Abdominal Access Technique
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Single Port Laparoscopic Hysterectomy Through a 12Mm Incision Created by a Bladeless Trocar: a Novel Technique
Single Port Laparoscopic Hysterectomy through a 12mm incision created by a Bladeless Trocar: A Novel Technique Greg J. Marchand, M.D., Katelyn M. Sainz MS1 From the National Foundation for Minimally Invasive Surgery (minvase.org), and Research and Development division of Marchand OBGYN PLLC Precis: Single Port Hysterectomy can be performed safely through a 12mm bladeless incision via this novel technique. Decreasing port size is continually pushing the limits of minimally invasive surgery for enhanced patient outcomes. Corresponding author: Greg J. Marchand M.D., Marchand OBGYN Research and Development, 1520 S. Dobson #218, Mesa, AZ 85202, Tel: 480-628-0566, Fax: 480-999-0801 ABSTRACT Study Objective: The aim of this study is to report the technique used by one surgeon performing a laparoscopic hysterectomy performed through a single 12mm bladeless incision. With the exception of pure vaginal hysterectomy we believe this technique is the least invasive technique published thus far to date where the hysterectomy is performed entirely abdominally. Design: Retrospective Analysis of Charts and Technique Setting: One private Hospital in the Southwest US Patients: 6 patients receiving single port hysterectomy between 2013 and 2014 Intervention: Single Port Laparoscopic Hysterectomy was performed with our ultra-minimally invasive technique, using a Covidien(C) 12mm bladeless laparoscopic trocar followed by an Olympus(C) TriPort device and Olypus(C) articulating 5mm laparoscope without in any way stretching or extending the 12mm port. Other novel aspects of our technique include placement of the single port at the bottom of the umbilicus regardless of patient BMI, the usage of intra-abdominal marcaine to help with postoperative pain and vaginal repair of colpotomy. -

Entry Techniques in Gynecologic Laparoscopy—A Review
Gynecol Surg (2012) 9:139–146 DOI 10.1007/s10397-011-0710-8 REVIEW ARTICLE Entry techniques in gynecologic laparoscopy—a review Johannes Ott & Agnes Jaeger-Lansky & Gunda Poschalko & Regina Promberger & Eleen Rothschedl & René Wenzl Received: 9 June 2011 /Accepted: 19 October 2011 /Published online: 13 November 2011 # Springer-Verlag 2011 Abstract Laparoscopy is one of the most common surgical underpowered in order to assess the risk for rare but life- procedures in gynecologic medicine. Major complications threatening complications. In conclusion, there is no solid associated with gynecologic laparoscopy are relatively rare, evidence proving the superiority of any method of with up to 50% related to laparoscopic entry. Several entry laparoscopic entry. techniques have been developed, all of which aim to provide a safe and easy entry to the abdominal cavity. In Keywords Laparoscopy. Entry techniques . Gynecology. this article, we aim to review the available evidence on Complications . Veress needle . Hasson technique . Direct laparoscopic entry techniques in gynecologic surgery. We trocar entry found no evidence that the Hasson (open) technique is superior to the Veress needle entry, the preferred method of most gynecologists all over the world. When entering the Background abdomen using the Veress needle, an intraperitoneal pressure <10 mmHg is a reliable predictor of correct Laparoscopy is one of the most common surgical intraperitoneal placement. Entry at Palmer’s point (left procedures in gynecologic medicine and has become upper quadrant laparoscopy) is recommended for patients the method of choice over the last few decades for with suspected or known periumbilical adhesions, or a treating benign diseases that require surgery [1, 2]. -

Comparison Between Different Entry Techniques in Performing Pneumoperitoneum In10.5005/Jp-Journals-10033-1257 Laparoscopic Gynecological Surgery REVIEW ARTICLE
WJOLS Comparison between Different Entry Techniques in Performing Pneumoperitoneum in10.5005/jp-journals-10033-1257 Laparoscopic Gynecological Surgery REVIEW ARTICLE Comparison between Different Entry Techniques in Performing Pneumoperitoneum in Laparoscopic Gynecological Surgery Mandavi Rai ABSTRACT safety of one technique over another. However, the included studies are small and cannot be used to confirm safety of any Background: The main challenge facing the laparoscopic particular technique. No single technique or instrument has surgery is the primary abdominal access, as it is usually a blind been proved to eliminate laparoscopic entry-associated injury. procedure associated with vascular and visceral injuries. Lapa- Proper evaluation of the patient, supported by good surgical roscopy is a very common procedure in gynecology. Complica- skills and reasonably good knowledge of the technology of the tions associated with laparoscopy are often related to entry. instruments remain to be the cornerstone for safe access and The life-threatening complications include injury to the bowel, success in minimal access surgery. bladder, major abdominal vessels, and anterior abdominal- wall vessel. Other less serious complications can also occur, Keywords: Complications, Laparoscopy, Pnumoperitoneum, such as postoperative infection, subcutaneous emphysema Trocar. and extraperitoneal insufflation. There is no clear consensus as to the optimal method of entry into the peritoneal cavity. It How to cite this article: Rai M. Comparison between Dif- has been proved from studies that 50% of laparoscopic major ferent Entry Techniques in Performing Pneumoperitoneum complications occur prior to the commencement of the surgery. in Laparos copic Gynecological Surgery. World J Lap Surg The surgeon must have adequate training and experience in 2015;8(3):101-106. -

Use of the Veress Needle to Obtain Pneumoperitoneum Prior to Laparoscopy
Use of the Veress needle to obtain pneumoperitoneum prior to laparoscopy Consensus statement of the Royal Australian & New Zealand College of Obstetricians & Gynaecologists This statement has been developed by the Women’s (RANZCOG) and the Australasian Gynaecological Health Committee. It has been reviewed by the Endoscopy and Surgery Society (AGES). Endoscopic Surgery Advisory Committee (RANZCOG/AGES) and approved by the Objectives: To provide advice on the use of the RANZCOG Board and Council. Veress needle to obtain pneumoperitoneum prior to laparoscopy. A list of Women’s Health Committee and Endoscopic Surgery Advisory Committee Target audience: Health professionals providing (RANZCOG/AGES) Members can be found in gynaecological care, and patients. Appendix A. Values: The evidence was reviewed by the Disclosure statements have been received from all Endoscopic Surgery Advisory Committee members of this committee. (RANZCOG/AGES), and applied to local factors relating to Australia and New Zealand. Disclaimer This information is intended to provide Background: This statement was first developed by general advice to practitioners. This information Women’s Health Committee in April 1990 and most should not be relied on as a substitute for proper recently reviewed by the Endoscopic Surgery assessment with respect to the particular Committee (RANZCOG/AGES) in July 2017. circumstances of each case and the needs of any patient. This document reflects emerging clinical Funding: The development and review of this and scientific advances as of the date issued and is statement was funded by RANZCOG. subject to change. The document has been prepared having regard to general circumstances. First endorsed by RANZCOG: April 1990 Current: July 2017 Review due: July 2020 1 Table of contents Table of contents ............................................................................................................................ -

AUA BLUS Handbook of Laparoscopic and Robotic Fundamentals
AUA BLUS Handbook of Laparoscopic and Robotic Fundamentals Sean Collins, Daniel S. Lehman, Elspeth M. McDougall, Ralph V. Clayman, and Jaime Landman ©American Urological Association Education & Research, Inc. Table of Contents 1. Introduction 2. Patient selection a. Indication b. contradindications c. special considerations 3. Physiologic effects of pneumoperitoneum a. Renal surgery transperitoneal b. Renal surgery retroperitoneal c. Hand-assisted laparoscopic nephrectomy d. Prostatectomy 4. Getting Started 5. Patient positioning a. Renal surgery transperitoneal b. Renal surgery retroperitoneal c. Hand-assisted laparoscopic nephrectomy d. Prostatectomy 6. Strategic placement of surgical team and operating room (OR) equipment 7. Access a. Primary access b. Renal surgery transperitoneal trocar placement c. Renal surgery retroperitoneal trocar placement d. Secondary access e. Retroperitoneal primary and secondary access f. Hand-assisted laparoscopic nephrectomy trocar placement g. Prostatectomy trocar placement 8. Instrumentation a. Trocars i. Cutting ii. Dilating iii. Radially dilating b. Bipolar cautery c. Monopolar cautery d. Ultrasonic instrumentation e. Vessel sealing devices i. LigaSure ii. Enseal f. Staplers g. Vascular clamps h. Suture anchors i. Titanium clips j. Locking clips q. Retractors r. Hemostatic agents s. Hand Assisted devices 2 9. Technique for Transperitoneal Laparoscopic Nephrectomy 10. Complications of laparoscopic surgery 3 Chapter 1. Introduction The American Urological Association (AUA) has prepared this handbook for all those new to laparoscopy. Rather than being a detailed surgical atlas, this is a handbook designed to introduce the fundamental principles of laparoscopy including: indications and contraindications for laparoscopy, the physiologic effects of pneumoperitoneum, patient positioning; abdominal access and trocar placement; strategic placement of the operating room (OR) team and equipment, overview of laparoscopic instrumentation, and complications unique to laparoscopic surgery. -
Answer Key Chapter 1
Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 1 of 101 Answer Key Chapter 1 Introduction to Clinical Coding 1.1: Self-Assessment Exercise 1. The patient is seen as an outpatient for a bilateral mammogram. CPT Code: 77055-50 Note that the description for code 77055 is for a unilateral (one side) mammogram. 77056 is the correct code for a bilateral mammogram. Use of modifier -50 for bilateral is not appropriate when CPT code descriptions differentiate between unilateral and bilateral. 2. Physician performs a closed manipulation of a medial malleolus fracture—left ankle. CPT Code: 27766-LT The code represents an open treatment of the fracture, but the physician performed a closed manipulation. Correct code: 27762-LT 3. Surgeon performs a cystourethroscopy with dilation of a urethral stricture. CPT Code: 52341 The documentation states that it was a urethral stricture, but the CPT code identifies treatment of ureteral stricture. Correct code: 52281 4. The operative report states that the physician performed Strabismus surgery, requiring resection of the medial rectus muscle. CPT Code: 67314 The CPT code selection is for resection of one vertical muscle, but the medial rectus muscle is horizontal. Correct code: 67311 5. The chiropractor documents that he performed osteopathic manipulation on the neck and back (lumbar/thoracic). CPT Code: 98925 Note in the paragraph before code 98925, the body regions are identified. The neck would be the cervical region; the thoracic and lumbar regions are identified separately. Therefore, three body regions are identified. Correct code: 98926 Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 2 of 101 6. -

AST Guidelines for Counts
Recommended Standard of Practice for Counts Introduction The following Recommended Standards of Practice were researched and written by the AST Education and Professional Standards Committee and have been approved by the AST Board of Directors. They are effective October 27, 2006. AST developed the following Recommended Standards of Practice to support facilities in the reinforcement of best practices, related to performing the sponge, needle and instrument counts in the perioperative setting. The purpose of the Recommended Standards is to provide an outline that surgical team members can use to develop and implement policies and procedures for counts. The Recommended Standards is presented with the understanding that it is the responsibility of the healthcare facility to develop, approve, and establish policies and procedures for performing counts, according to established healthcare facility protocols. Rationale The following are Recommended Standards of Practice related to properly performing sponge, needle and instrument counts in the perioperative setting. It is recommended that sponge, needle and instrument counts be performed on all procedures that present with the possibility that a foreign object could be retained in order to increase patient safety practices in the perioperative setting. Risk factors identified as increasing the occurrence of an incorrect count or retained item include the following: emergency surgical procedures, unexpected change in the scope of the surgical procedure, procedures involving more than one surgical team, extended procedural length of time, unexpected transfusions, and morbidly obese patients.18 One of several safe patient outcomes related to surgery is all items viewed as retainable foreign objects are accounted for at the end of the surgical procedure, due to careful counting and documentation by the surgical team. -

Intraperitoneal Access by Closed Method (Veress Needle) Versus Open (Hasson’S) Method in Laparoscopic Surgery to Create Pneumoperitoneum
International Surgery Journal Chotai NR et al. Int Surg J. 2017 Aug;4(8):2786-2790 http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902 DOI: http://dx.doi.org/10.18203/2349-2902.isj20173419 Original Research Article Intraperitoneal access by closed method (veress needle) versus open (Hasson’s) method in laparoscopic surgery to create pneumoperitoneum Neet R. Chotai*, Dilip B. Choksi, Sushil Damor, Amul Bhedi Department of General Surgery, Government Medical College Baroda, Vadodara, India Received: 18 May 2017 Accepted: 17 June 2017 *Correspondence: Dr. Neet R. Chotai, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Access into the abdomen is the one challenge of laparoscopy that is particular to the insertion of surgical instruments through small incisions. In the last three decades, rapid advances in laparoscopic surgery have made it an invaluable part of general surgery, but there remains no clear consensus as an on optimal method of entry into the peritoneal cavity. The objective of this study was to study the comparison and efficacy between closed (veress needle)and open method (Hasson’s) of intraperitoneal access to create pneumoperitoneum in laparoscopic surgeries. Methods: All patients >18 year undergoing laparoscopic procedure at Sir Sayajirao Gaekwad Hospital attached to Medical College Baroda from November 2015 to November 2016, and include 160 patients. -

Surgical Products
Cervical & Endocervical Samplers Surgical Products Uterine Manipulation Devices Hysterectomy Instruments Laparoscopic Port-Site Closure Laparoscopic Instruments Laparoscopic Smoke Evacuation Laparoscopic Disposables Trocars Urology Instruments Retractors Delivering on the Promise to Help Clinicians Provide Better Health Care for Women Our mission is to enable physicians to provide increasingly more efficient and effective health care for women. We leverage our expertise in identifying and developing a steady stream of exceptional products that keep Ob/Gyns and others directly involved in caring for women, at the forefront of women’s health care. An Expansive Portfolio of Trusted Brands And Services Since our founding in 1990, CooperSurgical has researched, developed and manufactured a wide range of trusted brands that have advanced the standard of women’s health care. Our products are used by physicians and health care professionals in hospitals and their practices for a wide variety of procedures from basic annual gynecological exams to complex surgical procedures. As a full-service R&D and manufacturing company, we are committed to: • Improved patient outcomes and satisfaction • The highest quality and safety standards in the industry • Clinically proven technologies that provide ease of use • Technical support of our equipment – 20+ years of experience • Innovative solutions that reduce procedural costs • Annual support of medical professional educational organizations • Educational and in-service support of our products • Personalized service and a commitment to your satisfaction by educated professional representatives We appreciate the opportunity to partner with you to provide optimum health care for women. 2 To place an order, call us at: 800.243.2974 | Visit us online at: www.CooperSurgical.com About CooperSurgical Delivering on the Promise to Help Clinicians Provide Better Health Care for Women Industry-Leading Solutions for Laparoscopic and General Surgical Procedures CooperSurgical instruments are used every day in surgical procedures. -
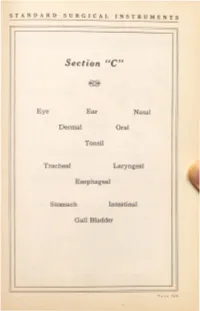
Surgical Instruments
STANDARD SURGICAL INSTRUMENTS Section ''C'' Eye Ear Nasal Dermal Oral Tonsil Tracheal Laryngeal Esophageal Stomach Intestinal Gall Bladder ST ANDARD SURGICAL INSTRUMENTS C-10 C-30 C-40 - 3 Condensing Lenses, Illuminators, Ophthalmoscopes and Retinoscopes ·c- . <...onden ing Len~. 2 inches. hard rubber rim, 13 dtoptar. ·c ond n mg Len . double. 1:3 and dioptar. ·c- 1 ond n 'ng Len • \\ith metal rim and handle. ·c Dr . Berger's upc ''ith met I hea band. ·c- 9 Dr. Bez:ger's upe with \\ebbiog head band. C-10 Ocular Transilluminator. E .S.I.Co. ·c-11 Ophthalmoscope. Loring's, 1 len . "C-12 Oph halmoscope, loring's, lectrical, with mtrror, in ca . •c-13 Ophthalmoscope, Morton 's, lectrical. with mtrror. on battery hand! . · C- 14 Retinoscope ?o.lirror. r lain or conca c. 11 mch . regtlar hand! . ·c-1s Retinoscope Mtrror, r lain or conca e, 1Y2 inchc , folding handle ·c-1 R tino ope firror, Thor ington's, % inch. •C- 17 Retino · ope ftrror, T h or ington's, % inch, with folding cover ·c-1 Retinoscope, lectrical, on battery handle, in case. •C-19 Retinoscope and Ophthalmoscope, electrical, on battery handle, in case. ·c-20 Ashe tos Chimney, with iris dtaphragm. Eyelid Retractors C-30 Desrna rre's, 4 izes. ·c-a Fish er 's, lid hook, double. latest model. C-3 Fi h er 's, fen trated. flexibl for shaping. C-37 Fisher 's, solid, fl xiblc for haping. C- Fish er 's, for lov r ltd. C 0 Ziegler's, one size. P A CE 170 STANDARD SURGICAL INSTRUMENTS ( ,)() . -

Aesculap Spine Miaspas TL
Aesculap Spine Miaspas TL Spinal Microsurgical Endoscopy THORACOSCOPIC LAPAROSCOPIC CONTENTS PAGE INTRODUCTION 3 RONGEURS AND NUCLEUS-GRASPING FORCEPS 5 BONE PUNCHES 6 APPLICATION OF THE SLIDING TUBE 7 DISSECTORS AND EXPLORATION HOOKS 8 SCOOPS 9 CURETTES, OSTEOTOMES AND IMPACTORS 10 LUNG SPATULA AND RIB ELEVATOR 11 SPECULUM, DILATOR ROD, BONE-GRAFT-HOLDER AND BONE GRAFT MEASUREMENT INSTRUMENT 12 DRILL, BURRS AND HAND PIECE 13 TROCARS COMPLETE 14 TROCAR SYSTEM 16 BIPOLAR FORCEPS 17 FURTHER ENDOSCOPIC INSTRUMENTS AND MOTOR LINE EQUIPMENT SEE FOLLOWING LEAFLETS 18 AESCULAP SPINE PRODUCTS 19 2 SPINAL MICROSURGICAL ENDOSCOPY The miaspasTL instrument system was developed in co-operation with Daniel Rosenthal, MD. Praxisklinik Bad Homburg Hessenring 128 A 61348 Bad Homburg Germany to safely perform microsurgical endoscopic surgery on the thoracic and lumbar spine. Microsurgical endoscopy - as the name suggests - is a technique based on two of the most minimally invasive or least traumatic current techniques for spinal surgery. The miaspasTL instruments are designed with the surgeon in mind, to facilitate spinal microsurgical endoscopic procedures. Main advantages of the miaspasTL instrument system: ➠ microsurgical endoscopic technique promotes minimal patient trauma ➠ suitable for both laparoscopic (using gas insufflation) and thoracoscopic (gasless) procedures ➠ well balanced instrument design ensures easy handling ➠ high quality reusable instruments ensure cost savings ➠ instrumentation is easily disassembled for cleaning prior to sterilisation -
Development of an Intraperitoneal Catheter Placement Device for Use on the Battlefield
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Mechanical (and Materials) Engineering -- Mechanical & Materials Engineering, Dissertations, Theses, and Student Research Department of 5-2021 Development of an Intraperitoneal Catheter Placement Device for Use on the Battlefield Riley Reynolds University of Nebraska-Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/mechengdiss Part of the Biomedical Devices and Instrumentation Commons, Materials Science and Engineering Commons, and the Mechanical Engineering Commons Reynolds, Riley, "Development of an Intraperitoneal Catheter Placement Device for Use on the Battlefield" (2021). Mechanical (and Materials) Engineering -- Dissertations, Theses, and Student Research. 164. https://digitalcommons.unl.edu/mechengdiss/164 This Article is brought to you for free and open access by the Mechanical & Materials Engineering, Department of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Mechanical (and Materials) Engineering -- Dissertations, Theses, and Student Research by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. DEVELOPMENT OF AN INTRAPERITONEAL CATHETER PLACEMENT DEVICE FOR USE ON THE BATTLEFIELD By Riley Reynolds A THESIS Presented to the Faculty of The Graduate College at the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Master of Science Major: Mechanical Engineering and Applied Mechanics Under the Supervision of Professor Benjamin S. Terry Lincoln, Nebraska May 2021 DEVELOPMENT OF AN INTRAPERITONEAL CATHETER PLACEMENT DEVICE FOR USE ON THE BATTLEFIELD Riley Reynolds, M.S. University of Nebraska, 2021 Adviser: Benjamin Terry The objective of this project was to simplify peritoneal cavity access so an Airforce field medic can safely infuse oxygen microbubbles (OMBs) into the intraperitoneal space for the emergency treatment of hypoxia due to lung damage.