Development of an Intraperitoneal Catheter Placement Device for Use on the Battlefield
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Single Port Laparoscopic Hysterectomy Through a 12Mm Incision Created by a Bladeless Trocar: a Novel Technique
Single Port Laparoscopic Hysterectomy through a 12mm incision created by a Bladeless Trocar: A Novel Technique Greg J. Marchand, M.D., Katelyn M. Sainz MS1 From the National Foundation for Minimally Invasive Surgery (minvase.org), and Research and Development division of Marchand OBGYN PLLC Precis: Single Port Hysterectomy can be performed safely through a 12mm bladeless incision via this novel technique. Decreasing port size is continually pushing the limits of minimally invasive surgery for enhanced patient outcomes. Corresponding author: Greg J. Marchand M.D., Marchand OBGYN Research and Development, 1520 S. Dobson #218, Mesa, AZ 85202, Tel: 480-628-0566, Fax: 480-999-0801 ABSTRACT Study Objective: The aim of this study is to report the technique used by one surgeon performing a laparoscopic hysterectomy performed through a single 12mm bladeless incision. With the exception of pure vaginal hysterectomy we believe this technique is the least invasive technique published thus far to date where the hysterectomy is performed entirely abdominally. Design: Retrospective Analysis of Charts and Technique Setting: One private Hospital in the Southwest US Patients: 6 patients receiving single port hysterectomy between 2013 and 2014 Intervention: Single Port Laparoscopic Hysterectomy was performed with our ultra-minimally invasive technique, using a Covidien(C) 12mm bladeless laparoscopic trocar followed by an Olympus(C) TriPort device and Olypus(C) articulating 5mm laparoscope without in any way stretching or extending the 12mm port. Other novel aspects of our technique include placement of the single port at the bottom of the umbilicus regardless of patient BMI, the usage of intra-abdominal marcaine to help with postoperative pain and vaginal repair of colpotomy. -
Drug Administration Routes - Summary
Only Use L6. DrugCourse Administration & Transport 207 by Fluid Motion 243/CENG April 19, 2018 NANO Only Use Course 207 243/CENG Part I: Drug Administration NANO Routes of Drug Administration Only Topical: local effect, substanceUse is applied directly where its action is desired. EnteralCourse: systemic effect, substance is 207given via the gastrointestinal (GI) tract. Parenteral: systemic effect, substance is given by routes other than the gastrointestinal (GI) tract. 243/CENG NANO Topical Drug Delivery Epicutaneous – directly onto the surface of the skin Only allergy testing local anesthesia… Use Eye drops antibiotics for conjunctivitis … Course Inhalational207 asthma medications acute infection in upper airway … 243/CENG Intranasal route decongestant nasal sprays … NANO Enteral Drug Delivery Any form of administration that involves any part of the gastrointestinalOnly tract Use Course 207 Oral: Rectal: Gastric feeding tube: many drugs as tablets, various drugs in many drugs, enteral capsules, drops… suppository or enema nutrition… form… 243/CENG NANO Parenteral Drug Delivery Intravenous: into a vein (many drugs, total parenteral nutrition…) Only Intramuscular: into a muscle (many vaccines, antibiotics…) Use Subcutaneous: under the skin (insulin…) Intraarterial: into an artery (vasodilator drugs in the treatment of vasospasm…) Course Intradermal: into the skin itself (skin testing some allergens, tattoos…) 207 Transdermal: diffusion through the intact skin (transdermal opioid patches in pain management, nicotine patches for treatment -

Entry Techniques in Gynecologic Laparoscopy—A Review
Gynecol Surg (2012) 9:139–146 DOI 10.1007/s10397-011-0710-8 REVIEW ARTICLE Entry techniques in gynecologic laparoscopy—a review Johannes Ott & Agnes Jaeger-Lansky & Gunda Poschalko & Regina Promberger & Eleen Rothschedl & René Wenzl Received: 9 June 2011 /Accepted: 19 October 2011 /Published online: 13 November 2011 # Springer-Verlag 2011 Abstract Laparoscopy is one of the most common surgical underpowered in order to assess the risk for rare but life- procedures in gynecologic medicine. Major complications threatening complications. In conclusion, there is no solid associated with gynecologic laparoscopy are relatively rare, evidence proving the superiority of any method of with up to 50% related to laparoscopic entry. Several entry laparoscopic entry. techniques have been developed, all of which aim to provide a safe and easy entry to the abdominal cavity. In Keywords Laparoscopy. Entry techniques . Gynecology. this article, we aim to review the available evidence on Complications . Veress needle . Hasson technique . Direct laparoscopic entry techniques in gynecologic surgery. We trocar entry found no evidence that the Hasson (open) technique is superior to the Veress needle entry, the preferred method of most gynecologists all over the world. When entering the Background abdomen using the Veress needle, an intraperitoneal pressure <10 mmHg is a reliable predictor of correct Laparoscopy is one of the most common surgical intraperitoneal placement. Entry at Palmer’s point (left procedures in gynecologic medicine and has become upper quadrant laparoscopy) is recommended for patients the method of choice over the last few decades for with suspected or known periumbilical adhesions, or a treating benign diseases that require surgery [1, 2]. -

Effects of Intraoperative Insufflation with Warmed, Humidified CO2 During Abdominal Surgery: a Review
Annals of Original Article Coloproctology Ann Coloproctol 2018;34(3):125-137 pISSN 2287-9714 eISSN 2287-9722 https://doi.org/10.3393/ac.2017.09.26 www.coloproctol.org Effects of Intraoperative Insufflation With Warmed, Humidified CO2 during Abdominal Surgery: A Review Ju Yong Cheong1,2, Anil Keshava1, Paul Witting2, Christopher John Young1 1Colorectal Surgical Department, Concord Repatriation General Hospital, Sydney Medical School, The University of Sydney, Sydney; 2Discipline of Pathology, Charles Perkins Centre, Sydney Medical School, The University of Sydney, Sydney, Australia Purpose: During a laparotomy, the peritoneum is exposed to the cold, dry ambient air of the operating room (20°C, 0%– 5% relative humidity). The aim of this review is to determine whether the use of humidified and/or warmed CO2 in the intraperitoneal environment during open or laparoscopic operations influences postoperative outcomes. Methods: A review was performed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The PubMed, OVID MEDLINE, Cochrane Central Register of Controlled Trials and Embase databases were searched for articles published between 1980 and 2016 (October). Comparative studies on humans or nonhuman animals that involved randomized controlled trials (RCTs) or prospective cohort studies were included. Both laparotomy and laparoscopic studies were included. The primary outcomes identified were peritoneal inflammation, core body temperature, and postoperative pain. Results: The literature search identified 37 articles for analysis, including 30 RCTs, 7 prospective cohort studies, 23 human studies, and 14 animal studies. Four studies found that compared with warmed/humidified CO2, cold, dry CO2 resulted in significant peritoneal injury, with greater lymphocytic infiltration, higher proinflammatory cytokine levels and peritoneal adhesion formation. -

West Virginia Nerve Injury Slides
Anesthesia for Robotic Surgery: Is it a Different Ball Game? Michael A. Olympio, M.D. Professor of Anesthesiology Wake Forest University School of Medicine YES, it is… Access to, and monitoring the patient Combined Pneumoperitoneum and Trendelenburg – Type and amount of inflation gas – Pulmonary impairments – Hydrostatic gradients – Cardiovascular derangements – Circulation to the lower limb – Confounding obesity Anesthetic adjuncts and outcomes – Routine general anesthesia – General and regional? – Multimodal, narcotic-sparing, “ideal” anesthetic Olympio, MA. “Anesthetic Considerations for Robotic Urologic Surgery” In, Hemal AK, Menon M (eds.) Robotic Urologic Surgery. New York: Springer-Verlag, 2011. Photo of RALRP At the end of this lecture, the learner will explain or understand: – the physiological derangements associated with combined pneumoperitoneum and Trendelenburg posture – the relationships between, and significance of hydrostatic pressure, blood pressure measurement and the risks of organ hypo/hyper-perfusion – the reasons for choosing specific anesthetic management techniques and drugs. No disclosures. What you should know about your own surgical outcomes: operative time nausea and vomiting rates blood loss use of intermittent morbidity types and rates pneumatic serial compression (IPSC) length of stay and criteria for discharge desired extremes of TP mortality (if any and its desired intra-abdominal cause) inflation pressures (IAP) postoperative pain and and, type of inflation gas analgesic regimens Pre-Anesthetic -

Catheter Associated Urinary Tract Infection (CAUTI) Prevention
Catheter Associated Urinary Tract Infection (CAUTI) Prevention System CAUTI Prevention Team 1 Objectives At the end of this module, the participant will be able to: Identify risk factors for CAUTI Explain the relationship between catheter duration and CAUTI risk List the appropriate indications for urinary catheter insertion and continued use Implement evidence-based nursing practice to decrease the risk and incidence of CAUTI 2 The Problem All patients with an indwelling urinary catheter are at risk for developing a CAUTI. CAUTI increases pain and suffering, morbidity & mortality, length of stay, and healthcare costs. Appropriate indwelling catheter use can prevent about 400,000 infections and 9,000 deaths every year! (APIC, 2008; Gould et al, 2009) 3 2012 National Patient Safety Goal Implement evidence-based practices to prevent indwelling catheter associated urinary tract infections (CAUTI) Insert indwelling urinary catheters according to evidence-based guidelines Limit catheter use and duration Use aseptic technique for site preparation, equipment, and supplies (The Joint Commission (TJC), 2011) 4 2012 National Patient Safety Goal Manage indwelling urinary catheters according to evidence-based guidelines Secure catheters for unobstructed urine flow and drainage Maintain the sterility of the urine collection system Replace the urine collection system when required Collect urine samples using aseptic technique (TJC, 2011) 5 Sources of CAUTI Microorganisms Endogenous Meatal, rectal, or vaginal colonization Exogenous -
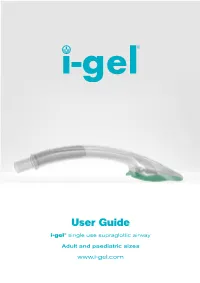
I-Gel User Guide
User Guide i-gel® single use supraglottic airway Adult and paediatric sizes www.i-gel.com Contents 1.0 Introduction .................................................................................................................... 2 1.1 The i-gel design ..................................................................................................................................................2 1.2 Key components and their function .........................................................................................................3 1.2.1 Soft non-inflatable cuff ................................................................................................................4 1.2.2 Gastric channel .............................................................................................................................4 1.2.3 Epiglottic rest ................................................................................................................................4 1.2.4 Buccal cavity stabiliser ................................................................................................................4 1.2.5 15mm connector ..........................................................................................................................5 1.2.6 Important key points.....................................................................................................................5 2.0 Indications ..................................................................................................................... -

Comparison Between Different Entry Techniques in Performing Pneumoperitoneum In10.5005/Jp-Journals-10033-1257 Laparoscopic Gynecological Surgery REVIEW ARTICLE
WJOLS Comparison between Different Entry Techniques in Performing Pneumoperitoneum in10.5005/jp-journals-10033-1257 Laparoscopic Gynecological Surgery REVIEW ARTICLE Comparison between Different Entry Techniques in Performing Pneumoperitoneum in Laparoscopic Gynecological Surgery Mandavi Rai ABSTRACT safety of one technique over another. However, the included studies are small and cannot be used to confirm safety of any Background: The main challenge facing the laparoscopic particular technique. No single technique or instrument has surgery is the primary abdominal access, as it is usually a blind been proved to eliminate laparoscopic entry-associated injury. procedure associated with vascular and visceral injuries. Lapa- Proper evaluation of the patient, supported by good surgical roscopy is a very common procedure in gynecology. Complica- skills and reasonably good knowledge of the technology of the tions associated with laparoscopy are often related to entry. instruments remain to be the cornerstone for safe access and The life-threatening complications include injury to the bowel, success in minimal access surgery. bladder, major abdominal vessels, and anterior abdominal- wall vessel. Other less serious complications can also occur, Keywords: Complications, Laparoscopy, Pnumoperitoneum, such as postoperative infection, subcutaneous emphysema Trocar. and extraperitoneal insufflation. There is no clear consensus as to the optimal method of entry into the peritoneal cavity. It How to cite this article: Rai M. Comparison between Dif- has been proved from studies that 50% of laparoscopic major ferent Entry Techniques in Performing Pneumoperitoneum complications occur prior to the commencement of the surgery. in Laparos copic Gynecological Surgery. World J Lap Surg The surgeon must have adequate training and experience in 2015;8(3):101-106. -

Use of the Veress Needle to Obtain Pneumoperitoneum Prior to Laparoscopy
Use of the Veress needle to obtain pneumoperitoneum prior to laparoscopy Consensus statement of the Royal Australian & New Zealand College of Obstetricians & Gynaecologists This statement has been developed by the Women’s (RANZCOG) and the Australasian Gynaecological Health Committee. It has been reviewed by the Endoscopy and Surgery Society (AGES). Endoscopic Surgery Advisory Committee (RANZCOG/AGES) and approved by the Objectives: To provide advice on the use of the RANZCOG Board and Council. Veress needle to obtain pneumoperitoneum prior to laparoscopy. A list of Women’s Health Committee and Endoscopic Surgery Advisory Committee Target audience: Health professionals providing (RANZCOG/AGES) Members can be found in gynaecological care, and patients. Appendix A. Values: The evidence was reviewed by the Disclosure statements have been received from all Endoscopic Surgery Advisory Committee members of this committee. (RANZCOG/AGES), and applied to local factors relating to Australia and New Zealand. Disclaimer This information is intended to provide Background: This statement was first developed by general advice to practitioners. This information Women’s Health Committee in April 1990 and most should not be relied on as a substitute for proper recently reviewed by the Endoscopic Surgery assessment with respect to the particular Committee (RANZCOG/AGES) in July 2017. circumstances of each case and the needs of any patient. This document reflects emerging clinical Funding: The development and review of this and scientific advances as of the date issued and is statement was funded by RANZCOG. subject to change. The document has been prepared having regard to general circumstances. First endorsed by RANZCOG: April 1990 Current: July 2017 Review due: July 2020 1 Table of contents Table of contents ............................................................................................................................ -

Download the Evonik for More Information!
ADVANCED APPROACHES THE PRESCRIPTION CAN WE ACHIEVE FOR DELAYED-RELEASE ABUSE EPIDEMIC: EFFECTIVE ORAL P04 FORMULATIONS P18 DESIGNING A SOLUTION P32 DELIVERY OF VACCINES? NOVEL ORAL DELIVERY SYSTEMS 77 O 2017 • ISSUE N 2017 TH JULY 17 JULY Contents o TH ONdrugDelivery Issue N 77, July 17 , 2017 Advanced Approaches for Delayed-Release Formulations Maria Montero Mirabet, Senior Project Manager, NOVEL ORAL DELIVERY SYSTEMS Drug Delivery Services, Business Line Health Care, and 4 - 9 Brigitte Skalsky, Senior Director, Scientific Communication, This edition is one in the ONdrugDelivery series Business Line Health Care of publications from Frederick Furness Publishing. Evonik Nutrition & Care Each issue focuses on a specific topic within the field of drug delivery, and is supported by industry Technologies & Clinical Studies for the Oral Delivery of Calcitonin Nozer Mehta, Principal leaders in that field. Peptide Technologies James P Gilligan, Chief Scientific Officer 12 MONTH EDITORIAL CALENDAR 10 - 16 Tarsa Therapeutics Sep Wearable Injectors William Stern, Consultant Peptide Drug Development Oct Prefilled Syringes Nov Pulmonary & Nasal Delivery The Prescription Abuse Epidemic: Designing a Solution Dec Connecting Drug Delivery Aia Malik, Healthcare Product Manager, and 18 - 20 Gemma Budd, Director of Technologies and Strategy Jan ‘18 Ophthalmic Delivery Lucideon Feb Prefilled Syringes Mar Skin Drug Delivery: Targeting the End Goal: Opportunities & Innovations in Colonic Drug Delivery Dermal, Transdermal & Microneedles Sejal R Ranmal, Director -

Ozone in Medicine. the Low-Dose Ozone Concept and Its Basic Biochemical Mechanisms of Action in Chronic Inflammatory Diseases
International Journal of Molecular Sciences Article Ozone in Medicine. The Low-Dose Ozone Concept and Its Basic Biochemical Mechanisms of Action in Chronic Inflammatory Diseases Renate Viebahn-Haensler 1,*,† and Olga Sonia León Fernández 2,*,† 1 Medical Society for the Use of Ozone in Prevention and Therapy, Iffezheim, D-76473 Baden-Baden, Germany 2 Pharmacy and Food Institute, University of Havana, Coronela, Lisa, Havana 10 400, Cuba * Correspondence: [email protected] (R.V.-H.); [email protected] (O.S.L.F.) † Both authors contributed equally. Abstract: Low-dose ozone acts as a bioregulator in chronic inflammatory diseases, biochemically char- acterized by high oxidative stress and a blocked regulation. During systemic applications, “Ozone peroxides” are able to replace H2O2 in its specific function of regulation, restore redox signaling, and improve the antioxidant capacity. Two different mechanisms have to be understood. Firstly, there is the direct mechanism, used in topical treatments, mostly via radical reactions. In systemic treatments, the indirect, ionic mechanism is to be discussed: “ozone peroxide” will be directly reduced by the glutathione system, informing the nuclear factors to start the regulation. The GSH/GSSG balance outlines the ozone dose and concentration limiting factor. Antioxidants are regulated, and in the case of inflammatory diseases up-regulated; cytokines are modulated, here downregulated. Rheumatoid Citation: Viebahn-Haensler, R.; arthritis RA as a model for chronic inflammation: RA, in preclinical and clinical trials, reflects the León Fernández, O.S. Ozone in pharmacology of ozone in a typical manner: SOD (superoxide dismutase), CAT (catalase) and finally Medicine. The Low-Dose Ozone GSH (reduced glutathione) increase, followed by a significant reduction of oxidative stress. -

Caring for Your Urinary (Foley) Catheter
Caring for Your Urinary (Foley) Catheter This information will help you care for your urinary (Foley) catheter while you’re at home. You have had a urinary catheter (a thin, flexible tube) placed in your bladder to drain your urine (pee). It’s held inside your bladder by a balloon filled with water. The parts of the catheter outside your body are shown in Figure 1. Catheter Care ● You need to clean your catheter, change your drainage bags, and wash your drainage bags every day. ● You may see some blood or urine around where the catheter enters your body, especially when walking or having a bowel movement. This is normal, as long as there’s urine draining into the drainage bag. If there’s not, call your healthcare provider. ● While you have your catheter, drink 1 to 2 glasses of liquids every 2 hours while you’re awake. ● Make sure that the catheter is in place in a tension free manner. The catheter should not be tight and should sit loosely. Showering ● You can shower while you have your catheter in place. Don’t take a bath until after your catheter is removed. ● Make sure you always shower with your night bag. Don’t shower with your leg bag. You may find it easier to shower in the morning. Cleaning Your Catheter You can clean your catheter while you’re in the shower. You will need the following supplies: 1. Gather your supplies. You will need: ○ Mild soap ○ Water 2. Wash your hands with soap and water for at least 20 seconds.