EAU Guidelines on Iatrogenic Trauma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urological Trauma
Guidelines on Urological Trauma D. Lynch, L. Martinez-Piñeiro, E. Plas, E. Serafetinidis, L. Turkeri, R. Santucci, M. Hohenfellner © European Association of Urology 2007 TABLE OF CONTENTS PAGE 1. RENAL TRAUMA 5 1.1 Background 5 1.2 Mode of injury 5 1.2.1 Injury classification 5 1.3 Diagnosis: initial emergency assessment 6 1.3.1 History and physical examination 6 1.3.1.1 Guidelines on history and physical examination 7 1.3.2 Laboratory evaluation 7 1.3.2.1 Guidelines on laboratory evaluation 7 1.3.3 Imaging: criteria for radiographic assessment in adults 7 1.3.3.1 Ultrasonography 7 1.3.3.2 Standard intravenous pyelography (IVP) 8 1.3.3.3 One shot intraoperative intravenous pyelography (IVP) 8 1.3.3.4 Computed tomography (CT) 8 1.3.3.5 Magnetic resonance imaging (MRI) 9 1.3.3.6 Angiography 9 1.3.3.7 Radionuclide scans 9 1.3.3.8 Guidelines on radiographic assessment 9 1.4 Treatment 10 1.4.1 Indications for renal exploration 10 1.4.2 Operative findings and reconstruction 10 1.4.3 Non-operative management of renal injuries 11 1.4.4 Guidelines on management of renal trauma 11 1.4.5 Post-operative care and follow-up 11 1.4.5.1 Guidelines on post-operative management and follow-up 12 1.4.6 Complications 12 1.4.6.1 Guidelines on management of complications 12 1.4.7 Paediatric renal trauma 12 1.4.7.1 Guidelines on management of paediatric trauma 13 1.4.8 Renal injury in the polytrauma patient 13 1.4.8.1 Guidelines on management of polytrauma with associated renal injury 14 1.5 Suggestions for future research studies 14 1.6 Algorithms 14 1.7 References 17 2. -

Product Catalog Stainless Steel Vaginal Specula
PRODUCT CATALOG STAINLESS STEEL VAGINAL SPECULA Graves Speculum Product No. Description LTL-GS300 Graves Speculum, Small 3” x .75” LTL-GS400 Graves Speculum, Medium 4” x 1.5” LTL-GS450 Graves Speculum, Large 4.50” x 1.5” LTL-GS700 Graves Speculum, XL 7” x 1.5” Pederson Speculum Product No. Description LTL-PS305 Pederson Speculum, Virginal 3” x .5” LTL-PS300 Pederson Speculum, Small 3” x 1” LTL-PS400 Pederson Speculum, Medium 4” x 1” LTL-PS450 Pederson Speculum, Large 4.5” x 1” LTL-PS455 Pederson Speculum, Extra Narrow 4.5” x .5” LTL-PS700 Pederson Speculum, XL 7” x 1” Open Sided Speculum Product No. Description LTL-WGR400 Weisman-Graves Speculum, Medium, Right Open 4” x 1.5” LTL-WGR450 Weisman-Graves Speculum, Large, Right Open 4.5” x 1.5” LTL-WGL400 Weisman-Graves Speculum, Medium, Left Open 4” x 1.5” LTL-WGL450 Weisman-Graves Speculum, Large, Left Open 4.5” x 1.5” LTL-WPR400 Weisman-Pederson Speculum, Medium, Right Open 4” x 1” LTL-WPR450 Weisman-Pederson Speculum, Large, Right Open 4.5” x 1” LTL-WPL400 Weisman-Pederson Speculum, Medium, Left Open 4” x 1” LTL-WPL450 Weisman-Prderspm Speculum, Large, Left Open 4.5” x 1” *We also offer wide view (4cm) and full view (7cm) openings. 1 | TOLL FREE 1 [800] 910-8303 FAX 1 [805] 579-9415 WWW.LTLMEDICAL.NET BIOPSY PUNCHES Standard Style Rotating Style Tischler [Morgan] 7mm x 3mm Baby Tischler 4mm x 2mm Tischler Kevorkian 9.5mm x 3mm Product No. Description Product No. Description Product No. -

Point-Of-Care Ultrasound to Assess Anuria in Children
CME REVIEW ARTICLE Point-of-Care Ultrasound to Assess Anuria in Children Matthew D. Steimle, DO, Jennifer Plumb, MD, MPH, and Howard M. Corneli, MD patients to stay abreast of the most current advances in medicine Abstract: Anuria in children may arise from a host of causes and is a fre- and provide the safest, most efficient, state-of-the-art care. Point- quent concern in the emergency department. This review focuses on differ- of-care US can help us meet this goal.” entiating common causes of obstructive and nonobstructive anuria and the role of point-of-care ultrasound in this evaluation. We discuss some indications and basic techniques for bedside ultrasound imaging of the CLINICAL CONSIDERATIONS urinary system. In some cases, as for example with obvious dehydration or known renal failure, anuria is not mysterious, and evaluation can Key Words: point-of-care ultrasound, anuria, imaging, evaluation, be directed without imaging. In many other cases, however, diagnosis point-of-care US can be a simple and helpful way to assess urine (Pediatr Emer Care 2016;32: 544–548) volume, differentiate urinary retention in the bladder from other causes, evaluate other pathology, and, detect obstructive causes. TARGET AUDIENCE When should point-of-care US be performed? Because this imag- ing is low-risk, and rapid, early use is encouraged in any case This article is intended for health care providers who see chil- where it might be helpful. Scanning the bladder first answers the dren and adolescents in acute care settings. Pediatric emergency key question of whether urine is present. -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -

Hemorrhagic Anuria with Acute Kidney Injury After a Single Dose of Acetazolamide: a Case Study of a Rare Side Effect
Open Access Case Report DOI: 10.7759/cureus.10107 Hemorrhagic Anuria With Acute Kidney Injury After a Single Dose of Acetazolamide: A Case Study of a Rare Side Effect Christy Lawson 1 , Leisa Morris 2 , Vera Wilson 3 , Bracken Burns Jr 4 1. Surgery, Quillen College of Medicine, East Tennesse State University, Johnson City, USA 2. Trauma, Ballad Health Trauma Services, Johnson City, USA 3. Pharmacy, Ballad Health Trauma Services, Johnson City, USA 4. Surgery, Quillen College of Medicine, East Tennessee State University, Johnson City, USA Corresponding author: Bracken Burns Jr, [email protected] Abstract Acetazolamide (ACZ) is a relatively commonly used medication in critical illness, glaucoma and altitude sickness. ACZ is sometimes used in the intensive care unit to assist with the treatment of metabolic alkalosis in ventilated patients. This is a case report of a patient who received two doses of ACZ, one week apart, for metabolic alkalosis and subsequently developed renal colic and dysuria that progressed to hemorrhagic anuria and acute kidney injury. This is an incredibly rare side effect of ACZ therapy, and has been reported in a few case reports in the literature, but usually is associated with a longer duration of therapy. This case resolved entirely within 24 hours with aggressive fluid therapy. Clinicians using ACZ therapy for any reason should be aware of this rare but significant side effect. Categories: Trauma Keywords: acetazolamide, hemorrhagic anuria, acute kidney injury Introduction Acetazolamide (ACZ) is a carbonic anhydrase inhibitor. It works to cause an accumulation of carbonic acid in the proximal kidney, preventing its breakdown, and causes lowering of blood pH and resorption of sodium, bicarbonate, and chloride with their subsequent excretion into the urine [1]. -

Current Current
CP_0406_Cases.final 3/17/06 2:57 PM Page 67 Current p SYCHIATRY CASES THAT TEST YOUR SKILLS Chronic enuresis has destroyed 12-year-old Jimmy’s emotional and social functioning. The challenge: restore his self-esteem by finding out why can’t he stop wetting his bed. The boy who longed for a ‘dry spell’ Tanvir Singh, MD Kristi Williams, MD Fellow, child® Dowdenpsychiatry ResidencyHealth training Media director, psychiatry Medical University of Ohio, Toledo CopyrightFor personal use only HISTORY ‘I CAN’T FACE MYSELF’ during regular checkups and refer to a psychia- immy, age 12, is referred to us by his pediatri- trist only if the child has an emotional problem J cian, who is concerned about his “frequent secondary to enuresis or a comorbid psychiatric nighttime accidents.” His parents report that he wets disorder. his bed 5 to 6 times weekly and has never stayed con- Once identified, enuresis requires a thorough sistently dry for more than a few days. assessment—including its emotional conse- The accidents occur only at night, his parents quences, which for Jimmy are significant. In its say. Numerous interventions have failed, including practice parameter for treating enuresis, the restricting fluids after dinner and awakening the boy American Academy of Child and Adolescent overnight to make him go to the bathroom. Psychiatry (AACAP)1 suggests that you: Jimmy, a sixth-grader, wonders if he will ever Take an extensive developmental and family stop wetting his bed. He refuses to go to summer history. Find out if the child was toilet trained and camp or stay overnight at a friend’s house, fearful started walking, talking, or running at an appro- that other kids will make fun of him after an acci- priate age. -

Overactive Bladder: What You Need to Know Whiteboard Animation Transcript with Shawna Johnston, MD and Emily Stern, MD
Obstetrics and Gynecology – Overactive Bladder: What You Need to Know Whiteboard Animation Transcript with Shawna Johnston, MD and Emily Stern, MD Overactive bladder (OAB) is a symptom-based disease state, which includes urinary frequency, nocturia, and urgency, with or without urgency incontinence. Symptoms of a urinary tract infection (UTI) are similar but additionally include dysuria (painful voiding) and hematuria. OAB tends to be a chronic progressive condition, while UTI symptoms are acute and may be associated with fever and malaise. In patients whose symptoms are unclear, urinalysis and urine culture may help rule out infection. If symptoms point to OAB, you should rule out: 1. Neurological disorders, such as multiple sclerosis, dementia, parkinson’s disease, and stroke. 2. Medical disorders such as diabetes, and 3. Prolapse, as women with obstructed voiding, usually from advanced prolapse, can have symptoms that mimic those of OAB. It is important to delineate how OAB symptoms affect a patient’s quality of life. Women with OAB are often socially isolated and sleep poorly. On history, pay attention to lifestyle factors such as caffeine and fluid intake, environmental triggers, and medications that may worsen symptoms like diuretics. Cognitive impairment and diabetes can influence OAB symptoms. Estrogen deficiency worsens OAB symptoms, so menopausal status and hormone use are important to note. Physical exam includes a screening sacral neurologic exam, an assessment for pelvic organ prolapse and a cough stress test to rule out stress urinary incontinence. On pelvic exam, look for signs of estrogen deficiency. Investigations include urinalysis, urine culture, and a post-void residual volume measurement. -
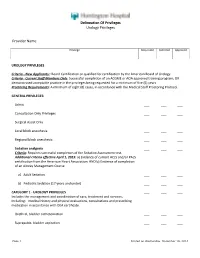
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -
Inhaltsverzeichnis Index Index Indice Alfabético Indice
Inhaltsverzeichnis Index Index Indice alfabético Indice Inhaltsverzeichnis Index Index Indice alfabético Indice E-01 Inhaltsverzeichnis Index Index Indice alfabético Indice A B Accessories for sterilization container ......... 88-38 to 88-41 BABCOCK seizing forceps ........................................ 64-02 Adenotome LAFORCE .............................................. 46-19 BABINSKY percussion hammer ............................... 02-07 ADLERKREUTZ thumb and tissue forceps ............... 10-04 BACKHAUS-CLIP tube holder towel clamp .............. 14-03 ADSON BABY hemostatic forceps ............................ 12-09 BACKHAUS KOCHER towel clamp .......................... 14-02 ADSON-Baby retractor .............................................. 18-15 BACKHAUS towel clamp ........................................... 14-02 ADSON BAGGISH uterine biopsy specimen forceps ............. 70-45 bone rongeur ........................................................ 32-03 BAILEY-BABY rib contractor ..................................... 56-18 ADSON-BROWN thumb and tissue forceps ............. 10-03 BAILEY-GIBBON rib contractor ................................. 56-18 ADSON BAILEY rib contractor ............................................... 56-18 elevator ................................................................. 32-21 BAINBRIDGE hemostatic forceps ............................................... 12-09 atraumatic forceps ................................................ 13-09 hypophyseal forceps ............................................ -

Topic Objectives Physical Examination
LECTURE MODULE 3; PHYSICAL EXAMINATION OF URINE Topic Objectives 1. Identify the colors which commonly associated with abnormal urine. 2. State two possible causes for urine turbidity in a sample that is not fresh. 3. Identify possible causes for abnormal urinary foam. 4. Identify the odors commonly associated with abnormal urine. 5. Differentiate between the following abnormalities of urine volume: Polyuria Oliguria Anuria Nocturia 6. Define specific gravity of urine. 7. Define refractive index of a solution. 8. Identify possible causes of abnormal specific gravities of urine. 9. Compare and contrast Diabetes Mellitus with Diabetes Insipidus. Physical Examination Appearance Color Transparency Foam Odor Specific Gravity Volume 1 Color • When an examiner first receives a urine specimen, color is observed and recorded. • Normal urine usually ranges from a light yellow to a dark amber color. • The normal metabolic products which are excreted from the body contribute to this color. • Urochrome is the chief urinary pigment. • Urinary color may vary, depending on concentration, dietary pigments, drugs, metabolites, and the presence or absence of blood. • A pale color generally indicates dilute urine with low specific gravity. • Occasionally, a pale urine with high specific gravity is seen in a diabetic patient. Color In many diseases, urinary color may drastically change. In liver disease, bile pigments may produce a yellow-brown or greenish tinge in the urine. Pink, red, or brown urine usually indicates the presence of blood, but porphyrins may also cause a pink or red urine. Since drugs, dyes and certain foods may alter urine color, the patient’s drug list and diet intake should be checked. -

Prof.Dr. S.Mohamed Musthafa
PROF.DR. S.MOHAMED MUSTHAFA M.B.B.S., M.S(GEN.SURGERY) D.L.O (ENT) FAIS.,FICS.,FACRSI., PROFESSOR OF SURGERY S.R.M. MEDICAL COLLEGE AND RESEARCH CENTRE KATTANKULATHUR – 603 203 INJURIES TO THE MALE URETHRA ANATOMY OF URETHRA TUBULAR PASSAGE EXTEND: NECK OF BLADDER TO EXT. URETHRAL MEATUS O 20 CM O 3.75 CM MALE URETHRA 3 PARTS PROSTATIC PART (3.1 CM) MEMBRANEOUS PART 1.25 CM 1.9 CM SPONGY PART 15 CM BLOOD SUPPLY: ARTERIES TO BULB Br OF INTERNAL PUDENTAL A NERVE SUPPLY PERINEAL Br OF PUDENDAL NERVE INJURIES TO THE MALE URETHRA y RUPTURE OF THE BULBAR URETHRA y RUPTURE OF THE MEMBRANOUS URETHRA RUPTURE OF THE BULBAR URETHRA CAUSE y FALL ASTRIDE PROJECTING OBJECT CYCLING ACCIDENTS y LOOSE MANHOLE COVERS y GYMMNASIUM ACCIDENTS y WORKERS LOSING THEIR FOOTING CLINICAL FEATURES SIGNS y RETENTION OF URINE y PERINEAL HAEMATOMA – SWELLING y BLEEDING FROM EXT.URINARY MEATUS. ASSESSMENT ANALGESIC IF SUSPECTED RUPTURE – DISCOURAGE URETHRA FROM PASSING URINE. FULL BLADDER – PERCUTANEOUS SUPRAPUBIC SPC CATHETER DRAINAGE IF PT. ALREADY PASSED URINE WHEN FIRST SEEN NO EXTRAVASATION PARTIAL URETHRAL RUPTURE SPC NOT NEEDED TREATMENT AVOID INJUDICIOUS CATHETERISATION IT WILL CONVERT PARTIAL TEAR COMPLETE TRANSECTION ASSESS URETHRAL INJURY ASCENDING URETHROGRAM WITH WATER BASED CONTRAST FLEXIBLE CYSTOSCOPY NO FACILITIES FOR SPC VERY OCCASIONALLY TRY TO PASS SOFF, SMALL CALIBRE CATHETER WITHOUT FORCE. COMPLETE URETHRAL TEAR SPC – ARRANGE FOR REPAIR SOME SURGEONS – EARLY INTERVENSION EARLY OPEN REPAIR EARLY REPAIR EXCISION OF TRAUMATISED SECTION AND SPATULATED END TO END REANASTAMOSIS OF URETHRA. OTHER SURGEONS WAIT LONGER FOR REPAIR USING URETHROSCOPE TO FIND WAY ACROSS GAP IN URETHRA WAIT LONGER y ALLOWS URETHRAL CATHETER TO BE PLACED y ENDS OF URETHRA ARE ALIGNED HEALING OCCUR COMPLICATION IF THE PT. -

Dysuria White Paper
CASE STUDY SUMMARY Management of Dysuria for BPH Surgical Procedures Ricardo Gonzalez, M.D. Medical Director of Voiding Dysfunction at Houston Metro Urology, Houston, Texas Dysuria following Benign Prostatic approach, concentrating on one area without Hyperplasia (BPH) Procedures ‘jumping around.’ Keep the laser at .5 mm away from the tissue when using the GreenLight PV® Transient dysuria following surgical treatment system; and 3 mm or less for the GreenLight of benign prostatic hyperplasia (BPH) is not an HPS® and GreenLight XPS® systems. Care must uncommon occurrence regardless of treatment. also be taken at the bladder neck: Identify Many factors may contribute to dysuria after the UOs and trigone, use lower power these procedures, including irritation from the (60-80 watts) and avoid directing energy introduction of the cystoscope; the degree of into the bladder.” tissue necrosis; the surgical modality utilized; the surgical technique employed; and the patient’s condition. This paper will focus on Pre-and Post-Operative Management both pre-procedural as well as post-procedural of Dysuria management of irritative symptoms related to Dr. Ricardo Gonzalez is an expert in the surgical BPH procedures. treatment of BPH with the GreenLight Laser System. “I spend considerable time Contributors to Dysuria educating patients on what to expect after Ricardo Gonzalez, M.D., Medical Director of surgical treatment of BPH, including dysuria,” Voiding Dysfunction at Houston Metro Urology says Dr. Gonzalez. “Proper patient education states, “Inefficient surgical technique can encour- will prevent many unnecessary phone calls age coagulative necrosis, which may increase from patients.” inflammation. This is more likely to be the case Dr.