The Liver, Pancreas, and Gallbladder*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Heart Vein Artery
1 PRE-LAB EXERCISES Open the Atlas app. From the Views menu, go to System Views and scroll down to Circulatory System Views. You are responsible for the identification of all bold terms. A. Circulatory System Overview In the Circulatory System Views section, select View 1. Circulatory System. The skeletal system is included in this view. Note that blood vessels travel throughout the entire body. Heart Artery Vein 2 Brachiocephalic trunk Pulmonary circulation Pericardium 1. Where would you find the blood vessels with the largest diameter? 2. Select a few vessels in the leg and read their names. The large blue-colored vessels are _______________________________ and the large red-colored vessels are_______________________________. 3. In the system tray on the left side of the screen, deselect the skeletal system icon to remove the skeletal system structures from the view. The largest arteries and veins are all connected to the _______________________________. 4. Select the heart to highlight the pericardium. Use the Hide button in the content box to hide the pericardium from the view and observe the heart muscle and the vasculature of the heart. 3 a. What is the largest artery that supplies the heart? b. What are the two large, blue-colored veins that enter the right side of the heart? c. What is the large, red-colored artery that exits from the top of the heart? 5. Select any of the purple-colored branching vessels inside the rib cage and use the arrow in the content box to find and choose Pulmonary circulation from the hierarchy list. This will highlight the circulatory route that takes deoxygenated blood to the lungs and returns oxygenated blood back to the heart. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Vessels and Circulation
CARDIOVASCULAR SYSTEM OUTLINE 23.1 Anatomy of Blood Vessels 684 23.1a Blood Vessel Tunics 684 23.1b Arteries 685 23.1c Capillaries 688 23 23.1d Veins 689 23.2 Blood Pressure 691 23.3 Systemic Circulation 692 Vessels and 23.3a General Arterial Flow Out of the Heart 693 23.3b General Venous Return to the Heart 693 23.3c Blood Flow Through the Head and Neck 693 23.3d Blood Flow Through the Thoracic and Abdominal Walls 697 23.3e Blood Flow Through the Thoracic Organs 700 Circulation 23.3f Blood Flow Through the Gastrointestinal Tract 701 23.3g Blood Flow Through the Posterior Abdominal Organs, Pelvis, and Perineum 705 23.3h Blood Flow Through the Upper Limb 705 23.3i Blood Flow Through the Lower Limb 709 23.4 Pulmonary Circulation 712 23.5 Review of Heart, Systemic, and Pulmonary Circulation 714 23.6 Aging and the Cardiovascular System 715 23.7 Blood Vessel Development 716 23.7a Artery Development 716 23.7b Vein Development 717 23.7c Comparison of Fetal and Postnatal Circulation 718 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch23_683-723.indd 683 2/14/11 4:31 PM 684 Chapter Twenty-Three Vessels and Circulation lood vessels are analogous to highways—they are an efficient larger as they merge and come closer to the heart. The site where B mode of transport for oxygen, carbon dioxide, nutrients, hor- two or more arteries (or two or more veins) converge to supply the mones, and waste products to and from body tissues. The heart is same body region is called an anastomosis (ă-nas ′tō -mō′ sis; pl., the mechanical pump that propels the blood through the vessels. -

Liver • Gallbladder
NORMAL BODY Microscopic Anatomy! Accessory Glands of the GI Tract,! lecture 2! ! • Liver • Gallbladder John Klingensmith [email protected] Objectives! By the end of this lecture, students will be able to: ! • trace the flow of blood and bile within the liver • describe the structure of the liver in regard to its functions • indicate the major cell types of the liver and their functions • distinguish the microanatomy of exocrine and endocrine function by the hepatocytes • explain the functional organization of the gallbladder at the cellular level (Lecture plan: overview of structure and function, then increasing resolution of microanatomy and cellular function) Liver and Gallbladder Liver October is “Liver Awareness Month” -- http://www.liverfoundation.org Liver • Encapsulated by CT sheath and mesothelium • Lobes largely composed of hepatocytes in parenchyma • Receives blood from small intestine and general circulation Major functions of the liver • Production and secretion of digestive fluids to small intestine (exocrine) • Production of plasma proteins and lipoproteins (endocrine) • Storage and control of blood glucose • Detoxification of absorbed compounds • Source of embyronic hematopoiesis The liver lobule • Functional unit of the parenchyma • Delimited by CT septa, invisible in humans (pig is shown) • Surrounds the central vein • Bordered by portal tracts Central vein, muralia and sinusoids Parenchyma: Muralia and sinusoids • Hepatocyte basolateral membrane faces sinusoidal lumen • Bile canaliculi occur between adjacent hepatocytes • Cords anastomose Vascularization of the liver • Receives veinous blood from small intestine via portal vein • Receives freshly oxygenated blood from hepatic artery • Discharges blood into vena cava via hepatic vein Blood flow in the liver lobes • flows in via the portal vein and hepatic artery • oozes through the liver lobules to central veins • flows out via the hepatic vein Portal Tract! (aka portal triad) • Portal venule • Hepatic arteriole • Bile duct • Lymph vessel • Nerves • Connective tissue Central vein! (a.k.a. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -
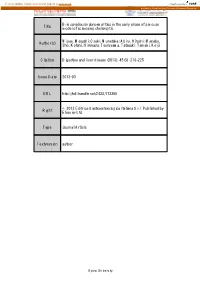
Title Bile Canalicular Abnormalities in the Early Phase of a Mouse
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Bile canalicular abnormalities in the early phase of a mouse Title model of sclerosing cholangitis. Miyao, Masashi; Ozeki, Munetaka; Abiru, Hitoshi; Manabe, Author(s) Sho; Kotani, Hirokazu; Tsuruyama, Tatsuaki; Tamaki, Keiji Citation Digestive and liver disease (2013), 45(3): 216-225 Issue Date 2013-03 URL http://hdl.handle.net/2433/173350 © 2012 Editrice Gastroenterologica Italiana S.r.l. Published by Right Elsevier Ltd. Type Journal Article Textversion author Kyoto University 1 Bile canalicular abnormalities in the early phase of a mouse model of sclerosing cholangitis Masashi Miyao1M.D.; Munetaka Ozeki1Ph.D.; Hitoshi Abiru1B.S.; Sho Manabe1B.S.; Hirokazu Kotani1M.D.; Tatsuaki Tsuruyama2 M.D. and Keiji Tamaki1 M.D. 1Department of Forensic Medicine and Molecular Pathology, Kyoto University Graduate School of Medicine 2Center for Anatomical Studies, Kyoto University Graduate School of Medicine Corresponding author: Keiji Tamaki. Telephone: +81 75 753 4474. Fax: +81 75 761 9591. E-mail: [email protected]. Department of Forensic Medicine and Molecular Pathology, Kyoto University Graduate School of Medicine, Yoshida-Konoe-cho, Sakyo-ku, Kyoto 606-8501, Japan Conflict of Interest: The authors declare no conflict of interest. Word count: 3484 words (excluding abstract, references, figures). 2 Abstract Background: The bile canaliculus is the smallest and first biliary channel and is formed by two or three adjacent hepatocytes. Previous studies of chronic cholangiopathies such as primary sclerosing cholangitis have focused on the bile ductules. However, little is known about the pathological alterations in bile canaliculi in the early phase of cholangiopathies. -

Review Article
JOURNAL OF PHYSIOLOGY AND PHARMACOLOGY 2008, 59, Suppl 2, 231238 www.jpp.krakow.pl Review article H. CICHO¯-LACH, K. CELIÑSKI, M. S£OMKA, B. KASZTELAN-SZCZERBIÑSKA PATHOPHYSIOLOGY OF PORTAL HYPERTENSION Department of Gastroenterology Medical University of Lublin, Poland In last years significant progress in recognizing mechanisms of portal hypertension pathophysiology was done. However, some unclear topics in this disease still exist. Portal hypertension is primarily caused by the increase in resistance to portal outflow and secondly by an increase in splanchnic blood flow. Portal hypertension is associated with changes in the intrahepatic, systemic, and portosystemic collateral circulation. Alterations in vasoreactivity (vasodilation and vasoconstriction) play a central role in the pathophysiology of portal hypertension by contributing to increased intrahepatic resistance, hyperdynamic circulation, and expansion of the collateral circulation. Among vasoactive substances which are activated in portal hypertension nitric oxide (NO) is considered as the most important vasodilator. Endothelin-1 and cyclooxygenase-derived prostaglandins are the main vasoconstrictor factors. The imbalance between the hyperresponsiveness and overproduction of vasoconstrictors and the hyporesponsiveness and impaired production of vasodilators are the mechanisms responsible of the increased vascular tone in the sinusoidal area of the liver. New concepts in the pathophysiology of portal hypertension find the significant role of hepatic stellate cells activated by endothelial factors which cause vascular remodeling as an adaptive response of the portal vessels wall. The most frequent causes of portal hypertension include portal vein thrombosis, storage diseases of the liver, hepatic cirrhosis (independent of etiology), hepatic veins thrombosis and schistosomiasis. Understanding the pathophysiology of portal hypertension could be of great utility in preventing and curing the complications of portal hypertension, such as esophageal varices, hepatic encephalopathy, ascites. -

20.201 Mechanisms of Drug Action the Liver and Metabolism
3/20/2007 Page 1 20.201 Mechanisms of Drug Action The Liver and Metabolism September 30, 2005 3/20/2007 Page 2 Distribution of Chemicals to Liver • Chemicals entering blood are distributed in the general circulation via the aorta • Chemicals enter various organs • Focus now on liver Epiglottis Mouth Grinds food and mixes it Flap that closes with saliva; where digestion windpipe during begins. • Liver anatomy swallowing. Salivary Glands ~ Largest organ and gland (1.5 kg) Trachea Make saliva, Windpipe (not part of start digestion of starch. ~ Structure: lobes (2 large - R and L; 2 small digestive system) Esophagus - caudate, quadrate) Hepatic Vein* Passes food from mouth to Vein that carries blood stomach by a process known ~ Blood supply: portal blood flow, 80%; away from liver. as peristalsis (contractions by walls of digestive tract that hepatic artery, 20%; outflow into vena cava Liver* move food forward). Stores food and makes ~ Bile duct/gall bladder: bile secreted into bile chemical changes in it. Stomach Holds and mixes food; duct/gall bladder; then into duodenum Gallbladder* glands in lining of upper two thirds produce Sheltered by the liver, digestive juice, which acts It stores bile. • Liver function on protein; lower third Duodenum serves as pump. ~ major metabolic organ in body First part of small intestine; bile from liver breaks up fat Pancreas ~ significant route of xenobiotic excretion and juice from pancreas digests Make enzymes that break all food types. down all types of food. ~ exocrine gland: albumin, clotting factors Portal Vein Carries blood from entire Small Intestine (prothrombin, fibrinogen, factors 7,9,10) digestive tract to liver. -

Motility of Bile Canaliculi in the Living Animal: Implications for Bile Flow Norihito Watanabe, Nobuhiro Tsukada, Charles R
Motility of Bile Canaliculi in the Living Animal: Implications for Bile Flow Norihito Watanabe, Nobuhiro Tsukada, Charles R. Smith, and M. James Phillips Research Institute and Departments of Pathology and Pediatrics, The Hospital for Sick Children and University of Toronto, Toronto, Ontario, Canada M5G 1X8 Abstract. Modem fluorescence microscopic techniques direction towards the portal bile ducts. Contractions were used to image the bile canalicular, system in the were not seen in the network of canaliculi on the sur- intact rat liver, in vivo. By combining the use of sodi- face of the liver. Cytochalasin B administration resulted um fluorescein secretion into bile, with digitally en- in reduced canalicular motility, progressive dilation of hanced fluorescence microscopy and time-lapse video, zone 1 canaliculi, and impairment of bile flow. Cana- it was possible to capture and record the canalicular licular dilations invariably involved the branch points motility events that accompany the secretion of bile in of the canalicular network. The findings add substan- life. Active bile canalicular contractions were found tively to previous in vitro studies using couplets, and predominantly in zone 1 (periportal) hepatocytes of suggest that canalicular contractions contribute physio- the liver. The contractile movements were repetitive, logically to bile flow in the liver. forceful, and appeared unidirectional moving bile in a TIN, myosin and associated proteins involved in con- tile collapses of canaliculi resulting from secretory pressure tractile movements have been found in smooth muscle with rupture of canaliculi (9, 11, 30, 35). In this report, we and nonmuscle cells (1, 16, 18, 24, 42, 43, 56, 61, have taken advantage of the biliary secretion of sodium 65). -

Descriptive Anatomy of Hepatic and Portal Veins with Special Reference
Brazilian Journal of Poultry Science Revista Brasileira de Ciência Avícola Descriptive Anatomy of Hepatic and Portal Veins ISSN 1516-635X 2019 / v.21 / n.2 / 001-012 with Special Reference to Biliary Duct System in Broiler Chickens (Gallus gallus domesticus): http://dx.doi.org/10.1590/1806-9061-2019-0980 A Recent Illustration Original Article Author(s) ABSTRACT Maher MAI https://orcid.org/0000-0002-7040-7813 Chickens have a great participation in meat and egg production. The anatomical scientific data of poultry is important to support the recent researches either for illustrations in academic studies or clinically in diagnosis and treatment of some poultry nutritional diseases. The current investigation was performed on twenty broiler chickens of both sexes. The chickens were anaesthetized, slaughtered then the venous system was flushed with a normal saline to anatomically investigate the distribution of hepatic portal veins both intra and extrahepatic, as well as the hepatic venous and biliary duct systems. The fowl had two hepatic portal veins draining the gastrointestinal tract with its associated organs as spleen and pancreas. The left hepatic portal vein was small, restricted to a limited portion of left hepatic lobe and had been constituted by five main venous tributaries draining the proventriculus, gizzard and pylorus, while the right hepatic portal vein was the largest, receiving the proventriculosplenic, gastropancreaticoduodenal and common mesenteric veins then piercing the right hepatic lobe to be distributed in both hepatic segments through right and left divisions. The fowl has two hepatic portal veins differed in size and distribution. A characteristic imaginary trapezoid shape was formed by some tributaries draining the caudoventral part of the gizzard. -

Cirrhosis and Its Complications Catch This Liver Scarring Problem Early, Because Its Effects Can Be Life-Threatening
Cirrhosis and Its Complications Catch this liver scarring problem early, because its effects can be life-threatening By Scott R. Snyder, BS, NREMT-P, Sean M. Kivlehan, MD, MPH, NREMT-P, & Kevin T. Collopy, BA, FP-C, CCEMT-P, NREMT-P, WEMT This month’s CE article looks at cirrhosis and its complications. In an attempt to best understand the signs and symptoms and progression of this disease, we will review the anatomy, physiology and pathophysiology of the liver and cirrhosis and the clinical manifestations of the disease and its complications. ANATOMY OF THE LIVER The liver is the largest visceral organ in the body, and the majority of its mass is located in the upper right abdominal quadrant and extends into the upper left quadrant, lying directly below the diaphragm. It weighs about 3.3 lbs. (1.5 kg) in the average adult male. The liver is encased in a tough, fi brous capsule (Glisson’s capsule) and covered by a layer of visceral peritoneum. It is held in place in the abdomen by several ligaments, including the falciform, round and coronary ligaments. The gallbladder is a small, hollow, pear-shaped muscular sac that lies on the posterior surface of the liver. While not a true part of the liver, it works closely with the liver to store and secrete bile produced in the liver to aid digestion. Blood Supply The liver is the largest blood reservoir in the body, receiving about 25% of the cardiac output. It is unique in that it has a double blood supply, receiving blood from both the hepatic portal vein and hepatic arteries. -
Question 1. Why Do We Have the Portal Vein Or the Liver Receiving More
Question 1. why do we have the portal vein or the liver receiving more blood from the vein than it receives from the artery? The portal vein or hepatic portal vein (HPV) is a blood vessel that carries blood from the gastrointestinal tract, gallbladder, pancreas and spleen to the liver. This blood contains nutrients and toxins extracted from digested contents. Approximately 75% of total liver blood flow is through the portal vein, with the remainder coming from the hepatic artery proper. The blood leaves the liver to the heart in the hepatic veins. The portal vein is not a true vein, because it conducts blood to capillary beds in the liver and not directly to the heart. It is a major component of the hepatic portal system, one of only two portal venous systems in the body – with the hypophyseal portal system among the other. The portal vein is usually formed by the confluence of the superior mesenteric to splenic veins and also receives blood from the inferior mesenteric left and right gastric veins and cystic veins. Conditions involving the portal vein cause considerable illness and death. An important example of such a condition is elevated blood pressure in the portal vein. This condition, called portal hypertension, is a major complication of cirrhosis. Unlike most veins, the portal vein does not drain into the heart. Rather, it is part of a portal venous system that delivers venous blood into another capillary system, the hepatic sinusoids of the liver. In carrying venous blood from the gastrointestinal tract to the liver, the portal vein accomplishes two tasks: it supplies the liver with metabolic substrates and it ensures that substances ingested are first processed by the liver before reaching the systemic circulation.This accomplishes two things.