Overview Auditory Problems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: a Clinical Study
Int Adv Otol 2014; 10(2): 102-6 • DOI: 10.5152/iao.2014.40 Original Article A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: A Clinical Study Can Özbay, Rıza Dündar, Erkan Kulduk, Kemal Fatih Soy, Mehmet Aslan, Hüseyin Katılmış Department of Otorhinolaryngology, Şifa University Faculty of Medicine, İzmir, Turkey (CÖ) Department of Otorhinolaryngology, Mardin State Hospital, Mardin, Turkey (RD, EK, KFS, MA) Department of Otorhinolaryngology, Katip Çelebi University Atatürk Training and Research Hospital, İzmir, Turkey (HK) OBJECTIVE: Myringosclerosis (MS) is a pathological condition characterized by hyaline degeneration and calcification of the collagenous structure of the fibrotic layer of the tympanic membrane, which may develop after trauma, infection, or inflammation as myringotomy, insertion of a ventila- tion tube, or myringoplasty. The aim of our study was to both reveal and evaluate the impact of the factors that might be effective on the post-tym- panoplasty development of myringosclerosis in the graft. MATERIALS and METHODS: In line with this objective, a total of 108 patients (44 males and 64 females) aged between 11 and 66 years (mean age, 29.5 years) who had undergone type 1 tympanoplasty (TP) with an intact canal wall technique and type 2 TP, followed up for an average of 38.8 months, were evaluated. In the presence of myringosclerosis, in consideration of the tympanic membrane (TM) quadrants involved, the influential factors were analyzed in our study, together with the development of myringosclerosis, including preoperative factors, such as the presence of myringosclerosis in the residual and also contralateral tympanic membrane, extent and location of the perforation, and perioperative factors, such as tympanosclerosis in the middle ear and mastoid cavity, cholesteatoma, granulation tissue, and type of the operation performed. -
HEARING LOSS, DEAFNESS Ear32 (1)
HEARING LOSS, DEAFNESS Ear32 (1) Hearing Loss, Deafness Last updated: May 11, 2019 CLASSIFICATION, DIAGNOSIS ................................................................................................................. 1 METHODS OF COMMUNICATION FOR DEAF ............................................................................................ 2 MANAGEMENT ......................................................................................................................................... 2 HEARING AIDS (S. AMPLIFICATION) ....................................................................................................... 2 COCHLEAR IMPLANTS ............................................................................................................................ 2 AUDITORY BRAINSTEM IMPLANTS .......................................................................................................... 4 PREVENTION .......................................................................................................................................... 4 PEDIATRIC HEARING DEFICITS ............................................................................................................... 4 ETIOLOGY .............................................................................................................................................. 4 DIAGNOSIS ............................................................................................................................................. 6 TREATMENT .......................................................................................................................................... -

Hearing Loss in Patients with Extracranial Complications of Chronic Otitis Media
ORIGINAL ARTICLE Hearing loss in patients with extracranial complications of chronic otitis media Authors’ Contribution: BCDE AF A – Study Design Tomasz Przewoźny , Jerzy Kuczkowski B – Data Collection C – Statistical Analysis D – Data Interpretation Department of Otolaryngology, Medical University of Gdańsk, Gdańsk, Poland E – Manuscript Preparation F – Literature Search G – Funds Collection Article history: Received: 13.04.2017 Accepted: 10.04.2017 Published: 15.06.2017 ABSTRACT: Objective: A pure tone audiomety analysis of patients with extracranial complications of chronic suppurative otitis media (ECCSOM). Material and methods: We retrospectively analyzed audiometric data performed before treatment from 63 pa- tients with ECCSOM (56 single, 7 multiple complications) including groups of frequencies. Results: The greatest levels of hearing loss were noted for 6 and 8 kHz (79.0 and 75.7 dBHL) and for the frequency groups high tone average (76.1 dBHL). As regards the severity of hearing impairment in pure tone average the prev- alence of complications was as follows: labyrinthitis (77.8±33.6 dBHL), facial palsy (57.1±14.3 dBHL), perilymphatic fistula (53.9±19.9 dBHL) and mastoiditis (42.2±9.5 dBHL) (p=0.023). Conclusions: Hearing loss in ECCSOM is dominated by mixed, high-tone, moderate type of hearing loss, most pro- found in labyrinthitis. In 11% of patients the complication causes total deafness. KEYWORDS: chronic suppurative otitis media, complications extracranial, hearing loss INTRODUCTION ing discharge from the ear and mixed or conductive hearing loss can be observed [4-5]. Labyrinthitis is associated with Chronic suppurative otitis media (CSOM) is a destructive slowly progressive high-frequency sensorineural hearing loss disease of the ear. -

Changes in the Three-Dimensional Angular Vestibulo-Ocular Reflex Following Intratympanic Gentamicin for Menieres Disease
JARO 03: 430±443 82002) DOI: 10.1007/s101620010053 JARO Journal of the Association for Research in Otolaryngology Changes in the Three-Dimensional Angular Vestibulo-Ocular Re¯ex following Intratympanic Gentamicin for MeÂnieÁre's Disease 1 1±3 4,5 1 JOHN P. CAREY, LLOYD B. MINOR, GRACE C.Y. PENG, CHARLES C. DELLA SANTINA, 6 7 PHILLIP D. CREMER, AND THOMAS HASLWANTER 1 1Department of Otolaryngology±Head and Neck Surgery, Johns Hopkins University, Baltimore, MD 21287, USA 2Department of Biomedical Engineering, Johns Hopkins University, Baltimore, MD 21205, USA 3Department of Neuroscience, Johns Hopkins University, Baltimore, MD 21205, USA 4Department of Neurology, Johns Hopkins University, Baltimore, MD 21287, USA 1 5Department of Biomedical Engineering, Catholic University of America, Washington, DC 20064, USA 6Eye and Ear Research Unit, Institute of Clinical Neurosciences, Royal Prince Alfred Hospital, Sydney, Australia 7Department of Neurology, ZuÈrich University Hospital, ZuÈrich, Switzerland Received: 19 June 2000; Accepted: 21 January 2002; Online publication: 26 March 2002 ABSTRACT these gain values and those for head thrusts that ex- cited the contralateral canals were <2%. In contrast, The 3-dimensional angular vestibulo-ocular re¯exes caloric asymmetries averaged 40% 32%. Intra- 8AVOR) elicited by rapid rotary head thrusts were tympanic gentamicin resulted in decreased gains studied in 17 subjects with unilateral MeÂnieÁre's attributable to each canal on the treated side: disease before and 2±10 weeks after treatment with 0.40 0.12 8HC), 0.35 0.14 8AC), 0.31 0.14 8PC) intratympanic gentamicin and in 13 subjects after 8p < 0.01). However, the gains attributable to con- surgical unilateral vestibular destruction 8SUVD). -

Hearing Loss Due to Myringotomy and Tube Placement and the Role of Preoperative Audiograms
ORIGINAL ARTICLE Hearing Loss Due to Myringotomy and Tube Placement and the Role of Preoperative Audiograms Mark Emery, MD; Peter C. Weber, MD Background: Postoperative complications of myrin- erative and postoperative sensorineural and conductive gotomy and tube placement often include otorrhea, tym- hearing loss. panosclerosis, and tympanic membrane perforation. How- ever, the incidence of sensorineural or conductive hearing Results: No patient developed a postoperative sensori- loss has not been documented. Recent efforts to curb the neural or conductive hearing loss. All patients resolved use of preoperative audiometric testing requires docu- their conductive hearing loss after myringotomy and tube mentation of this incidence. placement. There was a 1.3% incidence of preexisting sen- sorineural hearing loss. Objective: To define the incidence of conductive and sensorineural hearing loss associated with myrin- Conclusions: The incidence of sensorineural or con- gotomy and tube placement. ductive hearing loss after myringotomy and tube place- ment is negligible and the use of preoperative audiomet- Materials and Methods: A retrospective chart re- ric evaluation may be unnecessary in selected patients, view of 550 patients undergoing myringotomy and tube but further studies need to be done to corroborate this placement was performed. A total of 520 patients under- small data set. going 602 procedures (1204 ears), including myrin- gotomy and tube placement, were assessed for preop- Arch Otolaryngol Head Neck Surg. 1998;124:421-424 TITIS MEDIA (OM) is one erative hearing status and whether it has of the most frequent dis- either improved or remained stable after eases of childhood, af- MTT. A recent report by Manning et al11 fecting at least 80% of demonstrated a 1% incidence of preop- children prior to school erative sensorineural hearing loss (SNHL) Oentry.1-4 Because of the high incidence of in children undergoing MTT. -

Pediatric Sensorineural Hearing Loss, Part 2: Syndromic And
Published May 19, 2011 as 10.3174/ajnr.A2499 Pediatric Sensorineural Hearing Loss, Part 2: REVIEW ARTICLE Syndromic and Acquired Causes B.Y. Huang SUMMARY: This article is the second in a 2-part series reviewing neuroimaging in childhood SNHL. C. Zdanski Previously, we discussed the clinical work-up of children with hearing impairment, the classification of inner ear malformations, and congenital nonsyndromic causes of hearing loss. Here, we review and M. Castillo illustrate the most common syndromic hereditary and acquired causes of childhood SNHL, with an emphasis on entities that demonstrate inner ear abnormalities on cross-sectional imaging. Syndromes discussed include BOR syndrome, CHARGE syndrome, Pendred syndrome, Waardenburg syndrome, and X-linked hearing loss with stapes gusher. We conclude the article with a review of acquired causes of childhood SNHL, including infections, trauma, and neoplasms. ABBREVIATIONS: BOR ϭ branchio-oto-renal; CISS ϭ constructive interference in steady state; IAC ϭ internal auditory canal; NF-2 ϭ neurofibromatosis type II; SCC ϭ semicircular canal; SNHL ϭ sensorineural hearing loss; T1WI ϭ T1-weighted image; T2 WI ϭ T2-weighted image he estimated prevalence of SNHL in patients younger than Table 1: Selected hereditary syndromes commonly associated with 1 T18 years of age is 6 per 1000, making it one of the leading SNHL causes of childhood disability and a common reason for oto- Inner Ear Malformations on Inner Ear Malformations laryngology referrals. Cross-sectional imaging is now rou- Imaging Not Common on Imaging tinely performed in these patients because it provides impor- Alagille syndrome Alport syndrome tant information about potential etiologies for hearing loss, Branchio-oto-renal syndrome Biotinidase deficiency defines the anatomy of the temporal bone and the central au- CHARGE syndrome Jervell and Lange-Nielsen syndrome ditory pathway, and identifies additional intracranial abnor- Klippel-Feil syndrome Norrie syndrome malities that may require further work-up. -
Tympanic Membrane Perforations: the Safe Versus the Unsafe
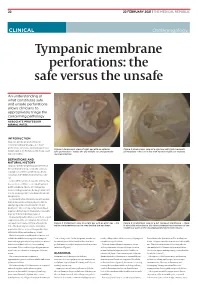
TMR_210222_22 2021-02-12T14:56:54+11:00 22 22 FEBRUARY 2021 | THE MEDICAL REPUBLIC CLINICAL Otolaryngology Tympanic membrane perforations: the safe versus the unsafe An understanding of what constitutes safe and unsafe perforations allows clinicians to appropriately triage the concerning pathology ASSOCIATE PROFESSOR NIRMAL PATEL INTRODUCTION Tympanic membrane perforations are seen frequently in general practice. Some perforations can be associated with significant Figure 1: Endoscopic view of right ear with an anterior Figure 2: Endoscopic view of a right ear with twin traumatic disease, such as cholesteatoma which may cause safe perforation – notice the dry middle ear and posterior perforations – the ear is dry with normal middle ear mucosa. major morbidity. myringosclerosis DEFINITIONS AND NATURAL HISTORY Tympanic membrane perforations are holes in the ear drum that most commonly occur as a consequence of either ear infections, chronic eustachian tube dysfunction or trauma to the ear. Acute middle ear infection (acute otitis media) is a common condition occurring at least once in 80% of children. Most acute otitis media resolves with spontaneous discharge of infected secretions through the eustachian tube into the nasopharynx. Occasionally when the infections are frequent, there is extensive scarring (tympanosclerosis and myringosclerosis) of the ear drum and middle ear . This scarring compromises blood supply to the healing ear drum and occasionally stops the hole from healing. (Figure 1) Traumatically induced holes occur from a rapid compression of the air column in the external ear canal, most commonly from a blow to the Figure 3: Endoscopic view of a right ear with an attic wax – the Figure 4: Endoscopic view of a left tympanic membrane – there white cholesteatoma can be seen behind the ear drum. -
Instruction Sheet: Otitis Externa
University of North Carolina Wilmington Abrons Student Health Center INSTRUCTION SHEET: OTITIS EXTERNA The Student Health Provider has diagnosed otitis externa, also known as external ear infection, or swimmer's ear. Otitis externa is a bacterial/fungal infection in the ear canal (the ear canal goes from the outside opening of the ear to the eardrum). Water in the ear, from swimming or bathing, makes the ear canal prone to infection. Hot and humid weather also predisposes to infection. Symptoms of otitis externa include: ear pain, fullness or itching in the ear, ear drainage, and temporary loss of hearing. These symptoms are similar to those caused by otitis media (middle ear infection). To differentiate between external ear infection and middle ear infection, the provider looks in the ear with an instrument called an otoscope. It is important to distinguish between the two infections, as they are treated differently: External otitis is treated with drops in the ear canal, while middle ear infection is sometimes treated with an antibiotic by mouth. MEASURES YOU SHOULD TAKE TO HELP TREAT EXTERNAL EAR INFECTION: 1. Use the ear drops regularly, as directed on the prescription. 2. The key to treatment is getting the drops down into the canal and keeping the medicine there. To accomplish this: Lie on your side, with the unaffected ear down. Put three to four drops in the infected ear canal, then gently pull the outer ear back and forth several times, working the medicine deeper into the ear canal. Remain still, good-ear-side-down for about 15 minutes. -

Consultation Diagnoses and Procedures Billed Among Recent Graduates Practicing General Otolaryngology – Head & Neck Surger
Eskander et al. Journal of Otolaryngology - Head and Neck Surgery (2018) 47:47 https://doi.org/10.1186/s40463-018-0293-8 ORIGINALRESEARCHARTICLE Open Access Consultation diagnoses and procedures billed among recent graduates practicing general otolaryngology – head & neck surgery in Ontario, Canada Antoine Eskander1,2,3* , Paolo Campisi4, Ian J. Witterick5 and David D. Pothier6 Abstract Background: An analysis of the scope of practice of recent Otolaryngology – Head and Neck Surgery (OHNS) graduates working as general otolaryngologists has not been previously performed. As Canadian OHNS residency programs implement competency-based training strategies, this data may be used to align residency curricula with the clinical and surgical practice of recent graduates. Methods: Ontario billing data were used to identify the most common diagnostic and procedure codes used by general otolaryngologists issued a billing number between 2006 and 2012. The codes were categorized by OHNS subspecialty. Practitioners with a narrow range of procedure codes or a high rate of complex procedure codes, were deemed subspecialists and therefore excluded. Results: There were 108 recent graduates in a general practice identified. The most common diagnostic codes assigned to consultation billings were categorized as ‘otology’ (42%), ‘general otolaryngology’ (35%), ‘rhinology’ (17%) and ‘head and neck’ (4%). The most common procedure codes were categorized as ‘general otolaryngology’ (45%), ‘otology’ (23%), ‘head and neck’ (13%) and ‘rhinology’ (9%). The top 5 procedures were nasolaryngoscopy, ear microdebridement, myringotomy with insertion of ventilation tube, tonsillectomy, and turbinate reduction. Although otology encompassed a large proportion of procedures billed, tympanoplasty and mastoidectomy were surprisingly uncommon. Conclusion: This is the first study to analyze the nature of the clinical and surgical cases managed by recent OHNS graduates. -

Tympanostomy Tubes in Children Final Evidence Report: Appendices
Health Technology Assessment Tympanostomy Tubes in Children Final Evidence Report: Appendices October 16, 2015 Health Technology Assessment Program (HTA) Washington State Health Care Authority PO Box 42712 Olympia, WA 98504-2712 (360) 725-5126 www.hca.wa.gov/hta/ [email protected] Tympanostomy Tubes Provided by: Spectrum Research, Inc. Final Report APPENDICES October 16, 2015 WA – Health Technology Assessment October 16, 2015 Table of Contents Appendices Appendix A. Algorithm for Article Selection ................................................................................................. 1 Appendix B. Search Strategies ...................................................................................................................... 2 Appendix C. Excluded Articles ....................................................................................................................... 4 Appendix D. Class of Evidence, Strength of Evidence, and QHES Determination ........................................ 9 Appendix E. Study quality: CoE and QHES evaluation ................................................................................ 13 Appendix F. Study characteristics ............................................................................................................... 20 Appendix G. Results Tables for Key Question 1 (Efficacy and Effectiveness) ............................................. 39 Appendix H. Results Tables for Key Question 2 (Safety) ............................................................................ -

ICD-9/10 Mapping Spreadsheet
ICD-9-CM to ICD-10-CM Mappings for Audiology Related Disorders Updated 7/16/2015 Disclaimer: This product is NOT comprehensive and consists only of codes commonly related to audiology services. Mappings are only to ICD-10-CM codes, not ICD-10-PCS. Every effort was made to accurately map codes using detailed analysis. Keep in mind, however, that while many codes in ICD-9-CM map directly to codes in ICD-10, in some cases, additional clinical analysis may be required to determine which code or codes should be selected for your situation. Always review mapping results before applying them. ICD-9-CM ICD-9-CM Description ICD-10- ICD-10-CM Description Notes Code CM Code 315.32 Mixed receptive-expressive F80.2 Mixed receptive-expressive language language disorder disorder Central auditory processing Developmental dysphasia or aphasia, disorder receptive type Developmental Wernicke's aphasia Excludes1: central auditory processing disorder (H93.25), dysphasia or aphasia NOS (R47.-), expressive language disorder (F80.1), expressive type dysphasia or aphasia (F80.1), word deafness (H93.25) Excludes2: acquired aphasia with epilepsy [Landau-Kleffner] (G40.80-), pervasive developmental disorders (F84.-), selective mutism (F94.0), intellectual disabilities (F70-F79) H93.25 Central auditory processing disorder Congenital auditory imperception Word deafness Excludes1: mixed receptive-epxressive language disorder (F80.2) 380.00 Perichondritis of pinna, unspecified H61.001 Unspecified perichondritis of right external ear H61.002 Unspecified perichondritis -

Vestibular Neuritis and Labyrinthitis
Vestibular Neuritis and DISORDERS Labyrinthitis: Infections of the Inner Ear By Charlotte L. Shupert, PhD with contributions from Bridget Kulick, PT and the Vestibular Disorders Association INFECTIONS Result in damage to inner ear and/or nerve. ARTICLE 079 DID THIS ARTICLE HELP YOU? SUPPORT VEDA @ VESTIBULAR.ORG Vestibular neuritis and labyrinthitis are disorders resulting from an 5018 NE 15th Ave. infection that inflames the inner ear or the nerves connecting the inner Portland, OR 97211 ear to the brain. This inflammation disrupts the transmission of sensory 1-800-837-8428 information from the ear to the brain. Vertigo, dizziness, and difficulties [email protected] with balance, vision, or hearing may result. vestibular.org Infections of the inner ear are usually viral; less commonly, the cause is bacterial. Such inner ear infections are not the same as middle ear infections, which are the type of bacterial infections common in childhood affecting the area around the eardrum. VESTIBULAR.ORG :: 079 / DISORDERS 1 INNER EAR STRUCTURE AND FUNCTION The inner ear consists of a system of fluid-filled DEFINITIONS tubes and sacs called the labyrinth. The labyrinth serves two functions: hearing and balance. Neuritis Inflamation of the nerve. The hearing function involves the cochlea, a snail- shaped tube filled with fluid and sensitive nerve Labyrinthitis Inflamation of the labyrinth. endings that transmit sound signals to the brain. Bacterial infection where The balance function involves the vestibular bacteria infect the middle organs. Fluid and hair cells in the three loop-shaped ear or the bone surrounding semicircular canals and the sac-shaped utricle and Serous the inner ear produce toxins saccule provide the brain with information about Labyrinthitis that invade the inner ear via head movement.