Comparison Between Hand Suture and Carter-Thomason Needle Closure of Port Sites in Laparoscopy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Answer Key Chapter 1
Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 1 of 101 Answer Key Chapter 1 Introduction to Clinical Coding 1.1: Self-Assessment Exercise 1. The patient is seen as an outpatient for a bilateral mammogram. CPT Code: 77055-50 Note that the description for code 77055 is for a unilateral (one side) mammogram. 77056 is the correct code for a bilateral mammogram. Use of modifier -50 for bilateral is not appropriate when CPT code descriptions differentiate between unilateral and bilateral. 2. Physician performs a closed manipulation of a medial malleolus fracture—left ankle. CPT Code: 27766-LT The code represents an open treatment of the fracture, but the physician performed a closed manipulation. Correct code: 27762-LT 3. Surgeon performs a cystourethroscopy with dilation of a urethral stricture. CPT Code: 52341 The documentation states that it was a urethral stricture, but the CPT code identifies treatment of ureteral stricture. Correct code: 52281 4. The operative report states that the physician performed Strabismus surgery, requiring resection of the medial rectus muscle. CPT Code: 67314 The CPT code selection is for resection of one vertical muscle, but the medial rectus muscle is horizontal. Correct code: 67311 5. The chiropractor documents that he performed osteopathic manipulation on the neck and back (lumbar/thoracic). CPT Code: 98925 Note in the paragraph before code 98925, the body regions are identified. The neck would be the cervical region; the thoracic and lumbar regions are identified separately. Therefore, three body regions are identified. Correct code: 98926 Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 2 of 101 6. -

AST Guidelines for Counts
Recommended Standard of Practice for Counts Introduction The following Recommended Standards of Practice were researched and written by the AST Education and Professional Standards Committee and have been approved by the AST Board of Directors. They are effective October 27, 2006. AST developed the following Recommended Standards of Practice to support facilities in the reinforcement of best practices, related to performing the sponge, needle and instrument counts in the perioperative setting. The purpose of the Recommended Standards is to provide an outline that surgical team members can use to develop and implement policies and procedures for counts. The Recommended Standards is presented with the understanding that it is the responsibility of the healthcare facility to develop, approve, and establish policies and procedures for performing counts, according to established healthcare facility protocols. Rationale The following are Recommended Standards of Practice related to properly performing sponge, needle and instrument counts in the perioperative setting. It is recommended that sponge, needle and instrument counts be performed on all procedures that present with the possibility that a foreign object could be retained in order to increase patient safety practices in the perioperative setting. Risk factors identified as increasing the occurrence of an incorrect count or retained item include the following: emergency surgical procedures, unexpected change in the scope of the surgical procedure, procedures involving more than one surgical team, extended procedural length of time, unexpected transfusions, and morbidly obese patients.18 One of several safe patient outcomes related to surgery is all items viewed as retainable foreign objects are accounted for at the end of the surgical procedure, due to careful counting and documentation by the surgical team. -

Surgical Products
Cervical & Endocervical Samplers Surgical Products Uterine Manipulation Devices Hysterectomy Instruments Laparoscopic Port-Site Closure Laparoscopic Instruments Laparoscopic Smoke Evacuation Laparoscopic Disposables Trocars Urology Instruments Retractors Delivering on the Promise to Help Clinicians Provide Better Health Care for Women Our mission is to enable physicians to provide increasingly more efficient and effective health care for women. We leverage our expertise in identifying and developing a steady stream of exceptional products that keep Ob/Gyns and others directly involved in caring for women, at the forefront of women’s health care. An Expansive Portfolio of Trusted Brands And Services Since our founding in 1990, CooperSurgical has researched, developed and manufactured a wide range of trusted brands that have advanced the standard of women’s health care. Our products are used by physicians and health care professionals in hospitals and their practices for a wide variety of procedures from basic annual gynecological exams to complex surgical procedures. As a full-service R&D and manufacturing company, we are committed to: • Improved patient outcomes and satisfaction • The highest quality and safety standards in the industry • Clinically proven technologies that provide ease of use • Technical support of our equipment – 20+ years of experience • Innovative solutions that reduce procedural costs • Annual support of medical professional educational organizations • Educational and in-service support of our products • Personalized service and a commitment to your satisfaction by educated professional representatives We appreciate the opportunity to partner with you to provide optimum health care for women. 2 To place an order, call us at: 800.243.2974 | Visit us online at: www.CooperSurgical.com About CooperSurgical Delivering on the Promise to Help Clinicians Provide Better Health Care for Women Industry-Leading Solutions for Laparoscopic and General Surgical Procedures CooperSurgical instruments are used every day in surgical procedures. -
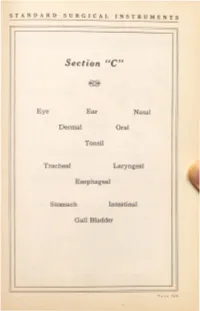
Surgical Instruments
STANDARD SURGICAL INSTRUMENTS Section ''C'' Eye Ear Nasal Dermal Oral Tonsil Tracheal Laryngeal Esophageal Stomach Intestinal Gall Bladder ST ANDARD SURGICAL INSTRUMENTS C-10 C-30 C-40 - 3 Condensing Lenses, Illuminators, Ophthalmoscopes and Retinoscopes ·c- . <...onden ing Len~. 2 inches. hard rubber rim, 13 dtoptar. ·c ond n mg Len . double. 1:3 and dioptar. ·c- 1 ond n 'ng Len • \\ith metal rim and handle. ·c Dr . Berger's upc ''ith met I hea band. ·c- 9 Dr. Bez:ger's upe with \\ebbiog head band. C-10 Ocular Transilluminator. E .S.I.Co. ·c-11 Ophthalmoscope. Loring's, 1 len . "C-12 Oph halmoscope, loring's, lectrical, with mtrror, in ca . •c-13 Ophthalmoscope, Morton 's, lectrical. with mtrror. on battery hand! . · C- 14 Retinoscope ?o.lirror. r lain or conca c. 11 mch . regtlar hand! . ·c-1s Retinoscope Mtrror, r lain or conca e, 1Y2 inchc , folding handle ·c-1 R tino ope firror, Thor ington's, % inch. •C- 17 Retino · ope ftrror, T h or ington's, % inch, with folding cover ·c-1 Retinoscope, lectrical, on battery handle, in case. •C-19 Retinoscope and Ophthalmoscope, electrical, on battery handle, in case. ·c-20 Ashe tos Chimney, with iris dtaphragm. Eyelid Retractors C-30 Desrna rre's, 4 izes. ·c-a Fish er 's, lid hook, double. latest model. C-3 Fi h er 's, fen trated. flexibl for shaping. C-37 Fisher 's, solid, fl xiblc for haping. C- Fish er 's, for lov r ltd. C 0 Ziegler's, one size. P A CE 170 STANDARD SURGICAL INSTRUMENTS ( ,)() . -

Aesculap Spine Miaspas TL
Aesculap Spine Miaspas TL Spinal Microsurgical Endoscopy THORACOSCOPIC LAPAROSCOPIC CONTENTS PAGE INTRODUCTION 3 RONGEURS AND NUCLEUS-GRASPING FORCEPS 5 BONE PUNCHES 6 APPLICATION OF THE SLIDING TUBE 7 DISSECTORS AND EXPLORATION HOOKS 8 SCOOPS 9 CURETTES, OSTEOTOMES AND IMPACTORS 10 LUNG SPATULA AND RIB ELEVATOR 11 SPECULUM, DILATOR ROD, BONE-GRAFT-HOLDER AND BONE GRAFT MEASUREMENT INSTRUMENT 12 DRILL, BURRS AND HAND PIECE 13 TROCARS COMPLETE 14 TROCAR SYSTEM 16 BIPOLAR FORCEPS 17 FURTHER ENDOSCOPIC INSTRUMENTS AND MOTOR LINE EQUIPMENT SEE FOLLOWING LEAFLETS 18 AESCULAP SPINE PRODUCTS 19 2 SPINAL MICROSURGICAL ENDOSCOPY The miaspasTL instrument system was developed in co-operation with Daniel Rosenthal, MD. Praxisklinik Bad Homburg Hessenring 128 A 61348 Bad Homburg Germany to safely perform microsurgical endoscopic surgery on the thoracic and lumbar spine. Microsurgical endoscopy - as the name suggests - is a technique based on two of the most minimally invasive or least traumatic current techniques for spinal surgery. The miaspasTL instruments are designed with the surgeon in mind, to facilitate spinal microsurgical endoscopic procedures. Main advantages of the miaspasTL instrument system: ➠ microsurgical endoscopic technique promotes minimal patient trauma ➠ suitable for both laparoscopic (using gas insufflation) and thoracoscopic (gasless) procedures ➠ well balanced instrument design ensures easy handling ➠ high quality reusable instruments ensure cost savings ➠ instrumentation is easily disassembled for cleaning prior to sterilisation -

United States Patent (19) 11 Patent Number: 4,545,374 Jacobson 45 Date of Patent: Oct
United States Patent (19) 11 Patent Number: 4,545,374 Jacobson 45 Date of Patent: Oct. 8, 1985 54 METHOD AND INSTRUMENTS FOR PERFORMING A PERCUTANEOUS OTHER PUBLICATIONS LUMBAR DISKECTOMY "Nucleography”, May 1952, issue of Journal of Bone (76) Inventor: Robert E. Jacobson, 1295 NW. 14th and Joint Surgery, vol. 34B, No. 2. St., Suite G, Miami, Fla. 33125 "Dr. Parvas Kanbin Develops New Surgical Procedure Aiding Herniated Spinal Disk Sufferers', May 1982, 21) Appl. No.: 414,779 issue of Image, vol. 6, No. 5. 22) Filed: Sep. 3, 1982 "Microlumbar Discectomy', Feb. 1982, issue of Resi dent and Staff Physician. (51) Int. Cl." .............................................. A61B 17/00 52 U.S. C. ................................ 128/303 R; 128/305; "Oh, My Aching Back', p. D1, Saturday, Nov. 7, 1981, 128/312; 128/348.1; 604/164; 604/264 issue of The Miami Herald. 58) Field of Search .............. 128/348.1, 92 E, 92 EB, "Percutaneous Lumbar Discectomy', 1981, Dr. Robert 128/303 R, 753-754, 341-343, 345, 3, 126, E. Jacobson. 305.3, 741, 303.11, 303.13,783-784, 362; Primary Examiner-C. Fred Rosenbaum 604/22, 164-166, 264,904 Assistant Examiner-Gene B. Kartchner 56) References Cited Attorney, Agent, or Firm-Pennie & Edmonds U.S. PATENT DOCUMENTS (57) ABSTRACT 2,991,787 7/1961 Shelden et al. .................. 128/305.3 A method for percutaneously accessing the lumbar 3,308,819 3/1967 Arp ..................................... 604/164 region of the spinal column by laterally inserting a can 3,320,131 5/1967 Smith . nula through the patient's side above the pelvic crest to 3,320,948 5/1967 Martin .................................. -

Instruments 449-478 4/3/06 10:42 AM Page 449
Instruments_449-478 4/3/06 10:42 AM Page 449 Neuro Hammers & Diagnostic ADC® NEUROLOGICAL HAMMERS Four of the most popular hammers for diagnosis of neurological function. 369110105375 Buck Hammer, 7 1/4˝, Chrome Plated Handle w/2 sided rubber head, Handle Conceals “screw-in” Brush, Needle Contained Within The Head 369310105374 Taylor Hammer, 7 1/2˝, Chrome Handle w/triangular rubber head, Orange 3693BK10141795 Taylor Hammer, 7 1/2˝, Chrome Handle w/triangular rubber head, Black 3693DG10141796 Taylor Hammer, 7 1/2˝, Chrome Handle w/triangular rubber head, Dark Green 3693RB10141797 Taylor Hammer, 7 1/2˝, Chrome Handle w/triangular rubber head, ADC® TUNING FORKS Royal Blue 369510105372 Wartenberg Pinwheel, 7 1/2˝, Stainless Steel Handle w/textured grip, Non magnetic, corrosion resistant aluminum alloy construction weighs 1/3 of Rotating Spur comparable steel tuning forks. Produced from 3/8˝ x 1˝ bar stock for superior 369710105373 Babinski Hammer, 8 1/2˝, Octagonal Stainless Steel Handle w/concealed performance and consistent frequency accuracy. Extra long 2˝ handle of turned needle, Rubber Head smooth aluminum to facilitate bone conduction tests. 50012810105366 Tuning Fork w/fixed weight, 128cps Frequency 50025610105367 Tuning Fork w/fixed weight, 256cps Frequency 50051210105368 Tuning Fork w/o weight, 512cps Frequency 50102410105369 Tuning Fork w/o weight, 1024cps Frequency 50204810105370 Tuning Fork w/o weight, 2048cps Frequency 50409610105371 Tuning Fork w/o weight, 4096cps Frequency 1-200 1-220 MILTEX HAMMERS 1-20010090643 Taylor Percussion -
Design and Fabrication of a Trocar Attachment for Laparoscopic Bariatric Surgery
Design and Fabrication of a Trocar Attachment for Laparoscopic Bariatric Surgery A Major Qualifying Project Report Submitted to the Faculty of Worcester Polytechnic Institute In partial fulfillment of the requirements for the Degree of Bachelor Science By Katherine Handy _________________________ Alexis Mittelman _________________________ Amanda St Germain _________________________ Natalie Toomey _________________________ Date: 12 May 2020 Report Submitted to: Dr. Tiffiny Butler PhD, ATC; Advisor ______________________________ This report represents the work of four WPI undergraduate students submitted to the faculty as evidence of completion of a degree requirement. WPI routinely publishes these reports on its website without editorial or peer review. For more information about the projects program at WPI, please see: http://www.wpi.edu/Academics/Projects TABLE OF CONTENTS AUTHORSHIP PAGE 5 ACKNOWLEDGEMENTS 6 ABSTRACT 7 TABLE OF FIGURES 8 TABLE OF TABLES 9 CHAPTER 1 - INTRODUCTION 10 CHAPTER 2 - LITERATURE REVIEW 13 2.1 Laparoscopic Surgery 13 2.1.1 History 14 2.1.2 Equipment 15 2.1.3 Limitations 17 2.1.4 Adverse Events 18 2.1.4.1 Access Complications 18 2.1.4.2 Physiologic Complications of the Pneumoperitoneum 18 2.1.5 Benefits 19 2.2 Bariatric Surgery 19 2.2.1 Conditions for Surgery 21 2.2.2 Types of Bariatric Surgery 21 2.2.2.1 Sleeve Gastrectomy 22 2.2.2.2 Roux-en-Y Gastric Bypass 24 2.2.2.3 Gastric Bypass Revision 25 2.2.2.4 Lap-Band Surgery 27 2.3 Surgical Trocars 28 2.3.1 History 28 2.3.2 Structure 29 2.3.3 Important Features -
Abdominal Access Technique
56 Textbook of Practical Laparoscopic Surgery 5 Abdominal Access Technique Minimal access surgery, a new surgical and access surgical procedures like axilloscopy, interventional approach was called by different name retroperitoneoscopy and totally extraperitoneal and one of the popular is minimally invasive surgery. approach of hernia repair. In general, closed technique However, this terminology is considered inappropriate by Veress needle is possible only if there is a preformed by Prof. Cuschieri for two reasons. Firstly, it carries cavity like abdomen. connotations of increased safety, which is not the case. Secondly, it is semantically incorrect since to invade is OPEN ACCESS absolute, and indeed such interventions are as invasive In this, there is direct entry by open technique, without as open surgery in terms of reach of the various organs creating pneumoperitoneum and insufflator is and tissues. The hallmark of the new approaches is connected once blunt trocar is inside the abdominal Section One the reduction in the trauma of access. Hence, a more cavity under direct vision. There are various ways of appropriate generic term is minimal access therapy. open access like Hasson’s technique, Scandinavian In minimal access surgery, the technique of first technique and Fielding technique. entry inside the human body with telescope and Some surgeons and gynecologists practice blind instruments is called access technique. Technique of trocar insertion without pneumoperitoneum. The access is different for different minimal access surgical incidence of injury due to this type of access is much procedures. Thoracoscopy, retroperitoneoscopy, higher. This type of direct trocar entry is practiced by axilloscopy have different ways of access. -

Clinical Experience with an Optical Access Trocar in Gynecological Laparoscopy-Pelviscopy
SCIENTIFIC PAPERS JSLS Clinical Experience with an Optical Access Trocar in Gynecological Laparoscopy-Pelviscopy L Mettler, Prof Dr med, M. Ibrahim, MD, Vu Quang Vinh, W. Jonat, Prof Dr med ABSTRACT INTRODUCTION Background and Objectives: Development in surgical Obstetric and gynecological pelviscopic-laparoscopic technology must demand not only improved efficacy and surgery has recently made great progress due to improve- risk reduction but also a reduction in costs and efficient use ments in optics, energy sources, mechanical instrumentation of human resources. For 25 years we have discussed the and training of surgeons.1,2 Improvements in efficiency and development of optical access trocars and their probable safety have been achieved in robotics, computer systems benefits. They are now available in the form of the and optics through an interchange of ideas and technology OPTIVIEW by Ethicon and the SURGIVIEW by US Surgical. by colleagues performing laparoscopic surgery in different surgical specialties. Examples include 3-D optics, the robot- Methods: Between December 1996 and March 1997, we ic arm, harmonic scalpel and head-mounted display.3-5 utilized the optic obturator trocar, OPTIVIEW, in 104 cases Another such sophisticated technology is the optical access of gynecological operative laparoscopy. The instrument trocar, OPTIVIEW (Ethicon GmbH & Co. KG, was equipped with an axial grip to facilitate ergonomic Hummelsblitteler Steindamm 71, 22851 Norderstedt, handling. Germany). This instrument allows entry into the abdominal cavity under direct vision. In 1994, Semm recommended Results: The optical trocar was used with a Z-incision entry under direct vision and suggested a "2"-entry into the technique in 46 cases; a vertical incision was used in 58 abdominal cavity using a 5 mm optic and conical 5 mm tro- cases. -

Spring Case Study &
Dear SCQRs, Based on your feedback for more SCQR-specific education, we are trialing this case study review containing commonly asked SCQR questions. Feel free to discuss the case with your colleagues within the SCQR Forum. We will not be providing the correct responses, rationale, and any needed clarifications until Tuesday, April 9th, so there is plenty of time for a thorough examination of the case. This case study and the answer key will also be posted on the SCQR Forum. We hope to see some great discussions! Cheryl and Rhonda DATE OF OPERATION: 01/02/2018 PREOPERATIVE DIAGNOSIS: Colon cancer POSTOPERATIVE DIAGNOSIS: Colon cancer OPERATION PERFORMED: Laparoscopic right hemicolectomy SURGEON: John Doe, MD ANESTHESIA: General endotracheal SPECIMENS: Right hemicolectomy ESTIMATED BLOOD LOSS: Less than 200 mL DRAINS: None DESCRIPTION OF OPERATION: After the patient was consented for laparoscopic right hemicolectomy, the patient was taken to the operating room and given general endotracheal anesthesia. He was placed in the supine position. A Foley catheter was placed. The abdomen was prepped and draped in the standard surgical fashion. Incision was carried down in the umbilicus approximately half inch in length with the use of a scalpel. A Veress needle was introduced. The abdominal cavity was insufflated with CO2 gas. Next, 12 mm bladeless trocar was introduced into the abdominal cavity with ease. The abdominal cavity was then reinsufflated. A 10 mm, 30-degree scope was placed in the abdominal cavity. There was no evidence of any injury from the Veress needle or trocar. An additional 5 mm trocar was placed in the suprapubic position after a small stab incision was created with a 15 blade. -
Different Port Closure Techniques in Laparoscopy Surgery Different Port Closure Techniques in Laparoscopy Surgery
REVIEW ARTICLE Different Port Closure Techniques in Laparoscopy Surgery Different Port Closure Techniques in Laparoscopy Surgery 1Majid A Hamood, 2RK Mishra 1Department of Surgery, Hilla Teaching Hospital, PO Box 294, Babil, Hilla, Iraq 2Department of Surgery, Laparoscopy Hospital, New Delhi, India Abstract Introduction: Any new surgical procedure, face a new technical challenges, although minimally invasive surgery cause evident reduction of the pain to the patient postoperatively, with better cosmesis, but with time, new challenges appears. One of challenges is port closure techniques, in order to prevent the trocar site hernias and other complications . Aims: The aim of this study to review and list different techniques used for closure of the trocar sites. Methods: A literature search was performed for articles and text books dealing with techniques of closure. The author searched this subject using Medline and the search engine Google, Springerlink and High wire Press. The following search term were used; port site closure techniques. Review, All articles reporting techniques with their references were reviewed with some text books. Results: in this literature review we described many techniques in addition to classical closure using curved needles, including Grice needle, Maciol-needles, endoclose device. Carter-Thomason device, Tahoe ligature device, Endo-Judge device, exit puncture closure device, Owsley retractor, spinal cord needles, dual hemostat, Veress needle loop technique,suture carrier, Riverdin and Deschamps needles, and Gore-Tex closure device. Semm's emergency needle with adistal eyelet; the modified Veress needle with a slit made in the retractable brunt tip; dental awl with aneye; prolene 2/0 on a straight needle aided by a Veress needle; a straight needle armed with suture; Auto stitch (United States Surgical), a modified Veress needle bearing a crochet hook at the tip.