Hearing Loss, Vertigo and Tinnitus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: a Clinical Study
Int Adv Otol 2014; 10(2): 102-6 • DOI: 10.5152/iao.2014.40 Original Article A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: A Clinical Study Can Özbay, Rıza Dündar, Erkan Kulduk, Kemal Fatih Soy, Mehmet Aslan, Hüseyin Katılmış Department of Otorhinolaryngology, Şifa University Faculty of Medicine, İzmir, Turkey (CÖ) Department of Otorhinolaryngology, Mardin State Hospital, Mardin, Turkey (RD, EK, KFS, MA) Department of Otorhinolaryngology, Katip Çelebi University Atatürk Training and Research Hospital, İzmir, Turkey (HK) OBJECTIVE: Myringosclerosis (MS) is a pathological condition characterized by hyaline degeneration and calcification of the collagenous structure of the fibrotic layer of the tympanic membrane, which may develop after trauma, infection, or inflammation as myringotomy, insertion of a ventila- tion tube, or myringoplasty. The aim of our study was to both reveal and evaluate the impact of the factors that might be effective on the post-tym- panoplasty development of myringosclerosis in the graft. MATERIALS and METHODS: In line with this objective, a total of 108 patients (44 males and 64 females) aged between 11 and 66 years (mean age, 29.5 years) who had undergone type 1 tympanoplasty (TP) with an intact canal wall technique and type 2 TP, followed up for an average of 38.8 months, were evaluated. In the presence of myringosclerosis, in consideration of the tympanic membrane (TM) quadrants involved, the influential factors were analyzed in our study, together with the development of myringosclerosis, including preoperative factors, such as the presence of myringosclerosis in the residual and also contralateral tympanic membrane, extent and location of the perforation, and perioperative factors, such as tympanosclerosis in the middle ear and mastoid cavity, cholesteatoma, granulation tissue, and type of the operation performed. -
HEARING LOSS, DEAFNESS Ear32 (1)
HEARING LOSS, DEAFNESS Ear32 (1) Hearing Loss, Deafness Last updated: May 11, 2019 CLASSIFICATION, DIAGNOSIS ................................................................................................................. 1 METHODS OF COMMUNICATION FOR DEAF ............................................................................................ 2 MANAGEMENT ......................................................................................................................................... 2 HEARING AIDS (S. AMPLIFICATION) ....................................................................................................... 2 COCHLEAR IMPLANTS ............................................................................................................................ 2 AUDITORY BRAINSTEM IMPLANTS .......................................................................................................... 4 PREVENTION .......................................................................................................................................... 4 PEDIATRIC HEARING DEFICITS ............................................................................................................... 4 ETIOLOGY .............................................................................................................................................. 4 DIAGNOSIS ............................................................................................................................................. 6 TREATMENT .......................................................................................................................................... -

Pediatric Sensorineural Hearing Loss, Part 2: Syndromic And
Published May 19, 2011 as 10.3174/ajnr.A2499 Pediatric Sensorineural Hearing Loss, Part 2: REVIEW ARTICLE Syndromic and Acquired Causes B.Y. Huang SUMMARY: This article is the second in a 2-part series reviewing neuroimaging in childhood SNHL. C. Zdanski Previously, we discussed the clinical work-up of children with hearing impairment, the classification of inner ear malformations, and congenital nonsyndromic causes of hearing loss. Here, we review and M. Castillo illustrate the most common syndromic hereditary and acquired causes of childhood SNHL, with an emphasis on entities that demonstrate inner ear abnormalities on cross-sectional imaging. Syndromes discussed include BOR syndrome, CHARGE syndrome, Pendred syndrome, Waardenburg syndrome, and X-linked hearing loss with stapes gusher. We conclude the article with a review of acquired causes of childhood SNHL, including infections, trauma, and neoplasms. ABBREVIATIONS: BOR ϭ branchio-oto-renal; CISS ϭ constructive interference in steady state; IAC ϭ internal auditory canal; NF-2 ϭ neurofibromatosis type II; SCC ϭ semicircular canal; SNHL ϭ sensorineural hearing loss; T1WI ϭ T1-weighted image; T2 WI ϭ T2-weighted image he estimated prevalence of SNHL in patients younger than Table 1: Selected hereditary syndromes commonly associated with 1 T18 years of age is 6 per 1000, making it one of the leading SNHL causes of childhood disability and a common reason for oto- Inner Ear Malformations on Inner Ear Malformations laryngology referrals. Cross-sectional imaging is now rou- Imaging Not Common on Imaging tinely performed in these patients because it provides impor- Alagille syndrome Alport syndrome tant information about potential etiologies for hearing loss, Branchio-oto-renal syndrome Biotinidase deficiency defines the anatomy of the temporal bone and the central au- CHARGE syndrome Jervell and Lange-Nielsen syndrome ditory pathway, and identifies additional intracranial abnor- Klippel-Feil syndrome Norrie syndrome malities that may require further work-up. -
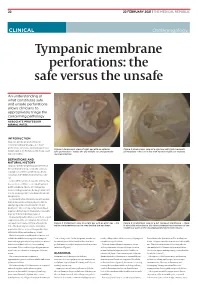
Tympanic Membrane Perforations: the Safe Versus the Unsafe
TMR_210222_22 2021-02-12T14:56:54+11:00 22 22 FEBRUARY 2021 | THE MEDICAL REPUBLIC CLINICAL Otolaryngology Tympanic membrane perforations: the safe versus the unsafe An understanding of what constitutes safe and unsafe perforations allows clinicians to appropriately triage the concerning pathology ASSOCIATE PROFESSOR NIRMAL PATEL INTRODUCTION Tympanic membrane perforations are seen frequently in general practice. Some perforations can be associated with significant Figure 1: Endoscopic view of right ear with an anterior Figure 2: Endoscopic view of a right ear with twin traumatic disease, such as cholesteatoma which may cause safe perforation – notice the dry middle ear and posterior perforations – the ear is dry with normal middle ear mucosa. major morbidity. myringosclerosis DEFINITIONS AND NATURAL HISTORY Tympanic membrane perforations are holes in the ear drum that most commonly occur as a consequence of either ear infections, chronic eustachian tube dysfunction or trauma to the ear. Acute middle ear infection (acute otitis media) is a common condition occurring at least once in 80% of children. Most acute otitis media resolves with spontaneous discharge of infected secretions through the eustachian tube into the nasopharynx. Occasionally when the infections are frequent, there is extensive scarring (tympanosclerosis and myringosclerosis) of the ear drum and middle ear . This scarring compromises blood supply to the healing ear drum and occasionally stops the hole from healing. (Figure 1) Traumatically induced holes occur from a rapid compression of the air column in the external ear canal, most commonly from a blow to the Figure 3: Endoscopic view of a right ear with an attic wax – the Figure 4: Endoscopic view of a left tympanic membrane – there white cholesteatoma can be seen behind the ear drum. -

Hearing Screening Training Manual REVISED 12/2018
Hearing Screening Training Manual REVISED 12/2018 Minnesota Department of Health (MDH) Community and Family Health Division Maternal and Child Health Section 1 2 For more information, contact Minnesota Department of Health Maternal Child Health Section 85 E 7th Place St. Paul, MN 55164-0882 651-201-3760 [email protected] www.health.state.mn.us Upon request, this material will be made available in an alternative format such as large print, Braille or audio recording. 3 Revisions made to this manual are based on: Guidelines for Hearing Screening After the Newborn Period to Kindergarten Age http://www.improveehdi.org/mn/library/files/afternewbornperiodguidelines.pdf American Academy of Audiology, Childhood Screening Guidelines http://www.cdc.gov/ncbddd/hearingloss/documents/AAA_Childhood%20Hearing%2 0Guidelines_2011.pdf American Academy of Pediatrics (AAP), Hearing Assessment in Children: Recommendations Beyond Neonatal Screening http://pediatrics.aappublications.org/content/124/4/1252 4 Contents Introduction .................................................................................................................... 7 Audience ..................................................................................................................... 7 Purpose ....................................................................................................................... 7 Overview of hearing and hearing loss ............................................................................ 9 Sound, hearing, and hearing -

Migraine Associated Vertigo
Headache: The Journal of Head and Face Pain VC 2015 American Headache Society Published by JohnWiley & Sons, Inc. doi: 10.1111/head.12704 Headache Toolbox Migraine Associated Vertigo Between 30 and 50% of migraineurs will sometimes times a condition similar to benign positional vertigo experience dizziness, a sense of spinning, or feeling like called vestibular neuronitis (or vestibular neuritis/labyrinthi- their balance is off in the midst of their headaches. This is tis) is triggered by a viral infection of the inner ear, result- now termed vestibular migraine, but is also called ing in constant vertigo or unsteadiness. Symptoms can migraine associated vertigo. Sometimes migraineurs last for a few days to a few weeks and then go away as experience these symptoms before the headache, but mysteriously as they came on. Vestibular migraine, by they can occur during the headache, or even without any definition, should have migraine symptoms in at least head pain. In children, vertigo may be a precursor to 50% of the vertigo episodes, and these include head migraines developing in the teens or adulthood. Migraine pain, light and noise sensitivity, and nausea. associated vertigo may be more common in those with There are red flags, which are warning signs that ver- motion sickness. tigo is not part of a migraine. Sudden hearing loss can be For some patients this vertiginous sensation resem- the sign of an infection that needs treatment. Loss of bal- bles migraine aura, which is a reversible, relatively short- ance alone, or accompanied by weakness can be the lived neurologic symptom associated with their migraines. -

Ear, Page 1 Lecture Outline
Ear - Hearing perspective Dr. Darren Hoffmann Lecture Objectives: After this lecture, you should be able to: -Describe the surface anatomy of the external ear in anatomical language -Recognize key anatomy in an otoscopic view of the tympanic membrane -Describe the anatomy and function of the ossicles and their associated muscles -Relate the anatomical structures of the middle ear to the anterior, posterior, lateral or medial walls -Explain the anatomy of middle ear infection and which regions have potential to spread to ear -Describe the anatomical structures of the inner ear -Discriminate between endolymph and perilymph in terms of their origin, composition and reabsorption mechanisms -Identify the structures of the Cochlea and Vestibular system histologically -Explain how hair cells function to transform fluid movement into electrical activity -Discriminate the location of cochlear activation for different frequencies of sound -Relate the hair cells of the cochlea to the hair cells of the vestibular system -Contrast the vestibular structures of macula and crista terminalis Let’s look at the following regions: Hoffmann – Ear, Page 1 Lecture Outline: C1. External Ear Function: Amplification of Sound waves Parts Auricle Visible part of external ear (pinna) Helix – large outer rim Tragus – tab anterior to external auditory meatus External auditory meatus Auditory Canal/External Auditory Meatus Leads from Auricle to Tympanic membrane Starts cartilaginous, becomes bony as it enters petrous part of temporal bone Earwax (Cerumen) Complex mixture -

ICD-9/10 Mapping Spreadsheet
ICD-9-CM to ICD-10-CM Mappings for Audiology Related Disorders Updated 7/16/2015 Disclaimer: This product is NOT comprehensive and consists only of codes commonly related to audiology services. Mappings are only to ICD-10-CM codes, not ICD-10-PCS. Every effort was made to accurately map codes using detailed analysis. Keep in mind, however, that while many codes in ICD-9-CM map directly to codes in ICD-10, in some cases, additional clinical analysis may be required to determine which code or codes should be selected for your situation. Always review mapping results before applying them. ICD-9-CM ICD-9-CM Description ICD-10- ICD-10-CM Description Notes Code CM Code 315.32 Mixed receptive-expressive F80.2 Mixed receptive-expressive language language disorder disorder Central auditory processing Developmental dysphasia or aphasia, disorder receptive type Developmental Wernicke's aphasia Excludes1: central auditory processing disorder (H93.25), dysphasia or aphasia NOS (R47.-), expressive language disorder (F80.1), expressive type dysphasia or aphasia (F80.1), word deafness (H93.25) Excludes2: acquired aphasia with epilepsy [Landau-Kleffner] (G40.80-), pervasive developmental disorders (F84.-), selective mutism (F94.0), intellectual disabilities (F70-F79) H93.25 Central auditory processing disorder Congenital auditory imperception Word deafness Excludes1: mixed receptive-epxressive language disorder (F80.2) 380.00 Perichondritis of pinna, unspecified H61.001 Unspecified perichondritis of right external ear H61.002 Unspecified perichondritis -

Vestibular Neuritis and Labyrinthitis
Vestibular Neuritis and DISORDERS Labyrinthitis: Infections of the Inner Ear By Charlotte L. Shupert, PhD with contributions from Bridget Kulick, PT and the Vestibular Disorders Association INFECTIONS Result in damage to inner ear and/or nerve. ARTICLE 079 DID THIS ARTICLE HELP YOU? SUPPORT VEDA @ VESTIBULAR.ORG Vestibular neuritis and labyrinthitis are disorders resulting from an 5018 NE 15th Ave. infection that inflames the inner ear or the nerves connecting the inner Portland, OR 97211 ear to the brain. This inflammation disrupts the transmission of sensory 1-800-837-8428 information from the ear to the brain. Vertigo, dizziness, and difficulties [email protected] with balance, vision, or hearing may result. vestibular.org Infections of the inner ear are usually viral; less commonly, the cause is bacterial. Such inner ear infections are not the same as middle ear infections, which are the type of bacterial infections common in childhood affecting the area around the eardrum. VESTIBULAR.ORG :: 079 / DISORDERS 1 INNER EAR STRUCTURE AND FUNCTION The inner ear consists of a system of fluid-filled DEFINITIONS tubes and sacs called the labyrinth. The labyrinth serves two functions: hearing and balance. Neuritis Inflamation of the nerve. The hearing function involves the cochlea, a snail- shaped tube filled with fluid and sensitive nerve Labyrinthitis Inflamation of the labyrinth. endings that transmit sound signals to the brain. Bacterial infection where The balance function involves the vestibular bacteria infect the middle organs. Fluid and hair cells in the three loop-shaped ear or the bone surrounding semicircular canals and the sac-shaped utricle and Serous the inner ear produce toxins saccule provide the brain with information about Labyrinthitis that invade the inner ear via head movement. -

Vestibular Neuritis, Labyrinthitis, and a Few Comments Regarding Sudden Sensorineural Hearing Loss Marcello Cherchi
Vestibular neuritis, labyrinthitis, and a few comments regarding sudden sensorineural hearing loss Marcello Cherchi §1: What are these diseases, how are they related, and what is their cause? §1.1: What is vestibular neuritis? Vestibular neuritis, also called vestibular neuronitis, was originally described by Margaret Ruth Dix and Charles Skinner Hallpike in 1952 (Dix and Hallpike 1952). It is currently suspected to be an inflammatory-mediated insult (damage) to the balance-related nerve (vestibular nerve) between the ear and the brain that manifests with abrupt-onset, severe dizziness that lasts days to weeks, and occasionally recurs. Although vestibular neuritis is usually regarded as a process affecting the vestibular nerve itself, damage restricted to the vestibule (balance components of the inner ear) would manifest clinically in a similar way, and might be termed “vestibulitis,” although that term is seldom applied (Izraeli, Rachmel et al. 1989). Thus, distinguishing between “vestibular neuritis” (inflammation of the vestibular nerve) and “vestibulitis” (inflammation of the balance-related components of the inner ear) would be difficult. §1.2: What is labyrinthitis? Labyrinthitis is currently suspected to be due to an inflammatory-mediated insult (damage) to both the “hearing component” (the cochlea) and the “balance component” (the semicircular canals and otolith organs) of the inner ear (labyrinth) itself. Labyrinthitis is sometimes also termed “vertigo with sudden hearing loss” (Pogson, Taylor et al. 2016, Kim, Choi et al. 2018) – and we will discuss sudden hearing loss further in a moment. Labyrinthitis usually manifests with severe dizziness (similar to vestibular neuritis) accompanied by ear symptoms on one side (typically hearing loss and tinnitus). -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Bedside Neuro-Otological Examination and Interpretation of Commonly
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.054478 on 24 November 2004. Downloaded from BEDSIDE NEURO-OTOLOGICAL EXAMINATION AND INTERPRETATION iv32 OF COMMONLY USED INVESTIGATIONS RDavies J Neurol Neurosurg Psychiatry 2004;75(Suppl IV):iv32–iv44. doi: 10.1136/jnnp.2004.054478 he assessment of the patient with a neuro-otological problem is not a complex task if approached in a logical manner. It is best addressed by taking a comprehensive history, by a Tphysical examination that is directed towards detecting abnormalities of eye movements and abnormalities of gait, and also towards identifying any associated otological or neurological problems. This examination needs to be mindful of the factors that can compromise the value of the signs elicited, and the range of investigative techniques available. The majority of patients that present with neuro-otological symptoms do not have a space occupying lesion and the over reliance on imaging techniques is likely to miss more common conditions, such as benign paroxysmal positional vertigo (BPPV), or the failure to compensate following an acute unilateral labyrinthine event. The role of the neuro-otologist is to identify the site of the lesion, gather information that may lead to an aetiological diagnosis, and from there, to formulate a management plan. c BACKGROUND Balance is maintained through the integration at the brainstem level of information from the vestibular end organs, and the visual and proprioceptive sensory modalities. This processing takes place in the vestibular nuclei, with modulating influences from higher centres including the cerebellum, the extrapyramidal system, the cerebral cortex, and the contiguous reticular formation (fig 1).