Urological Trauma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ultrasonography and Elastography Imaging
Jemds.com Case Report Post Traumatic Hematocele - Ultrasonography and Elastography Imaging Shivesh Pandey1, Suresh Vasant Phatak2, Gopidi Sai Nidhi Reddy3, Apoorvi Bharat Shah4 1, 2, 3, 4 Department of Radio diagnosis, Jawaharlal Nehru Medical College, Sawangi (Meghe), Wardha, Maharashtra India. INTRODUCTION Hematocele with blunt scrotal trauma is an uncommon cause of the testicular pain. Corresponding Author: Elastography is the new recent advance in the field of ultrasound. USG and Dr. Suresh Vasant Phatak, elastography findings of the acute hematocele is described in this aricle. Department of Radiodiagnosis, Jawaharlal Testicular trauma is the third most common cause of acute scrotal pain,1 and Nehru Medical College, Sawangi (Meghe), high-frequency ultrasonography (USG) with a linear array transducer is the first Wardha, Maharashtra – 442001, India. E-mail: [email protected] preferred modality for testicular trauma evaluation. Extra testicular haematoceles or blood collections inside the tunica vaginalis are the most common findings in the DOI: 10.14260/jemds/2021/340 scrotum after blunt injury.2 On clinical assessment, haematocele appears as a hard mass like swelling and causes pain in the scrotum. In the majority of cases, How to Cite This Article: spontaneous resolution occurs with the support of conservative therapy,3 even if Pandey S, Phatak SV, Reddy GSN, et al. Post treated conservatively, may result in infection, discomfort, or atrophy in undiagnosed traumatic hematocele - usg and broad hematoceles and testicular hematomas over time.4 elastography imaging. J Evolution Med A testis with its coverings, epididymis, and spermatic cord are all contained in Dent Sci 2021;10(21):1636-1638, DOI: 10.14260/jemds/2021/340 each hemiscrotum. -

Renal Ultrasonography
The American Society of Diagnostic and Interventional Nephrology Application for Certification Renal Ultrasonography Revised 10/5/10 The American Society of Diagnostic and Interventional Nephrology Application for Certification Renal Ultrasonography This application packet is composed of several parts: • Requirements for certification • Form for documentation of completion of basic requirements • Application form Checklist (check all that are included with application) Completed application form Documentation of didactic training Documentation of supervised studies Documentation of completion of basic requirements form Set of studies with follow-up Set of sample studies (Please label cases to reflect IB(3) or IIC of the application. Peer reference letter Application fee ($500/members or $750/non-members effective 1/1/08) *Non-member fee includes ASDIN membership for remainder of membership year from date of certification application. Basis for certification (check one) Nephrology fellowship based training program CME - accredited training program Other Certification requested (check one) General certification in renal ultrasonography Certification in renal transplantation ultrasonography Two copies of the application and all documentation should be submitted to the ASDIN office. Copies should be one of the following: a) two paper copies, OR b) one paper copy and one cd rom copy, OR c) one paper copy and one copy sent electronically to [email protected] Mail all application materials to: The American Society of Diagnostic and Interventional Nephrology Attn: Bertinna Dubra 134 Fairmont Street, Suite B Clinton, MS 39056 Revised 10/5/10 2 American Society of Diagnostic and Interventional Nephrology Requirements for Certification in Renal Ultrasonography I. Certification of nephrologists to perform and interpret sonograms of the kidney and bladder. -
Renal Relevant Radiology: Use of Ultrasonography in Patients with AKI
Renal Relevant Radiology: Use of Ultrasonography in Patients with AKI Sarah Faubel,* Nayana U. Patel,† Mark E. Lockhart,‡ and Melissa A. Cadnapaphornchai§ Summary As judged by the American College of Radiology Appropriateness Criteria, renal Doppler ultrasonography is the most appropriate imaging test in the evaluation of AKI and has the highest level of recommendation. Unfortunately, nephrologists are rarely specifically trained in ultrasonography technique and interpretation, and *Division of Internal Medicine, Nephrology, important clinical information obtained from renal ultrasonography may not be appreciated. In this review, the University of Colorado strengths and limitations of grayscale ultrasonography in the evaluation of patients with AKI will be discussed and Denver Veterans with attention to its use for (1) assessment of intrinsic causes of AKI, (2) distinguishing acute from chronic kidney Affairs Medical Center, 3 Denver, Colorado; diseases, and ( ) detection of obstruction. The use of Doppler imaging and the resistive index in patients with † AKI will be reviewed with attention to its use for (1) predicting the development of AKI, (2) predicting the Department of 3 Radiology and prognosis of AKI, and ( ) distinguishing prerenal azotemia from intrinsic AKI. Finally, pediatric considerations in §Department of Internal the use of ultrasonography in AKI will be reviewed. Medicine and Clin J Am Soc Nephrol 9: 382–394, 2014. doi: 10.2215/CJN.04840513 Pediatrics, Nephrology, University of Colorado Denver, Denver, Colorado; and Introduction structures on ultrasonography images. The renal cap- ‡Department of Renal ultrasonography is typically the most appro- sule consists of thin fibrous tissue, which is next to Radiology, University of priate and useful radiologic test in the evaluation of fat, and thus the kidney often appears to be surroun- Alabama at Birmingham, patients with AKI (1). -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -
Guidelines on Urological Trauma
European Association of Urology GUIDELINES ON UROLOGICAL TRAUMA D. Lynch, L. Martinez-Piñeiro, E. Plas, E. Serafetinidis, L. Turkeri, M. Hohenfellner FEBRUARY 2003 TABLE OF CONTENTS PAGE 1. RENAL TRAUMA 5 1.1 Background 5 1.2 Mode of injury 5 1.2.1 Injury classification 5 1.3 Diagnosis: initial emergency assessment 6 1.3.1 History and physical examination 6 1.3.1.1 Guidelines on history and physical examination 7 1.3.2 Laboratory evaluation 7 1.3.2.1 Guidelines on laboratory evaluation 7 1.3.3 Imaging: criteria for radiographic assessment 7 1.3.3.1 Ultrasonography 7 1.3.3.2 Intravenous pyelography (IVP) 8 1.3.3.3 Computed tomography (CT) 8 1.3.3.4 Magnetic resonance imaging (MRI) 9 1.3.3.5 Angiography 9 1.3.3.6 Guidelines on radiographic assessment 9 1.4 Treatment 9 1.4.1 Indications for renal exploration 9 1.4.2 Operative findings and reconstruction 10 1.4.3 Non-operative management of renal injuries 10 1.4.4 Guidelines on management of renal trauma 11 1.4.5 Post-operative care and follow-up 11 1.4.5.1 Guidelines on post-operative management and follow-up 11 1.4.6 Complications 11 1.4.6.1 Guidelines on management of complications 12 1.4.7 Paediatric renal trauma 12 1.4.7.1 Guidelines on management of paediatric trauma 13 1.4.8 Renal trauma in the polytrauma patient 13 1.4.8.1 Guidelines on management of polytrauma with associated renal injury 13 1.5 Suggestions for future research studies 13 1.6 Algorithms 13 1.7 References 15 2. -

Ultrasound Evaluation of Testicular Vein
[Downloaded free from http://www.njcponline.com on Monday, July 6, 2020, IP: 197.90.36.231] Original Article Ultrasound Evaluation of Testicular Vein Diameter in Suspected Cases of Varicocele: Comparison of Measurements in Supine and Upright Positions UR Ebubedike, SU Enukegwu1, AM Nwofor2 Department of Radiology, Background: Scrotal ultrasonography has high sensitivity in the detection Nnamdi Azikiwe University of intra‑scrotal abnormalities. Various ultrasonographic parameters such as Teaching Hospital, NAUTH Nnewi, 1St Bridget’s the spermatic cord diameter, venous diameter, and venous retrograde flow in Xray Centre Benin City, either supine or upright positions with or without Valsalva maneuver have been 2Depatment of Surgery, Abstract investigated to assess patients suspected of having varicocele. Aims: This study Nnamdi Azikiwe University aimed at comparing testicular vein diameter in supine and upright positions using Teaching Hospital, NAUTH, ultrasonography. Methodology: This is a prospective multicenter study conducted Nnewi, Nigeria between September 2018 and June 2019. Eighty‑two consenting suspected cases of varicocele, 20 years and above, referred for scrotal ultrasonography were included in this study. Results: The study population had a mean age of 42.9 + 14.89 (SD) with a range of 20–96 years. The highest number of participants fell within the age range of 30–39 years 23 (28%). Varicocele was demonstrated in 96.3% of the patients. More patients showed sonographic evidence of varicocele in the upright position, on the right 50 (61%) as well as left 50 (61%). Bilateral varicocele had a higher frequency in the upright position 45 (54.9%), while supine was 23 (28%). Upright position had the widest diameter in 72% of participants on the right and 82% on the left. -
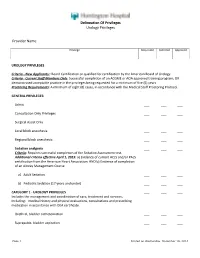
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

Common and Uncommon Presentation of Fluid Within the Scrotal Spaces
THIEME E34 Review Common and Uncommon Presentation of Fluid within the Scrotal Spaces Authors V. Patil, S. M. C. Shetty, S. Das Affiliation Radiodiagnosis, JSS Medical College, Mysore, India Key words Abstract gin. US may suggest a specific diagnosis for a ●▶ US wide variety of intrascrotal cystic and fluid ▶ ▼ ● ultrasonography Ultrasonography(US) of the scrotum has been lesions and appropriately guide therapeutic ●▶ fluid demonstrated to be useful in the diagnosis of options. The paper reviews the current knowl- ●▶ testis ●▶ scrotum fluid in the scrotal sac. Grayscale US character- edge of ultrasound in conditions with fluid in the izes the lesions as testicular or extratesticular testis and scrotum. The review presents the and, with color Doppler, power Doppler and applications of ultrasonography in the diagnosis pulse Doppler, any perfusion can also be assessed. of hydrocele, testicular cysts, epididymal cysts, Cystic or encapsulated fluid collections are rela- spermatoceles, tubular ectasia, hernia and hema- tively common benign lesions that usually pre- toceles. The aim of this paper is to provide a pic- sent as palpable testicular lumps. Most cysts torial review of the common and uncommon arise in the epidydimis, but all anatomical struc- presentation of fluid within the scrotal spaces. tures of the scrotum can be the site of their ori- Introduction images with portions of each testis on the same ▼ image should be ideally acquired in grayscale and Scrotal conditions associated with fluid can be color Doppler modes. The structures within the received 21.01.2015 accepted 29.06.2015 broadly classified as fluid in scrotal sac, testicular scrotal sac are examined to detect extra testicu- cysts, epididymal cysts and inguinoscrotal hernia. -

A Systematic Review of Graft Augmentation Urethroplasty Techniques for the Treatment of Anterior Urethral Strictures
EUROPEAN UROLOGY 59 (2011) 797–814 available at www.sciencedirect.com journal homepage: www.europeanurology.com Review – Reconstructive Urology A Systematic Review of Graft Augmentation Urethroplasty Techniques for the Treatment of Anterior Urethral Strictures Altaf Mangera *, Jacob M. Patterson, Christopher R. Chapple Royal Hallamshire Hospital, Sheffield, United Kingdom Article info Abstract Article history: Context: Reconstructive surgeons who perform urethroplasty have a variety of Accepted February 2, 2011 techniques in their armamentarium that may be used according to factors such as Published online ahead of aetiology, stricture position, and length. No one technique is recommended. print on February 11, 2011 Objective: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. Keywords: Evidence acquisition: We performed an updated systematic review of the Medline Augmentation urethroplasty literature from 1985 to date and classified the data according to the site of surgery Anterior urethral stricture and technique used. Data are also presented on the type of graft used and the Bulbar urethroplasty follow-up methodology used by each centre. Dorsal onlay bulbar Evidence synthesis: More than 2000 anterior urethroplasty procedures have been urethroplasty describedinthe literature.Whenconsidering the bulbar urethra there isnosignificant Ventral onlay bulbar difference between the average success rates of the dorsal and the ventral onlay urethroplasty procedures, 88.4% and 88.8% at42.2 and 34.4 moin 934 and 563 patients,respectively. Penile urethroplasty The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. -

Technical Report—Diagnosis and Management of an Initial UTI in Febrile Infants and Young Children
FROM THE AMERICAN ACADEMY OF PEDIATRICS Technical Report—Diagnosis and Management of an Initial UTI in Febrile Infants and Young Children S. Maria E. Finnell, MD, MS, Aaron E. Carroll, MD, MS, Stephen M. Downs, MD, MS, and the Subcommittee on abstract Urinary Tract Infection OBJECTIVES: The diagnosis and management of urinary tract infec- KEY WORDS tions (UTIs) in young children are clinically challenging. This report was urinary tract infection, infants, children, vesicoureteral reflux, voiding cystourethrography, antimicrobial, prophylaxis, developed to inform the revised, evidence-based, clinical guideline re- antibiotic prophylaxis, pyelonephritis garding the diagnosis and management of initial UTIs in febrile infants ABBREVIATIONS and young children, 2 to 24 months of age, from the American Academy UTI—urinary tract infection of Pediatrics Subcommittee on Urinary Tract Infection. VUR—vesicoureteral reflux VCUG—voiding cystourethrography METHODS: The conceptual model presented in the 1999 technical re- CI—confidence interval port was updated after a comprehensive review of published litera- RR—risk ratio ture. Studies with potentially new information or with evidence that RCT—randomized controlled trial LR—likelihood ratio reinforced the 1999 technical report were retained. Meta-analyses on SPA—suprapubic aspiration the effectiveness of antimicrobial prophylaxis to prevent recurrent UTI This document is copyrighted and is property of the American were performed. Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American RESULTS: Review of recent literature revealed new evidence in the Academy of Pediatrics. Any conflicts have been resolved through following areas. Certain clinical findings and new urinalysis methods a process approved by the Board of Directors. -

(Part 1): Management of Male Urethral Stricture Disease
EURURO-9412; No. of Pages 11 E U R O P E A N U R O L O G Y X X X ( 2 0 2 1 ) X X X – X X X ava ilable at www.sciencedirect.com journa l homepage: www.europeanurology.com Review – Reconstructive Urology European Association of Urology Guidelines on Urethral Stricture Disease (Part 1): Management of Male Urethral Stricture Disease a, b c d Nicolaas Lumen *, Felix Campos-Juanatey , Tamsin Greenwell , Francisco E. Martins , e f a c g Nadir I. Osman , Silke Riechardt , Marjan Waterloos , Rachel Barratt , Garson Chan , h i a j Francesco Esperto , Achilles Ploumidis , Wesley Verla , Konstantinos Dimitropoulos a b Division of Urology, Gent University Hospital, Gent, Belgium; Urology Department, Marques de Valdecilla University Hospital, Santander, Spain; c d Department of Urology, University College London Hospital, London, UK; Department of Urology, Santa Maria University Hospital, University of Lisbon, e f Lisbon, Portugal; Department of Urology, Sheffield Teaching Hospitals, Sheffield, UK; Department of Urology, University Medical Center Hamburg- g h Eppendorf, Hamburg, Germany; Division of Urology, University of Saskatchewan, Saskatoon, Canada; Department of Urology, Campus Biomedico i j University of Rome, Rome, Italy; Department of Urology, Athens Medical Centre, Athens, Greece; Aberdeen Royal Infirmary, Aberdeen, UK Article info Abstract Article history: Objective: To present a summary of the 2021 version of the European Association of Urology (EAU) guidelines on management of male urethral stricture disease. Accepted May 15, 2021 Evidence acquisition: The panel performed a literature review on these topics covering a time frame between 2008 and 2018, and used predefined inclusion and exclusion criteria Associate Editor: for the literature to be selected. -

Incidental Findings General Medical Ultrasound Examinations: Management and Diagnostic Pathways Guidance
w Incidental Findings General Medical Ultrasound Examinations: Management and Diagnostic Pathways Guidance September 2020 Acknowledgements The British Medical Ultrasound Society (BMUS) would like to acknowledge the work and assistance provided by the following in the production of this guideline: The Professional Standards Group BMUS 2019-2020: Chair: Mrs Catherine Kirkpatrick Consultant Sonographer Professor (Dr.) Rhodri Evans BMUS President. Consultant Radiologist Mrs Pamela Parker BMUS President Elect. Consultant Sonographer Dr Peter Cantin PhD. Consultant Sonographer Dr Oliver Byass. Consultant Radiologist Miss Alison Hall Consultant Sonographer Mrs Hazel Edwards Sonographer Mr Gerry Johnson Consultant Sonographer Dr. Mike Smith PhD. Physiotherapist/Senior Lecturer Professor (Dr.) Adrian Lim, Consultant Radiologist In addition, the documentation and protocol evidence from Hull University Teaching Hospitals NHS Trust, Plymouth NHS Trusts and United Lincolnshire Hospitals NHS Trust for template derivation. Foreword The introduction of this guidance document regarding the diagnosis and management of incidental findings is timely. The changing landscapes of ultrasound practice combined with the significant communication challenges within a variety of referral sources can often add to the pressures exerted on the ultrasound practitioner. The demand for diagnostic ultrasound examinations is ever increasing. Faster patient throughput and increasing complexities of patient management, coupled with advancing ultrasound technologies leads to an inevitable increase in ‘incidentalomas’. The challenges facing ultrasound practitioners include the re-definition of ‘normal’ due to increased resolution of imaging, dilemmas around reporting of incidental findings and managing the effects of this for the patients and the referring clinicians. These guidelines are a resource that can be used as a basis for diagnostic pathways and reporting protocols, and can be modified as appropriate to align with locally agreed protocols.