Intratympanic Membrane Cholesteotoma: an Unusual Rare Case
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: a Clinical Study
Int Adv Otol 2014; 10(2): 102-6 • DOI: 10.5152/iao.2014.40 Original Article A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: A Clinical Study Can Özbay, Rıza Dündar, Erkan Kulduk, Kemal Fatih Soy, Mehmet Aslan, Hüseyin Katılmış Department of Otorhinolaryngology, Şifa University Faculty of Medicine, İzmir, Turkey (CÖ) Department of Otorhinolaryngology, Mardin State Hospital, Mardin, Turkey (RD, EK, KFS, MA) Department of Otorhinolaryngology, Katip Çelebi University Atatürk Training and Research Hospital, İzmir, Turkey (HK) OBJECTIVE: Myringosclerosis (MS) is a pathological condition characterized by hyaline degeneration and calcification of the collagenous structure of the fibrotic layer of the tympanic membrane, which may develop after trauma, infection, or inflammation as myringotomy, insertion of a ventila- tion tube, or myringoplasty. The aim of our study was to both reveal and evaluate the impact of the factors that might be effective on the post-tym- panoplasty development of myringosclerosis in the graft. MATERIALS and METHODS: In line with this objective, a total of 108 patients (44 males and 64 females) aged between 11 and 66 years (mean age, 29.5 years) who had undergone type 1 tympanoplasty (TP) with an intact canal wall technique and type 2 TP, followed up for an average of 38.8 months, were evaluated. In the presence of myringosclerosis, in consideration of the tympanic membrane (TM) quadrants involved, the influential factors were analyzed in our study, together with the development of myringosclerosis, including preoperative factors, such as the presence of myringosclerosis in the residual and also contralateral tympanic membrane, extent and location of the perforation, and perioperative factors, such as tympanosclerosis in the middle ear and mastoid cavity, cholesteatoma, granulation tissue, and type of the operation performed. -
Tympanic Membrane Perforations: the Safe Versus the Unsafe
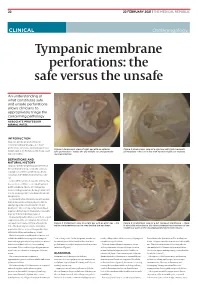
TMR_210222_22 2021-02-12T14:56:54+11:00 22 22 FEBRUARY 2021 | THE MEDICAL REPUBLIC CLINICAL Otolaryngology Tympanic membrane perforations: the safe versus the unsafe An understanding of what constitutes safe and unsafe perforations allows clinicians to appropriately triage the concerning pathology ASSOCIATE PROFESSOR NIRMAL PATEL INTRODUCTION Tympanic membrane perforations are seen frequently in general practice. Some perforations can be associated with significant Figure 1: Endoscopic view of right ear with an anterior Figure 2: Endoscopic view of a right ear with twin traumatic disease, such as cholesteatoma which may cause safe perforation – notice the dry middle ear and posterior perforations – the ear is dry with normal middle ear mucosa. major morbidity. myringosclerosis DEFINITIONS AND NATURAL HISTORY Tympanic membrane perforations are holes in the ear drum that most commonly occur as a consequence of either ear infections, chronic eustachian tube dysfunction or trauma to the ear. Acute middle ear infection (acute otitis media) is a common condition occurring at least once in 80% of children. Most acute otitis media resolves with spontaneous discharge of infected secretions through the eustachian tube into the nasopharynx. Occasionally when the infections are frequent, there is extensive scarring (tympanosclerosis and myringosclerosis) of the ear drum and middle ear . This scarring compromises blood supply to the healing ear drum and occasionally stops the hole from healing. (Figure 1) Traumatically induced holes occur from a rapid compression of the air column in the external ear canal, most commonly from a blow to the Figure 3: Endoscopic view of a right ear with an attic wax – the Figure 4: Endoscopic view of a left tympanic membrane – there white cholesteatoma can be seen behind the ear drum. -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Hearing Loss, Vertigo and Tinnitus
HEARING LOSS, VERTIGO AND TINNITUS Jonathan Lara, DO April 29, 2012 Hearing Loss Facts S Men are more likely to experience hearing loss than women. S Approximately 17 percent (36 million) of American adults report some degree of hearing loss. S About 2 to 3 out of every 1,000 children in the United States are born deaf or hard-of-hearing. S Nine out of every 10 children who are born deaf are born to parents who can hear. Hearing Loss Facts S The NIDCD estimates that approximately 15 percent (26 million) of Americans between the ages of 20 and 69 have high frequency hearing loss due to exposure to loud sounds or noise at work or in leisure activities. S Only 1 out of 5 people who could benefit from a hearing aid actually wears one. S Three out of 4 children experience ear infection (otitis media) by the time they are 3 years old. Hearing Loss Facts S There is a strong relationship between age and reported hearing loss: 18 percent of American adults 45-64 years old, 30 percent of adults 65-74 years old, and 47 percent of adults 75 years old or older have a hearing impairment. S Roughly 25 million Americans have experienced tinnitus. S Approximately 4,000 new cases of sudden deafness occur each year in the United States. Hearing Loss Facts S Approximately 615,000 individuals have been diagnosed with Ménière's disease in the United States. Another 45,500 are newly diagnosed each year. S One out of every 100,000 individuals per year develops an acoustic neurinoma (vestibular schwannoma). -

Neurootological Evaluation of Tinnitus
International Tinnitus Journal 1, 93-97 (1995) Neurootological Evaluation of Tinnitus J. c. R. Seabra, M.D., H. Diamantino, M.D., J. Faria e Almeida, M.D. Ear, Nose and Throat Department, Vila Nova de Gaia, Portugal Abstract: We analyse the neurootological data of patients attended in the Ear, Nose and Throat (E.N.T.) department of the Centro Hospitalar de Vila Nova de Gaia for a tinnitus problem. We submitted these patients to our neurootological routine evaluation. This approach is justified in a tinnitus patient because the cochleovestibular system is a unit and acts as a whole. We characterise the population that came to us by sex and mean age. The profile of these patients is then analysed by our neurootological routine evaluation, which comprises the history taking and audiometric as well as equilibriometric investigations. The results of the audiovestibulometric examinations - pure tone audiometry, vocal audiometry, and Brain Evoked Response Audiometry (B.E.R.A.), Cranio-Corpo Graphy (C.C.G.), Electronystagmography (E.N.G.) - are discussed. We concluded that many tinnitus patients, even those who had no vestibular symptoms, showed some disturbances in the vestibular tests. This fact highlights the need for a complete cochleovestibular investigation in all patients complaining about tinnitus. INTRODUCTION middle ear disease, such as chronic otitis, tympanic perforations, or tympanosclerosis. innitus is a widespread symptom that mortifies We investigated 44 patients, 19 men and 25 women, with T patients and frustrates doctors. It may be the only a mean age of 48-years (standard deviation being 12). symptom complained by patients, but commonly The patients underwent our routine neurootological it is associated with neurosensory hearing loss and/or examination which comprises: vertigo. -

Differential Diagnosis and Treatment of Hearing Loss JON E
Differential Diagnosis and Treatment of Hearing Loss JON E. ISAACSON, M.D., and NEIL M. VORA, M.D., Milton S. Hershey Medical Center, Hershey, Pennsylvania Hearing loss is a common problem that can occur at any age and makes verbal communication difficult. The ear is divided anatomically into three sections (external, middle, and inner), and pathology contributing to hearing loss may strike one or more sections. Hearing loss can be cat- egorized as conductive, sensorineural, or both. Leading causes of conductive hearing loss include cerumen impaction, otitis media, and otosclerosis. Leading causes of sensorineural hear- ing loss include inherited disorders, noise exposure, and presbycusis. An understanding of the indications for medical management, surgical treatment, and amplification can help the family physician provide more effective care for these patients. (Am Fam Physician 2003;68:1125-32. Copyright© 2003 American Academy of Family Physicians) ore than 28 million Amer- tive, the sound will be heard best in the icans have some degree of affected ear. If the loss is sensorineural, the hearing impairment. The sound will be heard best in the normal ear. differential diagnosis of The sound remains midline in patients with hearing loss can be sim- normal hearing. Mplified by considering the three major cate- The Rinne test compares air conduction gories of loss. Conductive hearing loss occurs with bone conduction. The tuning fork is when sound conduction is impeded through struck softly and placed on the mastoid bone the external ear, the middle ear, or both. Sen- (bone conduction). When the patient no sorineural hearing loss occurs when there is a longer can hear the sound, the tuning fork is problem within the cochlea or the neural placed adjacent to the ear canal (air conduc- pathway to the auditory cortex. -

Fitting Strategies for Patients with Conductive Or Mixed Hearing Loss
12843.C10.PGS 3/8/02 11:12 AM Page 272 10 Fitting Strategies for Patients with Conductive or Mixed Hearing Loss JOEL GOEBEL, MICHAEL VALENTE, MAUREEN VALENTE, JANE ENRIETTO, KAREN M. LAYTON, MARK S. WALLACE Introduction Bone conduction aids were once the main- stay of amplification technology for CHL. Surgical correction of conductive hearing These bone conduction devices, however, loss (CHL) is the principal and preferred have been superseded by newer technology treatment by most patients. Surgical therapy [i.e., bone-anchored hearing aid (BAHA®)]. is successful in the majority of cases, but not The use of conventional or programmable all patients are candidates for surgery be- air-conduction aids and implantable bone- cause of medical, anatomic, or personal rea- conduction hearing devices is emphasized sons. Although most who undergo an oto- in this chapter. logic operation achieve socially adequate There are a variety of causes of hearing hearing [i.e., speech recognition threshold loss. It is important for all members of the (SRT) of 25-dB hearing level (HL) or less], hearing health care team (otolaryngologists, some do not, and these patients can gener- audiologists, and aural rehabilitation spe- ally obtain additional benefit from amplifica- cialists) to fully understand the mechanisms tion. In cases of CHL in only hearing ear, the of both conductive and sensorineural com- surgeon recommends amplification to avoid ponents in each individual case and develop the risk of surgical complications that might an optimal rehabilitative strategy. In cases increase the hearing loss, provided that the with a significant conductive component, CHL is not the result of a progressive disor- many factors must be weighed. -

Factors Potentially Affecting the Hearing of Petroleum Industry Workers
report no. 5/05 factors potentially affecting the hearing of petroleum industry workers Prepared for CONCAWE’s Health Management Group by: P. Hoet M. Grosjean Unité de toxicologie industrielle et pathologie professionnelle Ecole de santé publique Faculté de médecine Université catholique de Louvain (Belgium) C. Somaruga School of Occupational Health University of Milan (Italy) Reproduction permitted with due acknowledgement © CONCAWE Brussels June 2005 I report no. 5/05 ABSTRACT This report aims at giving an overview of the various factors that may influence the hearing of petroleum industry workers, including the issue of ‘ototoxic’ chemical exposure. It also provides guidance for occupational physicians on factors that need to be considered as part of health management programmes. KEYWORDS hearing, petroleum industry, hearing loss, audiometry, ototoxicity, chemicals INTERNET This report is available as an Adobe pdf file on the CONCAWE website (www.concawe.org). NOTE Considerable efforts have been made to assure the accuracy and reliability of the information contained in this publication. However, neither CONCAWE nor any company participating in CONCAWE can accept liability for any loss, damage or injury whatsoever resulting from the use of this information. This report does not necessarily represent the views of any company participating in CONCAWE. II report no. 5/05 CONTENTS Page SUMMARY IV 1. INTRODUCTION 1 2. HEARING, MECHANISMS AND TYPES OF HEARING LOSS 3 2.1. PHYSIOLOGY OF HEARING: HEARING BASICS 3 2.2. MECHANISMS AND TYPES OF HEARING LOSS 4 2.2.1. Transmission or conduction hearing loss 4 2.2.2. Sensorineural hearing loss 5 2.3. EVALUATION OF HEARING LOSS 6 3. -

Tympanosclerosis Definition
Tympanosclerosis Definition • Tympanosclerosis (TS): calcification and hardening of tissue in the eardrum and middle ear • Unclear etiology but cause may include: • Long-term otitis media • Atherosclerosis • Insertion of tympanostomy tube Epidemiology • 5% among pediatric otolaryngology clinic visits • In 23%-40% of children who had glue ear (a fluid filled middle ear) or prior tympanostomy tubes. • Recent increase in incidence could be due to increased awareness and detection Classification • Myringosclerosis calcification only within the tympanic membrane usually less extensive than tympanosclerosis • Intratympanic tympanosclerosis when occurring at other location within the middle ear including the ossicular chain, middle ear mucosa or the mastoid cavity Signs and Symptoms • Myringosclerosis: Generally asymptomatic without hearing loss • Tympanosclerosis: Can result in significant hearing loss. However, hearing loss can often be completely reversed or improve with treatment Common History Findings • Patients with prior myringotomy and tube placement are at increased risk of TS or MS • Prolonged otitis media also increases risk for TS Tympanosclerosis (video) Tympanosclerosis appears as a chalky white material within the eardrum substance. Dense sclerosis, causes eardrum thickening and may involve the ossicles with impairment of hearing. (play video to see otoscopy findings) Tympanosclerosis Note the characteristic chalky white calcification of the tympanic membranes shown above. http://me.hawkelibrary.com/new/main.php?g2_itemId=1744 -

Hearing Loss in Tympanosclerosis
International Journal of Science and Research (IJSR) ISSN (Online): 2319-7064 Index Copernicus Value (2013): 6.14 | Impact Factor (2014): 5.611 Hearing Loss in Tympanosclerosis K S Munish1, B S Mamatha2, A M Shivakumar3 1Associate Professor, Department of Otorhinolaryngology, SSIMS&RC, Davangere 2Postgraduate student, Department of Otorhinolaryngology, SSIMS&RC, Davangere 3Professor and Head of Department of Otorhinolaryngology, SSIMS&RC, Davangere Abstract: Objectives: To study hearing loss in tympanosclerosis with intact membrane. Materials and Methods: 30 cases of tympanosclerosis with intact tympanic membrane in age15-50 year . Clinical and audiological evaluation done. The involvement of tympanic membrane and degree of hearing loss noted. Results: 30 patients 16 male and 14 female. Agewise 15-20 yrs, 21-30yrs, 31 -40 yrs, 41-50yrs was 5, 17, 5, 3cases respectively. According to the site, anterosuperior -4, anteroinferior - 6, posterosuperior – 5, , posteroinferior - 4, anterior 04, posterior 3, inferior 03, and whole tympanic membrane- 1 Tuning fork test : 20 had conducting hearing loss and 10 had normal hearing. On PTA, anterosuperior 18-20 db, anteroinferior 20-30 db, posterosuperior 20 -40 db, postero inferior 20-30 db, anteriorly 20-30 db, posteriorly 30-40db, inferiorly 20-30db and whole tympanic membrane 40db conducting hearing loss. Conclusion: Conductive hearing loss occur with myingosclerosis. common age group is 21-30 years. tympanosclerosis maximum in anteroinferior quadrant, maximum hearing loss with posterosuperior, posterior and whole tympanic membrane. Keywords: tympanosclerosis, hearing loss, tympanic membrane, pure tone audiogram 1. Introduction quaudrant- 5 patient, posteroinferior quadrant- 4patient, anterior 04, posterior 3, inferior 03, and all quarant 1 in pars Tympanosclerosis is an abnormal condition of the middle tensa. -

Secondary Middle-Ear Damages in Patients with Head and Neck
arm Ph ac f ov l o i a g n il r a n u c Huong et al., J Pharmacovigil 2018,S4 o e J Journal of Pharmacovigilance DOI: 10.4172/2329-6887.1000S4-002 ISSN: 2329-6887 Research Article Article OpenOpen Access Access Secondary Middle-ear Damages in Patients with Head and Neck Cancer after Radiotherapy Huong LD1, Nguyen LP1* and Nguyen HX2 1Department of Otorhinolaryngology, Military Medical 103 Hospital, Le Huu Trac Medical Pharmaceutical University, Vietnam 2Department of Pharmaceutical Sciences, College of Pharmacy, Mercer University, Atlanta, USA Abstract Objective: This study aimed to evaluate the relationship between radiotherapy and Eustachian tube dysfunction, and to investigate the efficacy of treatments by tympanostomy and grommet insertion. Methods: Patients with head and neck cancer (148 patients) were treated by three–dimensional radiotherapy in the Center of Oncology and Nuclear Medicine, Military Medical 103 Hospital from February 2014 to April 2016. All patients underwent an ear examination (otoscopy), audiometry, and tympanometry test. Those who developed otitis media with effusion and tympanosclerosis were then treated by tympanostomy or myringotomy. Results: The most common complication after the radiotherapy was found to be Eustachian tube dysfunction, especially otitis media with effusion and tympanosclerosis. Thus, carefully examining and closely monitoring need to be performed to detect patients with secondary middle-ear damages, to successfully cure post-radiotherapy otitis media with effusion, and to minimize possible injury to the middle ear and Eustachian tube. Also, tympanostomy and myringotomy were reported to be the preferable treatments due to their simplicity, high quality, and patients’ compliance. Conclusion: Eustachian tube dysfunction after radiotherapy treatment was the cause for otitis media with effusion and tympanosclerosis. -

Goh -CONDUCTIVE HEARING LOSS FINAL Version.Pptx
ASHNR 2016 ASHNR 2016 CONDUCTIVE HEARING LOSS DR JULIAN GOH DIAGNOSTIC RADIOLOGY TAN TOCK SENG HOSPITAL SINGAPORE ASHNR 2016 ASHNR 2016 Ossicles: fused / disrupted / absent / malformaon rd Dehiscence – 3 window Fluid or so ssue Vascular structures Abnormal interface with inner ear (oval / round windows) DECLARATIONS - NIL IP-III Bone, so ssue, cerumen ASHNR 2016 ASHNR 2016 IMAGING TECHNIQUES CT MSCT / CBCT • Double oblique • Wide window sengs WIDE WINDOWS MRI Pre & post contrast + DWI • Congenital cholesteatoma NARROW (BONE) • Cholesterol granulomas WINDOWS www.teachmesurgery.co • So; <ssue masses (extent, perineural spread) m ASHNR 2016 ASHNR 2016 EPITYMPANUM CHL – MIDDLE EAR PERFORATED INTACT TM TM EAC MESOTYMPANUM EUSTACHIAN NORMAL TUBE INFLAMMATION RED HYPOTYMPANUM TRAUMA WHITE BLUE ASHNR 2016 ASHNR 2016 INTACT TM - NORMAL CONGENITAL OSSICULAR CHAIN ANOMALIES • Usually in associaon with EAC anomalies • Isolated anomalies (with normal external ear) much less common1 • • Chronic effusions (chronic OME, Lack of progression, early age of onset dis<nguish from fenestral otosclerosis NPC) • Unilateral (sporadic) / bilateral (gene<c, AD) • Congenital ossicular anomalies Ossicular deformity: abnormal size, shape, • Oval window atresia orientaon • Otosclerosis Ossicular fixaon: bony bar from ossicles to middle ear wall Courtesy Berit Verbist, Leiden Courtesy Berit Verbist, Leiden Swartz JD, Harnsberger HR. Imaging of the Temporal Bone, 3rd edi<on. New York: Thieme 1998 ASHNR 2016 ASHNR 2016 OSSICULAR DEFORMITIES UNICRURAL STAPES CONGENITAL THICKENING