Different Port Closure Techniques in Laparoscopy Surgery Different Port Closure Techniques in Laparoscopy Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Instruments �������������������������������������������
SURGICAL INSTRUMENTS Claudia Gherman, ăCiocan, Ovidiu Fabian Learning objectives What you should know The main types of surgical instruments The main instruments used for cutting tissues The main instruments used for tissue manipulation The main instruments used for exposure (retractors) The main instruments used for suturing The functioning principle of electrocautery devices The main laparoscopic instruments What you should do Recognize the main surgical instruments Attach a scalpel blade to a handle/remove it from the handle Hand a scalpel to another person correctly Perform an incision Handle scissors (hold them correctly, cut under visual control, hand scissors to another person) Handle a self-retaining forceps (hold it correctly, grip the tissue, close and open the forceps, hand it to another person) Hold a retractor correctly Hold, close/open and hand over a needle holder correctly Recognize a suturing needle; recognize a sharp needle and an intestinal needle; find on the needle and suture package the main information about the needle Classification In order to perform surgery, the surgical team needs a number of surgical instruments. Each of the thousands of instruments used is designed for a specific function. They can be classified depending on use as follows: Cutting instruments Instruments for tissue grasping and manipulation Instruments for tissue exposure Suturing instruments Hybrid instruments Endoscopic instruments Cutting instruments Scalpels: consist of a handle and a blade; the handle is made of metal (reusable) or plastic (disposable); blades are disposable, of various shapes and sizes. The top of the scalpel handle has a special part, with a groove that allows its sliding into the blade slot and securing of the blade in position. -

Answer Key Chapter 1
Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 1 of 101 Answer Key Chapter 1 Introduction to Clinical Coding 1.1: Self-Assessment Exercise 1. The patient is seen as an outpatient for a bilateral mammogram. CPT Code: 77055-50 Note that the description for code 77055 is for a unilateral (one side) mammogram. 77056 is the correct code for a bilateral mammogram. Use of modifier -50 for bilateral is not appropriate when CPT code descriptions differentiate between unilateral and bilateral. 2. Physician performs a closed manipulation of a medial malleolus fracture—left ankle. CPT Code: 27766-LT The code represents an open treatment of the fracture, but the physician performed a closed manipulation. Correct code: 27762-LT 3. Surgeon performs a cystourethroscopy with dilation of a urethral stricture. CPT Code: 52341 The documentation states that it was a urethral stricture, but the CPT code identifies treatment of ureteral stricture. Correct code: 52281 4. The operative report states that the physician performed Strabismus surgery, requiring resection of the medial rectus muscle. CPT Code: 67314 The CPT code selection is for resection of one vertical muscle, but the medial rectus muscle is horizontal. Correct code: 67311 5. The chiropractor documents that he performed osteopathic manipulation on the neck and back (lumbar/thoracic). CPT Code: 98925 Note in the paragraph before code 98925, the body regions are identified. The neck would be the cervical region; the thoracic and lumbar regions are identified separately. Therefore, three body regions are identified. Correct code: 98926 Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 2 of 101 6. -

AST Guidelines for Counts
Recommended Standard of Practice for Counts Introduction The following Recommended Standards of Practice were researched and written by the AST Education and Professional Standards Committee and have been approved by the AST Board of Directors. They are effective October 27, 2006. AST developed the following Recommended Standards of Practice to support facilities in the reinforcement of best practices, related to performing the sponge, needle and instrument counts in the perioperative setting. The purpose of the Recommended Standards is to provide an outline that surgical team members can use to develop and implement policies and procedures for counts. The Recommended Standards is presented with the understanding that it is the responsibility of the healthcare facility to develop, approve, and establish policies and procedures for performing counts, according to established healthcare facility protocols. Rationale The following are Recommended Standards of Practice related to properly performing sponge, needle and instrument counts in the perioperative setting. It is recommended that sponge, needle and instrument counts be performed on all procedures that present with the possibility that a foreign object could be retained in order to increase patient safety practices in the perioperative setting. Risk factors identified as increasing the occurrence of an incorrect count or retained item include the following: emergency surgical procedures, unexpected change in the scope of the surgical procedure, procedures involving more than one surgical team, extended procedural length of time, unexpected transfusions, and morbidly obese patients.18 One of several safe patient outcomes related to surgery is all items viewed as retainable foreign objects are accounted for at the end of the surgical procedure, due to careful counting and documentation by the surgical team. -

Images Paediatr Cardiol
RK Kumar and AC Nair. Coil Occlusion of the Large Patent Ductus Arteriosus. Images Paediatr Cardiol. 2008 Jan-Mar; 10(1): 8–26. in PAEDIATRIC CARDIOLOGY IMAGES Images Paediatr Cardiol. 2008 Jan-Mar; 10(1): 8–26. PMCID: PMC3232586 Coil Occlusion of the Large Patent Ductus Arteriosus RK Kumar and AC Nair Amrita Institute of Medical Sciences and Research Centre, Kochi, Kerala, India Contact information: R. K. Kumar, Amrita Institute of Medical Sciences and Research Centre, Elamakkara PO, Kochi 682026, Kerala, India Phone: 91- 484-280-4001599 Fax: 91-484-2802020 ; Email: [email protected] Copyright : © Images in Paediatric Cardiology This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract While coil occlusion is well accepted for the small patent ductus arteriosus (PDA), occlusive devices are preferred for the larger (> 3 mm) ducts by most institutions. Because of costs concerns, occlusive devices are not always realistic in many countries. The technique of simultaneous delivery of multiple coils with bioptome assistance works well for relatively larger ducts. This technique requires careful case selection through echocardiography. The duct anatomy plays a crucial part in determining the suitability for coil occlusion. Coil occlusion has a specific advantage for relatively larger ducts in selected small children and in preterm infants because it is possible to accomplish delivery of multiple coils through relatively small introducer sheaths. In addition, aortic narrowing is less likely because coils compact in the ampulla. -

Surgery Instrumnts Khaled Khalilia Group 7
Surgery Instrumnts khaled khalilia Group 7 Scalpel handle blade +blade scalpel blade disposable fixed blade knife (Péan - Hand-grip : This grip is best for initial incisions and larger cuts. - Pen-grip : used for more precise cuts with smaller blades. - Changing Blade with Hemostat Liston Charrière Saw AmputationAmputati knife on knife Gigli Saw . a flexible wire saw used by surgeons for bone cutting .A gigli saw is used mainly for amputation surgeries. is the removal of a body extremity by trauma, prolonged constriction, or surgery. Scissors: here are two types of scissors used in surgeries.( zirconia/ ceramic,/ nitinol /titanium) . Ring scissors look much like standard utility scissors with two finger loops. Spring scissors are small scissors used mostly in eye surgery or microsurgery . Bandage scissors: Bandage scissors are angled tip scissors. helps in cutting bandages without gouging the skin. To size bandages and dressings. To cut through medical gauze. To cut through bandages already in place. Tenotomy Scissors: used to perform delicate surgery. used to cut small tissues They can be straight or curved, and blunt or sharp, depending upon necessity. operations in ophthalmic surgery or in neurosurgery. 10 c”m Metzenbaum scissors: designed for cutting delicate tissue come in variable lengths and have a relatively long shank-to-blade ratio blades can be curved or straight. the most commonly used scissors for cutting tissue. Use: ental, obstetrical, gynecological, dermatological, ophthalmological. Metzenbaum scissors Bandage scissors Tenotomy scissors Surgical scissors Forceps: Without teeth With teeth Dissecting forceps (Anatomical) With teeth: for tougher(hart) tissue: Fascia,Skin Without teeth: (atraumatic): for delicate tissues (empfindlich): Bowel Vessels. -

Surgical Products
Cervical & Endocervical Samplers Surgical Products Uterine Manipulation Devices Hysterectomy Instruments Laparoscopic Port-Site Closure Laparoscopic Instruments Laparoscopic Smoke Evacuation Laparoscopic Disposables Trocars Urology Instruments Retractors Delivering on the Promise to Help Clinicians Provide Better Health Care for Women Our mission is to enable physicians to provide increasingly more efficient and effective health care for women. We leverage our expertise in identifying and developing a steady stream of exceptional products that keep Ob/Gyns and others directly involved in caring for women, at the forefront of women’s health care. An Expansive Portfolio of Trusted Brands And Services Since our founding in 1990, CooperSurgical has researched, developed and manufactured a wide range of trusted brands that have advanced the standard of women’s health care. Our products are used by physicians and health care professionals in hospitals and their practices for a wide variety of procedures from basic annual gynecological exams to complex surgical procedures. As a full-service R&D and manufacturing company, we are committed to: • Improved patient outcomes and satisfaction • The highest quality and safety standards in the industry • Clinically proven technologies that provide ease of use • Technical support of our equipment – 20+ years of experience • Innovative solutions that reduce procedural costs • Annual support of medical professional educational organizations • Educational and in-service support of our products • Personalized service and a commitment to your satisfaction by educated professional representatives We appreciate the opportunity to partner with you to provide optimum health care for women. 2 To place an order, call us at: 800.243.2974 | Visit us online at: www.CooperSurgical.com About CooperSurgical Delivering on the Promise to Help Clinicians Provide Better Health Care for Women Industry-Leading Solutions for Laparoscopic and General Surgical Procedures CooperSurgical instruments are used every day in surgical procedures. -
Surgical Instruments
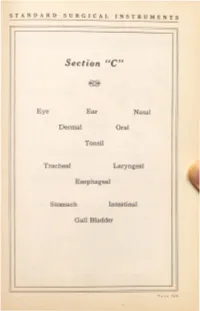
STANDARD SURGICAL INSTRUMENTS Section ''C'' Eye Ear Nasal Dermal Oral Tonsil Tracheal Laryngeal Esophageal Stomach Intestinal Gall Bladder ST ANDARD SURGICAL INSTRUMENTS C-10 C-30 C-40 - 3 Condensing Lenses, Illuminators, Ophthalmoscopes and Retinoscopes ·c- . <...onden ing Len~. 2 inches. hard rubber rim, 13 dtoptar. ·c ond n mg Len . double. 1:3 and dioptar. ·c- 1 ond n 'ng Len • \\ith metal rim and handle. ·c Dr . Berger's upc ''ith met I hea band. ·c- 9 Dr. Bez:ger's upe with \\ebbiog head band. C-10 Ocular Transilluminator. E .S.I.Co. ·c-11 Ophthalmoscope. Loring's, 1 len . "C-12 Oph halmoscope, loring's, lectrical, with mtrror, in ca . •c-13 Ophthalmoscope, Morton 's, lectrical. with mtrror. on battery hand! . · C- 14 Retinoscope ?o.lirror. r lain or conca c. 11 mch . regtlar hand! . ·c-1s Retinoscope Mtrror, r lain or conca e, 1Y2 inchc , folding handle ·c-1 R tino ope firror, Thor ington's, % inch. •C- 17 Retino · ope ftrror, T h or ington's, % inch, with folding cover ·c-1 Retinoscope, lectrical, on battery handle, in case. •C-19 Retinoscope and Ophthalmoscope, electrical, on battery handle, in case. ·c-20 Ashe tos Chimney, with iris dtaphragm. Eyelid Retractors C-30 Desrna rre's, 4 izes. ·c-a Fish er 's, lid hook, double. latest model. C-3 Fi h er 's, fen trated. flexibl for shaping. C-37 Fisher 's, solid, fl xiblc for haping. C- Fish er 's, for lov r ltd. C 0 Ziegler's, one size. P A CE 170 STANDARD SURGICAL INSTRUMENTS ( ,)() . -

49 How to Grasp the Needle with Needle
Basic Instrument Use Video Transcript How to Grasp the Needle with Needle Holders Placing a stitch requires a sequence of carefully planned steps. Each step, if performed incorrectly, contributes to the loss of precious operative time. Skilled surgeons do not necessarily suture with rapid hand motions, but use deliberate, disciplined steps that eliminate nonproductive motions during suturing. Novice surgeons must practice handling the needle holder and placing sutures in order to learn how to perform this technique pr operly and efficiently. In this video, we will examine the first step of placing a stitch, how to grasp the needle within the jaws of the needle holder. To grasp the needle in the needle holder, release the ratchet and open the jaws. The needle is positioned between the jaws, at the tip of the instrument, and is almost always held perpendicular to the axis of the jaws. This standard position allows for good needle stability and helps prevent bending. When the needle is held in this manner, the needle can be driven through tissue by merely rotating the holder on its axis. This minimizes the amount of motion needed to drive the needle, using less space to complete the stitch. When the needle is placed obliquely within the jaws, the handle of the holders must move through a wider arc to follow the curve of the needle through the tissue. There are few surgical situations in which oblique placement of the needle is required. When grasping the needle with needle holders, you will also need to plan where along the curve of the needle it should be grasped. -

Aesculap Spine Miaspas TL
Aesculap Spine Miaspas TL Spinal Microsurgical Endoscopy THORACOSCOPIC LAPAROSCOPIC CONTENTS PAGE INTRODUCTION 3 RONGEURS AND NUCLEUS-GRASPING FORCEPS 5 BONE PUNCHES 6 APPLICATION OF THE SLIDING TUBE 7 DISSECTORS AND EXPLORATION HOOKS 8 SCOOPS 9 CURETTES, OSTEOTOMES AND IMPACTORS 10 LUNG SPATULA AND RIB ELEVATOR 11 SPECULUM, DILATOR ROD, BONE-GRAFT-HOLDER AND BONE GRAFT MEASUREMENT INSTRUMENT 12 DRILL, BURRS AND HAND PIECE 13 TROCARS COMPLETE 14 TROCAR SYSTEM 16 BIPOLAR FORCEPS 17 FURTHER ENDOSCOPIC INSTRUMENTS AND MOTOR LINE EQUIPMENT SEE FOLLOWING LEAFLETS 18 AESCULAP SPINE PRODUCTS 19 2 SPINAL MICROSURGICAL ENDOSCOPY The miaspasTL instrument system was developed in co-operation with Daniel Rosenthal, MD. Praxisklinik Bad Homburg Hessenring 128 A 61348 Bad Homburg Germany to safely perform microsurgical endoscopic surgery on the thoracic and lumbar spine. Microsurgical endoscopy - as the name suggests - is a technique based on two of the most minimally invasive or least traumatic current techniques for spinal surgery. The miaspasTL instruments are designed with the surgeon in mind, to facilitate spinal microsurgical endoscopic procedures. Main advantages of the miaspasTL instrument system: ➠ microsurgical endoscopic technique promotes minimal patient trauma ➠ suitable for both laparoscopic (using gas insufflation) and thoracoscopic (gasless) procedures ➠ well balanced instrument design ensures easy handling ➠ high quality reusable instruments ensure cost savings ➠ instrumentation is easily disassembled for cleaning prior to sterilisation -

United States Patent (19) 11 Patent Number: 4,545,374 Jacobson 45 Date of Patent: Oct
United States Patent (19) 11 Patent Number: 4,545,374 Jacobson 45 Date of Patent: Oct. 8, 1985 54 METHOD AND INSTRUMENTS FOR PERFORMING A PERCUTANEOUS OTHER PUBLICATIONS LUMBAR DISKECTOMY "Nucleography”, May 1952, issue of Journal of Bone (76) Inventor: Robert E. Jacobson, 1295 NW. 14th and Joint Surgery, vol. 34B, No. 2. St., Suite G, Miami, Fla. 33125 "Dr. Parvas Kanbin Develops New Surgical Procedure Aiding Herniated Spinal Disk Sufferers', May 1982, 21) Appl. No.: 414,779 issue of Image, vol. 6, No. 5. 22) Filed: Sep. 3, 1982 "Microlumbar Discectomy', Feb. 1982, issue of Resi dent and Staff Physician. (51) Int. Cl." .............................................. A61B 17/00 52 U.S. C. ................................ 128/303 R; 128/305; "Oh, My Aching Back', p. D1, Saturday, Nov. 7, 1981, 128/312; 128/348.1; 604/164; 604/264 issue of The Miami Herald. 58) Field of Search .............. 128/348.1, 92 E, 92 EB, "Percutaneous Lumbar Discectomy', 1981, Dr. Robert 128/303 R, 753-754, 341-343, 345, 3, 126, E. Jacobson. 305.3, 741, 303.11, 303.13,783-784, 362; Primary Examiner-C. Fred Rosenbaum 604/22, 164-166, 264,904 Assistant Examiner-Gene B. Kartchner 56) References Cited Attorney, Agent, or Firm-Pennie & Edmonds U.S. PATENT DOCUMENTS (57) ABSTRACT 2,991,787 7/1961 Shelden et al. .................. 128/305.3 A method for percutaneously accessing the lumbar 3,308,819 3/1967 Arp ..................................... 604/164 region of the spinal column by laterally inserting a can 3,320,131 5/1967 Smith . nula through the patient's side above the pelvic crest to 3,320,948 5/1967 Martin .................................. -

Instruments 449-478 4/3/06 10:42 AM Page 449
Instruments_449-478 4/3/06 10:42 AM Page 449 Neuro Hammers & Diagnostic ADC® NEUROLOGICAL HAMMERS Four of the most popular hammers for diagnosis of neurological function. 369110105375 Buck Hammer, 7 1/4˝, Chrome Plated Handle w/2 sided rubber head, Handle Conceals “screw-in” Brush, Needle Contained Within The Head 369310105374 Taylor Hammer, 7 1/2˝, Chrome Handle w/triangular rubber head, Orange 3693BK10141795 Taylor Hammer, 7 1/2˝, Chrome Handle w/triangular rubber head, Black 3693DG10141796 Taylor Hammer, 7 1/2˝, Chrome Handle w/triangular rubber head, Dark Green 3693RB10141797 Taylor Hammer, 7 1/2˝, Chrome Handle w/triangular rubber head, ADC® TUNING FORKS Royal Blue 369510105372 Wartenberg Pinwheel, 7 1/2˝, Stainless Steel Handle w/textured grip, Non magnetic, corrosion resistant aluminum alloy construction weighs 1/3 of Rotating Spur comparable steel tuning forks. Produced from 3/8˝ x 1˝ bar stock for superior 369710105373 Babinski Hammer, 8 1/2˝, Octagonal Stainless Steel Handle w/concealed performance and consistent frequency accuracy. Extra long 2˝ handle of turned needle, Rubber Head smooth aluminum to facilitate bone conduction tests. 50012810105366 Tuning Fork w/fixed weight, 128cps Frequency 50025610105367 Tuning Fork w/fixed weight, 256cps Frequency 50051210105368 Tuning Fork w/o weight, 512cps Frequency 50102410105369 Tuning Fork w/o weight, 1024cps Frequency 50204810105370 Tuning Fork w/o weight, 2048cps Frequency 50409610105371 Tuning Fork w/o weight, 4096cps Frequency 1-200 1-220 MILTEX HAMMERS 1-20010090643 Taylor Percussion -
Fine Surgical Instruments for Research™ Hsin-Yi Road, Sec
INTERNATIONAL Scissors, Bone Instruments Fine Science Tools Inc. & Scalpels 202-277 Mountain Highway pages 3–61 North Vancouver, British Columbia Canada V7J 3T6 Telephone 800-665-5355 / 604-980-2481 Fax 800-665-4544 / 604-987-3299 E-Mail [email protected] Web finescience.ca Fine Science Tools (USA) Inc. 373-G Vintage Park Drive F Forceps & Hemostats Foster City, California 94404-1139 I pages 63–97 Telephone 800-521-2109 / 650-349-1636 N Fax 800-523-2109 / 650-349-3729 E E-Mail [email protected] Web finescience.com S C I E Fine Science Tools GmbH N Vangerowstraße 14 C 69115 Heidelberg Germany E Telephone +49 (0) 62 21 - 90 50 50 Fax +49 (0) 62 21 - 90 50 590 T Probes, Needle Holders, O E-Mail [email protected] Thread, Retractors & Clamps Web finescience.de O pages 99–133 L S InterFocus Ltd. Pentagon Business Park Cambridge Road Linton, Cambridge CB21 4NN C United Kingdom A Telephone +44 (0)1223 894833 T Fax +44 (0)1223 894235 A Surgical & Laboratory E-Mail [email protected] L Accessories Web surgicaltools.co.uk O pages 135–161 G 2 Muromachi Kikai Co., Ltd. 0 4-2-12, Nihonbashi-Muromachi 1 Chuo-ku 4 Tokyo 103-0022 Japan Telephone (03) 3241-2444 Fax (03) 3241-2940 E-Mail [email protected] Student Quality Instruments Web muromachi.com pages 163–167 Proserv Instruments Co., Ltd. 7F-2, No. 413 Fine Surgical Instruments for Research™ Hsin-Yi Road, Sec. 4 Taipei, Taiwan R.O.C. Telephone (02) 27230455 Fax (02) 27230799 2014 E-Mail [email protected] Web proserv.com.tw TABLE OF CONTENTS | CATALOG 2014 Scissors 3 – 37 Spring 3 – 14 WE PROUDLY STOCK Fine 15 – 30 Surgical 31 – 37 Bone Instruments 38 – 51 DUMONT® Rongeurs 38 – 41 A selection of over 50 of the most popular Cutters 42 – 49 Other Bone Instruments 50 Dumont forceps are offered in this catalog.