Activated PSC also express matrix degrading metalloproteinases(MMPs) and their tissue inhibitors(TIMPs). Previous work has demonstrated that during spontaneous recovery from experimental liver fibrosis after 4 weeks of carbon tetrachloride injections, there is a fall in the expression of TIMP-1, a loss of the hepatic stellate cells (HSCs) by apoptosis, and an increase in liver collagenolytic activity with the return of the liver to a near normal histology. -
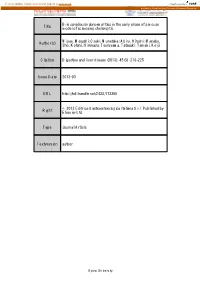
Title Bile Canalicular Abnormalities in the Early Phase of a Mouse
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Bile canalicular abnormalities in the early phase of a mouse Title model of sclerosing cholangitis. Miyao, Masashi; Ozeki, Munetaka; Abiru, Hitoshi; Manabe, Author(s) Sho; Kotani, Hirokazu; Tsuruyama, Tatsuaki; Tamaki, Keiji Citation Digestive and liver disease (2013), 45(3): 216-225 Issue Date 2013-03 URL http://hdl.handle.net/2433/173350 © 2012 Editrice Gastroenterologica Italiana S.r.l. Published by Right Elsevier Ltd. Type Journal Article Textversion author Kyoto University 1 Bile canalicular abnormalities in the early phase of a mouse model of sclerosing cholangitis Masashi Miyao1M.D.; Munetaka Ozeki1Ph.D.; Hitoshi Abiru1B.S.; Sho Manabe1B.S.; Hirokazu Kotani1M.D.; Tatsuaki Tsuruyama2 M.D. and Keiji Tamaki1 M.D. 1Department of Forensic Medicine and Molecular Pathology, Kyoto University Graduate School of Medicine 2Center for Anatomical Studies, Kyoto University Graduate School of Medicine Corresponding author: Keiji Tamaki. Telephone: +81 75 753 4474. Fax: +81 75 761 9591. E-mail: [email protected]. Department of Forensic Medicine and Molecular Pathology, Kyoto University Graduate School of Medicine, Yoshida-Konoe-cho, Sakyo-ku, Kyoto 606-8501, Japan Conflict of Interest: The authors declare no conflict of interest. Word count: 3484 words (excluding abstract, references, figures). 2 Abstract Background: The bile canaliculus is the smallest and first biliary channel and is formed by two or three adjacent hepatocytes. Previous studies of chronic cholangiopathies such as primary sclerosing cholangitis have focused on the bile ductules. However, little is known about the pathological alterations in bile canaliculi in the early phase of cholangiopathies. -

LA COLESTASI Diagnosi E Terapia Basata Sull’Evidenza Linee Guida
LA COLESTASI Diagnosi e terapia basata sull’evidenza Linee guida a cura della Commissione “Colestasi” dell’Associazione Italiana per lo Studio del Fegato Redatto da: Mario Angelico (coordinatore), Domenico Alvaro, Cristiana Barbera, Antonio Benedetti, Maria Antonia Bianco, Livio Cipolletta, Michele Colledan, Carla Colombo, Guido Costamagna, Davide Festi, Annarosa Floreani, Giovanni Galatola, Bruno Gridelli, Pietro Invernizzi, Paola Loria, Giuseppe Mazzella, Layos Okolicsanyi, Antonio Orlacchio, Floriano Rosina, Aurelio Sonzogni, Mario Strazzabosco. DOCUMENTI ELABORATI DALLE COMMISSIONI SCIENTIFICHE (RACCOLTA 1996-2001) Abbreviazioni usate nel testo: AMA: anticorpi anti-mitocondrio ANA: anticorpi anti-nucleo ASMA: anticorpi anti-muscolo liscio ANCA: anticorpi anti-citoplasma dei neutrofili AVB: atresia delle vie biliari OLT: trapianto di fegato (orthotopic liver transplantation) MRS: Mayo Risk Score (per CBP) CBP: cirrosi biliare primitiva CSP: colangite sclerosante primitiva CPRE: colangio-pancreatografia retrograda per-endoscopica CPRM: colangio-pancreatografia a risonanza magnetica CPT: colangiografia transepatica percutanea EUS: endosonografia US: ultrasonografia (ecografia) VBP: via biliare principale PPV: valore predittivo positivo NPV: valore predittivo negativo UDCA: acido ursodesossicolico TC: tomografia computerizzata SE: sfinterotomia endoscopica DCVB: dilatazioni congenite delle vie biliari CSA: colangite sclerosante autoimmune DNB: drenaggi nasobiliari PTDB drenaggi biliari dopo trapianto al fegato RCT: randomized controlled