Spring Case Study &
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Single Port Laparoscopic Hysterectomy Through a 12Mm Incision Created by a Bladeless Trocar: a Novel Technique
Single Port Laparoscopic Hysterectomy through a 12mm incision created by a Bladeless Trocar: A Novel Technique Greg J. Marchand, M.D., Katelyn M. Sainz MS1 From the National Foundation for Minimally Invasive Surgery (minvase.org), and Research and Development division of Marchand OBGYN PLLC Precis: Single Port Hysterectomy can be performed safely through a 12mm bladeless incision via this novel technique. Decreasing port size is continually pushing the limits of minimally invasive surgery for enhanced patient outcomes. Corresponding author: Greg J. Marchand M.D., Marchand OBGYN Research and Development, 1520 S. Dobson #218, Mesa, AZ 85202, Tel: 480-628-0566, Fax: 480-999-0801 ABSTRACT Study Objective: The aim of this study is to report the technique used by one surgeon performing a laparoscopic hysterectomy performed through a single 12mm bladeless incision. With the exception of pure vaginal hysterectomy we believe this technique is the least invasive technique published thus far to date where the hysterectomy is performed entirely abdominally. Design: Retrospective Analysis of Charts and Technique Setting: One private Hospital in the Southwest US Patients: 6 patients receiving single port hysterectomy between 2013 and 2014 Intervention: Single Port Laparoscopic Hysterectomy was performed with our ultra-minimally invasive technique, using a Covidien(C) 12mm bladeless laparoscopic trocar followed by an Olympus(C) TriPort device and Olypus(C) articulating 5mm laparoscope without in any way stretching or extending the 12mm port. Other novel aspects of our technique include placement of the single port at the bottom of the umbilicus regardless of patient BMI, the usage of intra-abdominal marcaine to help with postoperative pain and vaginal repair of colpotomy. -

Entry Techniques in Gynecologic Laparoscopy—A Review
Gynecol Surg (2012) 9:139–146 DOI 10.1007/s10397-011-0710-8 REVIEW ARTICLE Entry techniques in gynecologic laparoscopy—a review Johannes Ott & Agnes Jaeger-Lansky & Gunda Poschalko & Regina Promberger & Eleen Rothschedl & René Wenzl Received: 9 June 2011 /Accepted: 19 October 2011 /Published online: 13 November 2011 # Springer-Verlag 2011 Abstract Laparoscopy is one of the most common surgical underpowered in order to assess the risk for rare but life- procedures in gynecologic medicine. Major complications threatening complications. In conclusion, there is no solid associated with gynecologic laparoscopy are relatively rare, evidence proving the superiority of any method of with up to 50% related to laparoscopic entry. Several entry laparoscopic entry. techniques have been developed, all of which aim to provide a safe and easy entry to the abdominal cavity. In Keywords Laparoscopy. Entry techniques . Gynecology. this article, we aim to review the available evidence on Complications . Veress needle . Hasson technique . Direct laparoscopic entry techniques in gynecologic surgery. We trocar entry found no evidence that the Hasson (open) technique is superior to the Veress needle entry, the preferred method of most gynecologists all over the world. When entering the Background abdomen using the Veress needle, an intraperitoneal pressure <10 mmHg is a reliable predictor of correct Laparoscopy is one of the most common surgical intraperitoneal placement. Entry at Palmer’s point (left procedures in gynecologic medicine and has become upper quadrant laparoscopy) is recommended for patients the method of choice over the last few decades for with suspected or known periumbilical adhesions, or a treating benign diseases that require surgery [1, 2]. -

Comparison Between Different Entry Techniques in Performing Pneumoperitoneum In10.5005/Jp-Journals-10033-1257 Laparoscopic Gynecological Surgery REVIEW ARTICLE
WJOLS Comparison between Different Entry Techniques in Performing Pneumoperitoneum in10.5005/jp-journals-10033-1257 Laparoscopic Gynecological Surgery REVIEW ARTICLE Comparison between Different Entry Techniques in Performing Pneumoperitoneum in Laparoscopic Gynecological Surgery Mandavi Rai ABSTRACT safety of one technique over another. However, the included studies are small and cannot be used to confirm safety of any Background: The main challenge facing the laparoscopic particular technique. No single technique or instrument has surgery is the primary abdominal access, as it is usually a blind been proved to eliminate laparoscopic entry-associated injury. procedure associated with vascular and visceral injuries. Lapa- Proper evaluation of the patient, supported by good surgical roscopy is a very common procedure in gynecology. Complica- skills and reasonably good knowledge of the technology of the tions associated with laparoscopy are often related to entry. instruments remain to be the cornerstone for safe access and The life-threatening complications include injury to the bowel, success in minimal access surgery. bladder, major abdominal vessels, and anterior abdominal- wall vessel. Other less serious complications can also occur, Keywords: Complications, Laparoscopy, Pnumoperitoneum, such as postoperative infection, subcutaneous emphysema Trocar. and extraperitoneal insufflation. There is no clear consensus as to the optimal method of entry into the peritoneal cavity. It How to cite this article: Rai M. Comparison between Dif- has been proved from studies that 50% of laparoscopic major ferent Entry Techniques in Performing Pneumoperitoneum complications occur prior to the commencement of the surgery. in Laparos copic Gynecological Surgery. World J Lap Surg The surgeon must have adequate training and experience in 2015;8(3):101-106. -

Use of the Veress Needle to Obtain Pneumoperitoneum Prior to Laparoscopy
Use of the Veress needle to obtain pneumoperitoneum prior to laparoscopy Consensus statement of the Royal Australian & New Zealand College of Obstetricians & Gynaecologists This statement has been developed by the Women’s (RANZCOG) and the Australasian Gynaecological Health Committee. It has been reviewed by the Endoscopy and Surgery Society (AGES). Endoscopic Surgery Advisory Committee (RANZCOG/AGES) and approved by the Objectives: To provide advice on the use of the RANZCOG Board and Council. Veress needle to obtain pneumoperitoneum prior to laparoscopy. A list of Women’s Health Committee and Endoscopic Surgery Advisory Committee Target audience: Health professionals providing (RANZCOG/AGES) Members can be found in gynaecological care, and patients. Appendix A. Values: The evidence was reviewed by the Disclosure statements have been received from all Endoscopic Surgery Advisory Committee members of this committee. (RANZCOG/AGES), and applied to local factors relating to Australia and New Zealand. Disclaimer This information is intended to provide Background: This statement was first developed by general advice to practitioners. This information Women’s Health Committee in April 1990 and most should not be relied on as a substitute for proper recently reviewed by the Endoscopic Surgery assessment with respect to the particular Committee (RANZCOG/AGES) in July 2017. circumstances of each case and the needs of any patient. This document reflects emerging clinical Funding: The development and review of this and scientific advances as of the date issued and is statement was funded by RANZCOG. subject to change. The document has been prepared having regard to general circumstances. First endorsed by RANZCOG: April 1990 Current: July 2017 Review due: July 2020 1 Table of contents Table of contents ............................................................................................................................ -

AUA BLUS Handbook of Laparoscopic and Robotic Fundamentals
AUA BLUS Handbook of Laparoscopic and Robotic Fundamentals Sean Collins, Daniel S. Lehman, Elspeth M. McDougall, Ralph V. Clayman, and Jaime Landman ©American Urological Association Education & Research, Inc. Table of Contents 1. Introduction 2. Patient selection a. Indication b. contradindications c. special considerations 3. Physiologic effects of pneumoperitoneum a. Renal surgery transperitoneal b. Renal surgery retroperitoneal c. Hand-assisted laparoscopic nephrectomy d. Prostatectomy 4. Getting Started 5. Patient positioning a. Renal surgery transperitoneal b. Renal surgery retroperitoneal c. Hand-assisted laparoscopic nephrectomy d. Prostatectomy 6. Strategic placement of surgical team and operating room (OR) equipment 7. Access a. Primary access b. Renal surgery transperitoneal trocar placement c. Renal surgery retroperitoneal trocar placement d. Secondary access e. Retroperitoneal primary and secondary access f. Hand-assisted laparoscopic nephrectomy trocar placement g. Prostatectomy trocar placement 8. Instrumentation a. Trocars i. Cutting ii. Dilating iii. Radially dilating b. Bipolar cautery c. Monopolar cautery d. Ultrasonic instrumentation e. Vessel sealing devices i. LigaSure ii. Enseal f. Staplers g. Vascular clamps h. Suture anchors i. Titanium clips j. Locking clips q. Retractors r. Hemostatic agents s. Hand Assisted devices 2 9. Technique for Transperitoneal Laparoscopic Nephrectomy 10. Complications of laparoscopic surgery 3 Chapter 1. Introduction The American Urological Association (AUA) has prepared this handbook for all those new to laparoscopy. Rather than being a detailed surgical atlas, this is a handbook designed to introduce the fundamental principles of laparoscopy including: indications and contraindications for laparoscopy, the physiologic effects of pneumoperitoneum, patient positioning; abdominal access and trocar placement; strategic placement of the operating room (OR) team and equipment, overview of laparoscopic instrumentation, and complications unique to laparoscopic surgery. -
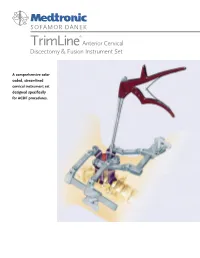
TRIMLINE® ACDF INSTRUMENT SET Cat
SOFAMOR DANEK ® TrimLine Anterior Cervical Discectomy & Fusion Instrument Set A comprehensive color coded, streamlined cervical instrument set designed specifically for ACDF procedures. Anterior Cervical Discectomy and Graft Curettes Fusion Instrument Set Placement Instruments Color coded handles to differentiate sizes The TrimLine ACDF Instrument Set has been designed Can be used with autograft or allograft Hand polished cutting specifically for standard cervical anterior approaches, Holder/Introducer will not leave a hole in surfaces to help discectomies, and fusions. It includes instruments necessary the graft maintain sharp edges to perform the cervical exposure, decompression, graft harvest, Ergonomically designed handles Fully machined and placement. Instruments are color coded to simplify components to enhance identification and this feature allows the procedure to product run more smoothly. Instruments can be purchased consistency separately or as part of the TrimLine Set. Kerrisons Color coded handles to differentiate sizes Hand polished cutting surfaces to help maintain sharp edges Fully machined components to enhance product consistency Pin Distraction Set Universally acceptable Self-Retaining instruments Retractors Improved pin strength Right and left options Generic blade for use with either fixed or rotating Hand-Held modular blade handles Retractors Modular blade handles can be removed after retractor frame is added Aluminum blades for better imaging Improved side-loading connection mechanism Ergonomically -

Miltex® Ophthalmic Instruments
OPHTHALmic INSTRUMENTS MILTEX ® OPHTHALMIC INSTRUMENTS The MILTEX® name is synonymous with unparalleled quality and service to our customers and surgical instrumentation produced with the utmost attention to consistent detail. The MILTEX® Ophthalmology product line includes both premium-grade German and American crafted stainless steel surgical instrumentation manufactured to exacting specifications. The surgical “feel” of our instruments, the outstanding cutting ability and the attention to delicate detail are just a few of the aspects that allow our products to outperform and stand out from the competition. This catalog presents our comprehensive offering of instruments necessary to support the innovative surgical techniques and advances in the field of Ophthalmology. In addition to our Ophthalmic offering, Miltex provides instruments to meet a variety of clinical needs for other specialties including: Plastic Surgery, Dermatology, Otolaryngology, Microsurgery, Gynecology, General Surgery as well as several other markets. General Information: Photographs in this catalog are close to actual size except where otherwise noted. Many illustrations are enlarged to show detail. Surgical instruments shown in this catalog are made of high quality surgical grade stainless steel, unless otherwise noted. Illustrations and content provide general description only and may be subject to change. Some products in this catalog may not be available for sale in the European Union. Miltex and Miltex Redefining Excellence are registered trademarks of Miltex, -

Answer Key Chapter 1
Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 1 of 101 Answer Key Chapter 1 Introduction to Clinical Coding 1.1: Self-Assessment Exercise 1. The patient is seen as an outpatient for a bilateral mammogram. CPT Code: 77055-50 Note that the description for code 77055 is for a unilateral (one side) mammogram. 77056 is the correct code for a bilateral mammogram. Use of modifier -50 for bilateral is not appropriate when CPT code descriptions differentiate between unilateral and bilateral. 2. Physician performs a closed manipulation of a medial malleolus fracture—left ankle. CPT Code: 27766-LT The code represents an open treatment of the fracture, but the physician performed a closed manipulation. Correct code: 27762-LT 3. Surgeon performs a cystourethroscopy with dilation of a urethral stricture. CPT Code: 52341 The documentation states that it was a urethral stricture, but the CPT code identifies treatment of ureteral stricture. Correct code: 52281 4. The operative report states that the physician performed Strabismus surgery, requiring resection of the medial rectus muscle. CPT Code: 67314 The CPT code selection is for resection of one vertical muscle, but the medial rectus muscle is horizontal. Correct code: 67311 5. The chiropractor documents that he performed osteopathic manipulation on the neck and back (lumbar/thoracic). CPT Code: 98925 Note in the paragraph before code 98925, the body regions are identified. The neck would be the cervical region; the thoracic and lumbar regions are identified separately. Therefore, three body regions are identified. Correct code: 98926 Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 2 of 101 6. -

AST Guidelines for Counts
Recommended Standard of Practice for Counts Introduction The following Recommended Standards of Practice were researched and written by the AST Education and Professional Standards Committee and have been approved by the AST Board of Directors. They are effective October 27, 2006. AST developed the following Recommended Standards of Practice to support facilities in the reinforcement of best practices, related to performing the sponge, needle and instrument counts in the perioperative setting. The purpose of the Recommended Standards is to provide an outline that surgical team members can use to develop and implement policies and procedures for counts. The Recommended Standards is presented with the understanding that it is the responsibility of the healthcare facility to develop, approve, and establish policies and procedures for performing counts, according to established healthcare facility protocols. Rationale The following are Recommended Standards of Practice related to properly performing sponge, needle and instrument counts in the perioperative setting. It is recommended that sponge, needle and instrument counts be performed on all procedures that present with the possibility that a foreign object could be retained in order to increase patient safety practices in the perioperative setting. Risk factors identified as increasing the occurrence of an incorrect count or retained item include the following: emergency surgical procedures, unexpected change in the scope of the surgical procedure, procedures involving more than one surgical team, extended procedural length of time, unexpected transfusions, and morbidly obese patients.18 One of several safe patient outcomes related to surgery is all items viewed as retainable foreign objects are accounted for at the end of the surgical procedure, due to careful counting and documentation by the surgical team. -

Surgery Instrumnts Khaled Khalilia Group 7
Surgery Instrumnts khaled khalilia Group 7 Scalpel handle blade +blade scalpel blade disposable fixed blade knife (Péan - Hand-grip : This grip is best for initial incisions and larger cuts. - Pen-grip : used for more precise cuts with smaller blades. - Changing Blade with Hemostat Liston Charrière Saw AmputationAmputati knife on knife Gigli Saw . a flexible wire saw used by surgeons for bone cutting .A gigli saw is used mainly for amputation surgeries. is the removal of a body extremity by trauma, prolonged constriction, or surgery. Scissors: here are two types of scissors used in surgeries.( zirconia/ ceramic,/ nitinol /titanium) . Ring scissors look much like standard utility scissors with two finger loops. Spring scissors are small scissors used mostly in eye surgery or microsurgery . Bandage scissors: Bandage scissors are angled tip scissors. helps in cutting bandages without gouging the skin. To size bandages and dressings. To cut through medical gauze. To cut through bandages already in place. Tenotomy Scissors: used to perform delicate surgery. used to cut small tissues They can be straight or curved, and blunt or sharp, depending upon necessity. operations in ophthalmic surgery or in neurosurgery. 10 c”m Metzenbaum scissors: designed for cutting delicate tissue come in variable lengths and have a relatively long shank-to-blade ratio blades can be curved or straight. the most commonly used scissors for cutting tissue. Use: ental, obstetrical, gynecological, dermatological, ophthalmological. Metzenbaum scissors Bandage scissors Tenotomy scissors Surgical scissors Forceps: Without teeth With teeth Dissecting forceps (Anatomical) With teeth: for tougher(hart) tissue: Fascia,Skin Without teeth: (atraumatic): for delicate tissues (empfindlich): Bowel Vessels. -

11 Cardiac Instruments
FEHLING AORTIC PUNCHES INS TRUMENTS AORTENSTANZEN 11/1 FEHLING... ... THE DIFFERENCE INSTRUMENTS FOR THORACIC, CARDIAC AND VASCULAR SURGERY INSTRUMENTE FÜR THORAX-, HERZ- UND GEFÄSSCHIRURGIE FEHLING Hanauer Landstraße 7A · 63791 Karlstein/Germany · www.fehling-instruments.de INSTRUMENTS +49(0) 6188 - 9574.40 +49(0) 6188 - 9574.45 [email protected] FEHLING STERNAL RETRACTORS INSTRUMENTS STERNUMSPREIZER 11/2 CALAFIORE STERNAL RETAINER STERNUMOFFENHALTER 1 1 ⁄2 ⁄4 1 1 1 ⁄16 ⁄2 ⁄2 STERNUM BLADE SCREW NUT STERNUMBLATT FLAT WRENCH STORAGE TRAY MUTTER GABELSCHLÜSSEL LAGERUNGS- LEFT RIGHT SINGLE USE BEHÄLTER LINKS RECHTS MPA-5 MPC-1L MPC-1R NEONATAL 7 x 30 mm** MPB-1 7 x 30 mm* 7 x 30 mm* Ø 8 MPC-0P MPB-7L MPB-7R 10 x 18 mm* 10 x 18 mm* MPA-6 “PEDIATRIC“ PEDIATRIC 45 x 65 mm** MPB-2 MPA-2L MPA-2R Ø 12 10 x 50 mm* 10 x 50 mm* MPA-3L MPA-3R ADULT 15 x 70 mm* 15 x 70 mm* MPA-9 45 x 65 mm** MPC-0A Ø 16 “ADULT“ MPA-4L MPA-4R ADIPOSIS 20 x 100 mm* 20 x 100 mm* MPA-7 70 x 90 mm** MPB-3 Ø 16 MPB-5L MPB-5R 15 x 30 mm* 15 x 30 mm* MPA-8 MPC-0C OSTEOPOROSIS 95 x 115 mm** “CURVED“ MPB-6L MPB-6R Ø 16 20 x 30 mm* 20 x 30 mm* *blade size / Blattgröße **opening width / Öffnungsweite exemplary configuration exemplary configuration Beispielkonfiguration Beispielkonfiguration ADULT - ADIPOSIS OSTEOPOROSIS FEHLING RETRACTORS INSTRUMENTS SPREIZER 11/3 TILTING KIPPBAR FOR PARTIAL STERNOTOMY FÜR PARTIELLE STERNOTOMIE BLADE SIZE BLATTGRÖSSE SPREADING WIDTH 160 mm a x b SPREIZWEITE 100 mm 35 x 50 mm MRM-5 45 x 50 mm MRM-6 215 mm 1 ⁄3 MARJAN 2 ⁄3 SUPERFLEX SOFT TISSUE RETRACTOR WEICHGEWEBERETRAKTOR 200 x 25 mm MTI-0 2 ⁄3 STERILISATION AND STORAGE TRAY FOR MTI-0 STERILISIER- UND LAGERSIEB FÜR MTI-0 220 x 51,2 x 19,5 mm MTK-0 FEHLING PROBES/SIZERS INSTRUMENTS SONDEN/LEHREN 11/6 SUPERPLAST A 45 mm A for mitral valve repair techniques without prosthetic ring SUPERPLAST instruments are construc- für Mitralklappenrekonstruktion ted of shape-memory metal. -

Intraperitoneal Access by Closed Method (Veress Needle) Versus Open (Hasson’S) Method in Laparoscopic Surgery to Create Pneumoperitoneum
International Surgery Journal Chotai NR et al. Int Surg J. 2017 Aug;4(8):2786-2790 http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902 DOI: http://dx.doi.org/10.18203/2349-2902.isj20173419 Original Research Article Intraperitoneal access by closed method (veress needle) versus open (Hasson’s) method in laparoscopic surgery to create pneumoperitoneum Neet R. Chotai*, Dilip B. Choksi, Sushil Damor, Amul Bhedi Department of General Surgery, Government Medical College Baroda, Vadodara, India Received: 18 May 2017 Accepted: 17 June 2017 *Correspondence: Dr. Neet R. Chotai, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Access into the abdomen is the one challenge of laparoscopy that is particular to the insertion of surgical instruments through small incisions. In the last three decades, rapid advances in laparoscopic surgery have made it an invaluable part of general surgery, but there remains no clear consensus as an on optimal method of entry into the peritoneal cavity. The objective of this study was to study the comparison and efficacy between closed (veress needle)and open method (Hasson’s) of intraperitoneal access to create pneumoperitoneum in laparoscopic surgeries. Methods: All patients >18 year undergoing laparoscopic procedure at Sir Sayajirao Gaekwad Hospital attached to Medical College Baroda from November 2015 to November 2016, and include 160 patients.