Urology Services in the ASC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urology 1 Cystoscopes
Urology 1 Cystoscopes 2 Urethrotomes 3 Resectoscopes 4 Uretero-Renoscopes 5 Nephroscopes 6 Lithotripsy (UreTron) 7 Laser Therapy 8 Small Caliber 9 Fluid Management 10 Accessories Richard Wolf Medical Instruments Corporation assumes no responsibility or liability for any errors or omissions in the content of this catalog. The information contained in this catalog is provided on an “as is” basis with no guarantees of completeness, accuracy, usefulness, or timeliness, and without warranties of any kind whatsoever, expressed or implied. 1777- 02.01-1118USA Cysto-Urethroscopes 8650 E-line design CYSTOSCOPES The E-line design guarantees optimum handling and safe, fatigue-free operation as well as a wide range of possible combinations. Basic Set for Cystoscopy Cysto-urethroscope sheath, 19.5 Fr. with obturator 8650.0341 Adapter with 1 instrument port 8650.264 Insert with Albarran deflector, 2 instrument ports 8650.204 Sterile universal sealing valve (pack of 5) 4712348 Viewing obturator 8650.724 Biopsy forceps Marburg 8650.614 Grasping forceps 8650.684 PANOVIEW telescope, 0° 8650.414 PANOVIEW telescope, 70° 8650.415 Otis urethrotome 8517.00 822.31 822.13 822.31 Flexible connector 822.13 Tray 8585030 1777- 02.01-1118USA 2 PANOVIEW Telescopes Overview CYSTOSCOPES Ø Viewing direction Color code Application mm 0° blue Standard 4 8650.414 12° orange Standard 4 8654.431 Standard 4 8654.422 30° red Long sheath 4 8668.433* 70° yellow Standard 4 8650.415 * Only 25° available. 1777- 02.01-1118USA 3 Cysto-Urethroscope 8650 for telescope 4 mm, 0°, 12°, 30°, 70° and adapters CYSTOSCOPES Sheaths and obturators Adapters Sheath incl. -

Cystoscopy to Understand a Cystoscopy, It Is Helpful to Become Familiar with the Urinary System (Figure 1)
Northwestern Memorial Hospital Patient Education TESTS AND PROCEDURES Cystoscopy To understand a cystoscopy, it is helpful to become familiar with the urinary system (Figure 1). The system’s main purpose is to remove urinary waste products from your body. Urine is produced by the kidneys, moves through the ureters and is stored in the bladder. The bladder is a balloon-like organ that stores urine. The urethra is the tube that carries urine from the bladder out of your body. If you have Figure 1. Urinary system any questions or concerns, Kidneys please ask your physician or nurse. Ureters Bladder Urethra A cystoscopy is a procedure that allows your physician to look at the inside of your urethra and bladder. A telescope-like instrument called a cystoscope is passed through your urethra into your bladder. During the procedure, your physician may also do the following, as needed: ■ Remove stones from your bladder or ureters ■ Place or remove a ureteral stent ■ Insert medication into your bladder ■ Remove small pieces of tissue for testing (biopsy) from your urinary tract A cystoscopy may be done in a physician’s office or in the hospital’s operating room (OR). Your physician will discuss which option is best for you. Preparation and procedure If the test is done in the OR, you will be asked to sign a written consent. The OR procedure and any special preparation will be explained to you. There may be some discomfort during the examination. Some patients may require sedation or anesthesia. Depending on the type of medication used for your procedure, you will be told if you need to stop eating and drinking before your procedure. -

Urological Trauma
Guidelines on Urological Trauma D. Lynch, L. Martinez-Piñeiro, E. Plas, E. Serafetinidis, L. Turkeri, R. Santucci, M. Hohenfellner © European Association of Urology 2007 TABLE OF CONTENTS PAGE 1. RENAL TRAUMA 5 1.1 Background 5 1.2 Mode of injury 5 1.2.1 Injury classification 5 1.3 Diagnosis: initial emergency assessment 6 1.3.1 History and physical examination 6 1.3.1.1 Guidelines on history and physical examination 7 1.3.2 Laboratory evaluation 7 1.3.2.1 Guidelines on laboratory evaluation 7 1.3.3 Imaging: criteria for radiographic assessment in adults 7 1.3.3.1 Ultrasonography 7 1.3.3.2 Standard intravenous pyelography (IVP) 8 1.3.3.3 One shot intraoperative intravenous pyelography (IVP) 8 1.3.3.4 Computed tomography (CT) 8 1.3.3.5 Magnetic resonance imaging (MRI) 9 1.3.3.6 Angiography 9 1.3.3.7 Radionuclide scans 9 1.3.3.8 Guidelines on radiographic assessment 9 1.4 Treatment 10 1.4.1 Indications for renal exploration 10 1.4.2 Operative findings and reconstruction 10 1.4.3 Non-operative management of renal injuries 11 1.4.4 Guidelines on management of renal trauma 11 1.4.5 Post-operative care and follow-up 11 1.4.5.1 Guidelines on post-operative management and follow-up 12 1.4.6 Complications 12 1.4.6.1 Guidelines on management of complications 12 1.4.7 Paediatric renal trauma 12 1.4.7.1 Guidelines on management of paediatric trauma 13 1.4.8 Renal injury in the polytrauma patient 13 1.4.8.1 Guidelines on management of polytrauma with associated renal injury 14 1.5 Suggestions for future research studies 14 1.6 Algorithms 14 1.7 References 17 2. -

Testosterone Replacement Therapy Is Associated with an Increased Risk of Urolithiasis
World Journal of Urology (2019) 37:2737–2746 https://doi.org/10.1007/s00345-019-02726-6 ORIGINAL ARTICLE Testosterone replacement therapy is associated with an increased risk of urolithiasis Tyler R. McClintock1 · Marie‑Therese I. Valovska2 · Nicollette K. Kwon3 · Alexander P. Cole1,3 · Wei Jiang3 · Martin N. Kathrins1 · Naeem Bhojani4 · George E. Haleblian1 · Tracey Koehlmoos5 · Adil H. Haider3,6 · Shehzad Basaria7 · Quoc‑Dien Trinh1,3 Received: 16 November 2018 / Accepted: 7 March 2019 / Published online: 23 March 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose To determine whether TRT in men with hypogonadism is associated with an increased risk of urolithiasis. Methods We conducted a population-based matched cohort study utilizing data sourced from the Military Health System Data Repository (a large military-based database that includes benefciaries of the TRICARE program). This included men aged 40–64 years with no prior history of urolithiasis who received continuous TRT for a diagnosis of hypogonadism between 2006 and 2014. Eligible individuals were matched using both demographics and comorbidities to TRICARE enrollees who did not receive TRT. The primary outcome was 2-year absolute risk of a stone-related event, comparing men on TRT to non-TRT controls. Results There were 26,586 pairs in our cohort. Four hundred and eighty-two stone-related events were observed at 2 years in the non-TRT group versus 659 in the TRT group. Log-rank comparisons showed this to be a statistically signifcant dif- ference in events between the two groups (p < 0.0001). This diference was observed for topical (p < 0.0001) and injection (p = 0.004) therapy-type subgroups, though not for pellet (p = 0.27). -

Native Kidney Biopsy
Mohammed E, et al., J Nephrol Renal Ther 2020, 6: 034 DOI: 10.24966/NRT-7313/100034 HSOA Journal of Nephrology & Renal Therapy Review Article Native Kidney Biopsy: An Introduction The burden of non communicable diseases has been a worldwide Update and Best Practice public health challenge, as chronic diseases compose 61% of global deaths and 49% of the global burden of diseases. Currently, many Evidence countries are encountering a fast transformation in the disease pro- file from first generation diseases such as infectious diseases to the encumbrance of non communicable diseases. In addition, Chronic Ehab Mohammed1, Issa Al Salmi1 *, Shilpa Ramaiah1 and Suad Hannawi2 Kidney Disease (CKD) is increasingly recognized as a global public health challenge as 10% of the global population is affected [1,2]. 1Nephrologist, The Renal Medicine Department, The Royal Hospital, Muscat, Oman The scarcity of well-trained renal pathologists, even in high-in- come countries, is a major obstacle to use of biopsy samples. The ISN 2Medicine Department, Ministry of Health and Prevention, Dubai, UAE is working worldwide to enhance development of local renal patholo- gy expertise. Levin et al stated that analysis of kidney biopsy samples can be used to stratify CKD into distinct subgroups of diseases based Abstract on specific histological patterns, when combined with the clinical pre- sentation [3]. Diabetes mellitus and hypertensive nephropathy are the Objectives: To Provide up-to-date guidelines for medical and nurs- commonly identified causes of End-Stage Kidney Disease (ESKD). ing staffs on the pre, during, and post care of a patient undergoing a Also, many patients with glomerulonephritis, systemic lupus erythe- percutaneous-kidney-biopsy-PKB. -

Clinical Significance of Cystoscopic Urethral Stricture
UCSF UC San Francisco Previously Published Works Title Clinical significance of cystoscopic urethral stricture recurrence after anterior urethroplasty: a multi-institution analysis from Trauma and Urologic Reconstructive Network of Surgeons (TURNS). Permalink https://escholarship.org/uc/item/3f57n621 Journal World journal of urology, 37(12) ISSN 0724-4983 Authors Baradaran, Nima Fergus, Kirkpatrick B Moses, Rachel A et al. Publication Date 2019-12-01 DOI 10.1007/s00345-019-02653-6 Peer reviewed eScholarship.org Powered by the California Digital Library University of California World Journal of Urology https://doi.org/10.1007/s00345-019-02653-6 ORIGINAL ARTICLE Clinical signifcance of cystoscopic urethral stricture recurrence after anterior urethroplasty: a multi‑institution analysis from Trauma and Urologic Reconstructive Network of Surgeons (TURNS) Nima Baradaran1 · Kirkpatrick B. Fergus2 · Rachel A. Moses3 · Darshan P. Patel3 · Thomas W. Gaither2 · Bryan B. Voelzke4 · Thomas G. Smith III5 · Bradley A. Erickson6 · Sean P. Elliott7 · Nejd F. Alsikaf8 · Alex J. Vanni9 · Jill Buckley10 · Lee C. Zhao11 · Jeremy B. Myers3 · Benjamin N. Breyer2 Received: 13 December 2018 / Accepted: 24 January 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose To assess the functional Queryoutcome of patients with cystoscopic recurrence of stricture post-urethroplasty and to evaluate the role of cystoscopy as initial screening tool to predict future failure. Methods Cases with cystoscopy data after anterior urethroplasty in a multi-institutional database were retrospectively studied. Based on cystoscopic evaluation, performed within 3-months post-urethroplasty, patients were categorized as small-caliber (SC) stricture recurrence: stricture unable to be passed by standard cystoscope, large-caliber (LC) stricture accommodating a cystoscope, and no recurrence. -

Cystoscopy Into the Bladder Via the Urethra, It Is About As Thick As a a Guide for Women
A flexible cystoscope is a thin telescope which is passed Cystoscopy into the bladder via the urethra, it is about as thick as a A Guide for Women pencil. As the cystoscope is flexible, it usually passes easily 1. What is a Cystoscopy? moved so the doctor can look at all the inside lining of the along the curves of the urethra. The flexible tip can also be 2. Why is a Cystoscopy performed? bladder and the opening of the ureters. 3. Preparation for the test 4. About the test 5. Are there any risks? A rigid cystoscope is a shorter rigid telescope, it allows 6. What to expect afterwards? a greater variety of devices to pass down side channels so that the doctor can for example take samples or inject into the bladder. Sometimes, it is necessary to perform a rigid What is a Cystoscopy? Cystoscopy is the name for a procedure allowing a doctor to look into your bladder and urethra with a special telescope cystoscopy at a later date after a flexible cystoscopy. called a cystoscope. Preparation for the test If you are having an outpatient procedure in most cases you When you have a bladder problem, your doctor may use a will be able to eat and drink normally prior to the test. If you cystoscope to see inside your bladder and urethra. The ure- are having general anesthesia, you should refrain from eat- thra is the tube that carries urine from the bladder to the ing and drinking for 6 to 8 hours prior to your cystoscopy. -
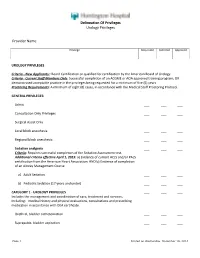
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

A Systematic Review of Graft Augmentation Urethroplasty Techniques for the Treatment of Anterior Urethral Strictures
EUROPEAN UROLOGY 59 (2011) 797–814 available at www.sciencedirect.com journal homepage: www.europeanurology.com Review – Reconstructive Urology A Systematic Review of Graft Augmentation Urethroplasty Techniques for the Treatment of Anterior Urethral Strictures Altaf Mangera *, Jacob M. Patterson, Christopher R. Chapple Royal Hallamshire Hospital, Sheffield, United Kingdom Article info Abstract Article history: Context: Reconstructive surgeons who perform urethroplasty have a variety of Accepted February 2, 2011 techniques in their armamentarium that may be used according to factors such as Published online ahead of aetiology, stricture position, and length. No one technique is recommended. print on February 11, 2011 Objective: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. Keywords: Evidence acquisition: We performed an updated systematic review of the Medline Augmentation urethroplasty literature from 1985 to date and classified the data according to the site of surgery Anterior urethral stricture and technique used. Data are also presented on the type of graft used and the Bulbar urethroplasty follow-up methodology used by each centre. Dorsal onlay bulbar Evidence synthesis: More than 2000 anterior urethroplasty procedures have been urethroplasty describedinthe literature.Whenconsidering the bulbar urethra there isnosignificant Ventral onlay bulbar difference between the average success rates of the dorsal and the ventral onlay urethroplasty procedures, 88.4% and 88.8% at42.2 and 34.4 moin 934 and 563 patients,respectively. Penile urethroplasty The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. -

Efficacy of Revision Urethroplasty in the Treatment Of
ORIGINAL ARTICLE Bali Medical Journal (Bali Med J) 2020, Volume 9, Number 1: 67-76 P-ISSN.2089-1180, E-ISSN.2302-2914 Efficacy of revision urethroplasty in the treatment of ORIGINAL ARTICLE recurrent urethral strictures at a tertiary hospital (Kenyatta National Hospital–KNH), in Nairobi Kenya: Published by DiscoverSys CrossMark Doi: http://dx.doi.org/10.15562/bmj.v9i1.1675 2015-2018 Willy H. Otele,* Sammy Miima, Francis Owilla, Simeon Monda Volume No.: 9 ABSTRACT Issue: 1 Background: Urethral strictures cause malfunction of the urethra. while Subsidiary outcome measures were associated complications. Urethroplasty is a cost-effective treatment option. Its success rate Outcomes were compared using statistical package SPSS version 23.0. is greater than 90% where excision and primary anastomosis(EPA) Result: 235 patients who met inclusion criteria underwent is performed and 80-85% following substitution urethroplasty. urethroplasty, 71.5% (n=168) had a successful outcome, while28.5% First page No.: 67 Definitive treatment for recurrent urethral strictures after (n=67) failed and were subjected to revision urethroplasty. Another urethroplasty is not defined. Repeat urethroplasty is a viable option 58% were successful upon revision but experienced significant with unknown efficacy. morbidity. Majority of urethral strictures were bulbomembranous. P-ISSN.2089-1180 Method: Retrospective analysis of patients who underwent revision Trauma was the leading cause of urethral strictures followed by urethroplasty for unsuccessful urethroplasty at KNH from 2015 to idiopathic strictures. EPA was the commonest surgery while Tissue 2018 was performed. Patients’ age, demographic data, stricture transfer featured prominently in revision urethroplasty. A significant length, location, aetiology, comorbidities and type of urethroplasty correlation was evident between stricture length, prior surgery, and E-ISSN.2302-2914 was evaluated from records with complete data. -

Complications of Ureteroscopic Approaches, Including Incisions
18 Complications of Ureteroscopic Approaches, Including Incisions Farjaad M. Siddiq, MD and Raymond J. Leveillee, MD CONTENTS INTRODUCTION PREPARATION FOR URETEROSCOPY URETERAL ACCESS DILATION OF THE URETERAL ORIFICE: IS IT NECESSARY? COMPLICATIONS OF URETEROSCOPY URETERAL STENTS: ARE THEY NECESSARY? POSTOPERATIVE IMAGING COMPLICATIONS OF URETEROSCOPIC MANAGEMENT OF UPPER TRACT TCC COMPLICATIONS OF URETEROSCOPIC INCISIONS CONCLUSION REFERENCES SUMMARY Ureteroscopy has progressed from cystoscopic examination of a dilated ureter in a child in 1929 and the initial use of rigid ureteroscopes in the 1980s, to its current state of small caliber semirigid and flexible instruments. In this chapter the authors review complications of ureteroscopy including those associated with incisional techniques where one would anticipate a higher incidence of complications. They review the his- tory and development of modern ureteroscopes, focusing on engineering advances. Clinical points made include proper patient selection and preparation; proper use of dilators, wires, and ureteral access sheaths; and the incidence, identification, and man- agement of complications associated with ureterorenoscopy (both intraopertively and postoperatively). Key Words: Ureteroscopy; calculi; urinary stones; stricture or ureter; urothelial carcinoma; surgical complications. From: Advanced Endourology: The Complete Clinical Guide Edited by: S. Y. Nakada and M. S. Pearle © Humana Press Inc., Totowa, NJ 299 300 Siddiq and Leveillee INTRODUCTION Ureteroscopy has progressed from cystoscopic examination of a dilated ureter in a child with posterior urethral valves by Young and McKay (1) in 1929 and the initial use of a rigid ureteroscope by Perez-Castro Ellendt and Martinez-Pineiro (2,3) in the early 1980s, to its current state of small caliber semirigid and flexible instruments. -

Percutaneous Ultrasound-Guided Renal Biopsy; a Comparison of Axial Vs
Percutaneous ultrasound-guided renal biopsy; A comparison of axial vs. sagittal probe location FARNAZ SHAMSHIRGAR1, SEYED MORTEZA BAGHERI2* 1Resident of Radiology, Iran University of Medical Sciences, Tehran, Iran 2Department of Radiology, Hasheminejad Kidney Center (HKC), Iran University of Medical Sciences, Tehran, Iran Background. Renal biopsy is an important method for diagnosis of renal parenchymal abnormalities. Here, we compare the effectiveness and complications of percutaneous ultrasound- guided renal biopsy using axial vs. sagittal probe locations. Methods. In a cross-sectional survey, in 2012, patients with a nephrologist order were biopsied by a radiology resident. Renal biopsy was done on 15 patients using axial (A group) and the same number of biopsies done with sagittal probe location (S group). The two groups were compared in term of the yields and complications of each method. Results. In the A group, the ratio of glomeruli gathered to the number of obtained samples was significantly higher than in the S group. Nine patients in the A group (60%) required only two samplings, whereas 66.7% in the S group required more than two attempts. Microscopic hematuria was more common in the A; conversely, gross hematuria was less common in the A group. Meagre hematomas were more frequent in the S group .When compared with hemoglobin level before biopsy, its level 24 hours after biopsy was similar within groups. Conclusion. Our study shows that percutaneous ultrasound-guided renal biopsy using axial probe provides better yield with fewer efforts and fewer serious complications. Keywords: Percutaneous renal biopsy, Ultrasound-guided renal biopsy, Ultra-sonography probe location. INTRODUCTION plications and related post therapeutic side effects may cause another complication such as vascular Percutaneous renal biopsy is an important occlusion, acute obstruction of renal output, renal method to diagnose most kidney diseases.