A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: a Clinical Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Changes in the Three-Dimensional Angular Vestibulo-Ocular Reflex Following Intratympanic Gentamicin for Menieres Disease
JARO 03: 430±443 82002) DOI: 10.1007/s101620010053 JARO Journal of the Association for Research in Otolaryngology Changes in the Three-Dimensional Angular Vestibulo-Ocular Re¯ex following Intratympanic Gentamicin for MeÂnieÁre's Disease 1 1±3 4,5 1 JOHN P. CAREY, LLOYD B. MINOR, GRACE C.Y. PENG, CHARLES C. DELLA SANTINA, 6 7 PHILLIP D. CREMER, AND THOMAS HASLWANTER 1 1Department of Otolaryngology±Head and Neck Surgery, Johns Hopkins University, Baltimore, MD 21287, USA 2Department of Biomedical Engineering, Johns Hopkins University, Baltimore, MD 21205, USA 3Department of Neuroscience, Johns Hopkins University, Baltimore, MD 21205, USA 4Department of Neurology, Johns Hopkins University, Baltimore, MD 21287, USA 1 5Department of Biomedical Engineering, Catholic University of America, Washington, DC 20064, USA 6Eye and Ear Research Unit, Institute of Clinical Neurosciences, Royal Prince Alfred Hospital, Sydney, Australia 7Department of Neurology, ZuÈrich University Hospital, ZuÈrich, Switzerland Received: 19 June 2000; Accepted: 21 January 2002; Online publication: 26 March 2002 ABSTRACT these gain values and those for head thrusts that ex- cited the contralateral canals were <2%. In contrast, The 3-dimensional angular vestibulo-ocular re¯exes caloric asymmetries averaged 40% 32%. Intra- 8AVOR) elicited by rapid rotary head thrusts were tympanic gentamicin resulted in decreased gains studied in 17 subjects with unilateral MeÂnieÁre's attributable to each canal on the treated side: disease before and 2±10 weeks after treatment with 0.40 0.12 8HC), 0.35 0.14 8AC), 0.31 0.14 8PC) intratympanic gentamicin and in 13 subjects after 8p < 0.01). However, the gains attributable to con- surgical unilateral vestibular destruction 8SUVD). -

Hearing Loss Due to Myringotomy and Tube Placement and the Role of Preoperative Audiograms
ORIGINAL ARTICLE Hearing Loss Due to Myringotomy and Tube Placement and the Role of Preoperative Audiograms Mark Emery, MD; Peter C. Weber, MD Background: Postoperative complications of myrin- erative and postoperative sensorineural and conductive gotomy and tube placement often include otorrhea, tym- hearing loss. panosclerosis, and tympanic membrane perforation. How- ever, the incidence of sensorineural or conductive hearing Results: No patient developed a postoperative sensori- loss has not been documented. Recent efforts to curb the neural or conductive hearing loss. All patients resolved use of preoperative audiometric testing requires docu- their conductive hearing loss after myringotomy and tube mentation of this incidence. placement. There was a 1.3% incidence of preexisting sen- sorineural hearing loss. Objective: To define the incidence of conductive and sensorineural hearing loss associated with myrin- Conclusions: The incidence of sensorineural or con- gotomy and tube placement. ductive hearing loss after myringotomy and tube place- ment is negligible and the use of preoperative audiomet- Materials and Methods: A retrospective chart re- ric evaluation may be unnecessary in selected patients, view of 550 patients undergoing myringotomy and tube but further studies need to be done to corroborate this placement was performed. A total of 520 patients under- small data set. going 602 procedures (1204 ears), including myrin- gotomy and tube placement, were assessed for preop- Arch Otolaryngol Head Neck Surg. 1998;124:421-424 TITIS MEDIA (OM) is one erative hearing status and whether it has of the most frequent dis- either improved or remained stable after eases of childhood, af- MTT. A recent report by Manning et al11 fecting at least 80% of demonstrated a 1% incidence of preop- children prior to school erative sensorineural hearing loss (SNHL) Oentry.1-4 Because of the high incidence of in children undergoing MTT. -

Myringotomy and Ear Tubes WHAT IS THE
Myringotomy and Ear Tubes Myringotomy and Ear Tubes What to expect after surgery when ear tubes are placed: WHAT IS THE OPERATION? 1. DIET: There may be nausea or vomiting for a few hours after the operation. Start by drinking liquids and advance to a A very small slit is made in the eardrum for the purpose of draining regular diet as tolerated. fluid out from behind the eardrum and allowing air to get in behind the eardrum. After the slit is made a very tiny plastic or silicone rubber 2. PAIN: Generally, there is little pain, but Tylenol or Tempra may tube is inserted in the eardrum to keep the small hole open. be taken if needed every six hours. If pain medication is needed beyond 2 days, contact the doctor. WHAT IS THE PURPOSE OF THE VENTILATION TUBE? 3. EAR DRAINAGE AFTER THE PROCEDURE: A little bloody Fluid in the ear causes hearing loss, promotes infection, and causes discharge for a few days is expected. Occasionally, there will discomfort. The function of the ventilation tube is to allow air to flow be a lot of mucus drainage from one or both of the ears, for between the outer ear and the middle ear, which equalizes air pressure perhaps a week. It is not unusual if there is no drainage. in the ear. It takes over the function of the patient’s own eustachian tube, which is not functioning properly. The tube will also allow 4. EAR DRAINAGE AFTER THE FIRST WEEK OR TWO: Usually there infection, if it recurs, to drain out of the ear. -
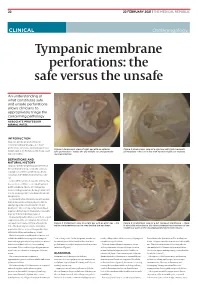
Tympanic Membrane Perforations: the Safe Versus the Unsafe
TMR_210222_22 2021-02-12T14:56:54+11:00 22 22 FEBRUARY 2021 | THE MEDICAL REPUBLIC CLINICAL Otolaryngology Tympanic membrane perforations: the safe versus the unsafe An understanding of what constitutes safe and unsafe perforations allows clinicians to appropriately triage the concerning pathology ASSOCIATE PROFESSOR NIRMAL PATEL INTRODUCTION Tympanic membrane perforations are seen frequently in general practice. Some perforations can be associated with significant Figure 1: Endoscopic view of right ear with an anterior Figure 2: Endoscopic view of a right ear with twin traumatic disease, such as cholesteatoma which may cause safe perforation – notice the dry middle ear and posterior perforations – the ear is dry with normal middle ear mucosa. major morbidity. myringosclerosis DEFINITIONS AND NATURAL HISTORY Tympanic membrane perforations are holes in the ear drum that most commonly occur as a consequence of either ear infections, chronic eustachian tube dysfunction or trauma to the ear. Acute middle ear infection (acute otitis media) is a common condition occurring at least once in 80% of children. Most acute otitis media resolves with spontaneous discharge of infected secretions through the eustachian tube into the nasopharynx. Occasionally when the infections are frequent, there is extensive scarring (tympanosclerosis and myringosclerosis) of the ear drum and middle ear . This scarring compromises blood supply to the healing ear drum and occasionally stops the hole from healing. (Figure 1) Traumatically induced holes occur from a rapid compression of the air column in the external ear canal, most commonly from a blow to the Figure 3: Endoscopic view of a right ear with an attic wax – the Figure 4: Endoscopic view of a left tympanic membrane – there white cholesteatoma can be seen behind the ear drum. -

The Evaluation of Dizzinessin Elderly Patients
Postgrad Med J: first published as 10.1136/pgmj.68.801.558 on 1 July 1992. Downloaded from Postgrad Med J (1992) 68, 558 561 The Fellowship of Postgraduate Medicine, 1992 The evaluation ofdizziness in elderly patients N. Ahmad, J.A. Wilson', R.M. Barr-Hamilton2, D.M. Kean3 and W.J. MacLennan Geriatric Medicine Unit, City Hospital, Edinburgh and Departments of'Otolaryngology, 2Audiology and 3Radiology, Royal Infirmary, Edinburgh, UK Summary: Twenty-one elderly patients with dizziness underwent a comprehensive medical and otoneurological evaluation. The majority had vertigo, limited mobility and restricted neck movements. Poor visual acuity, postural hypotension and presbyacusis were also frequent findings. Electronystagmo- graphy revealed positional nystagmus in 12, disordered smooth pursuit in 18, and abnormal caloric responses in nine. Magnetic resonance imaging showed ischaemic changes in six out of eight patients. Although dizziness in the elderly is clearly multifactorial, the suggested importance of vertebrobasilar ischaemia warrants further consideration as vertigo has been shown to be a risk factor for stroke. Introduction More than one third of individuals over the age of Patients and methods 65 years experience recurrent attacks of dizziness.' Serious consequences include a high incidence of The subjects were 21 patients who had been falls in patients with non-rotating dizziness, and an referred to either the care ofthe elderly unit or ENTcopyright. increased risk of stroke in those with vertigo (a Department in Edinburgh for the investigation of sensation ofmovement relative to surroundings)." 2 dizziness. There were five males and 16 females The causes ofdizziness are legion.3 Its diagnosis, aged 68-95 years (median = 81 years). -

Tympanostomy Tubes in Children Final Evidence Report: Appendices
Health Technology Assessment Tympanostomy Tubes in Children Final Evidence Report: Appendices October 16, 2015 Health Technology Assessment Program (HTA) Washington State Health Care Authority PO Box 42712 Olympia, WA 98504-2712 (360) 725-5126 www.hca.wa.gov/hta/ [email protected] Tympanostomy Tubes Provided by: Spectrum Research, Inc. Final Report APPENDICES October 16, 2015 WA – Health Technology Assessment October 16, 2015 Table of Contents Appendices Appendix A. Algorithm for Article Selection ................................................................................................. 1 Appendix B. Search Strategies ...................................................................................................................... 2 Appendix C. Excluded Articles ....................................................................................................................... 4 Appendix D. Class of Evidence, Strength of Evidence, and QHES Determination ........................................ 9 Appendix E. Study quality: CoE and QHES evaluation ................................................................................ 13 Appendix F. Study characteristics ............................................................................................................... 20 Appendix G. Results Tables for Key Question 1 (Efficacy and Effectiveness) ............................................. 39 Appendix H. Results Tables for Key Question 2 (Safety) ............................................................................ -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Hearing Loss, Vertigo and Tinnitus
HEARING LOSS, VERTIGO AND TINNITUS Jonathan Lara, DO April 29, 2012 Hearing Loss Facts S Men are more likely to experience hearing loss than women. S Approximately 17 percent (36 million) of American adults report some degree of hearing loss. S About 2 to 3 out of every 1,000 children in the United States are born deaf or hard-of-hearing. S Nine out of every 10 children who are born deaf are born to parents who can hear. Hearing Loss Facts S The NIDCD estimates that approximately 15 percent (26 million) of Americans between the ages of 20 and 69 have high frequency hearing loss due to exposure to loud sounds or noise at work or in leisure activities. S Only 1 out of 5 people who could benefit from a hearing aid actually wears one. S Three out of 4 children experience ear infection (otitis media) by the time they are 3 years old. Hearing Loss Facts S There is a strong relationship between age and reported hearing loss: 18 percent of American adults 45-64 years old, 30 percent of adults 65-74 years old, and 47 percent of adults 75 years old or older have a hearing impairment. S Roughly 25 million Americans have experienced tinnitus. S Approximately 4,000 new cases of sudden deafness occur each year in the United States. Hearing Loss Facts S Approximately 615,000 individuals have been diagnosed with Ménière's disease in the United States. Another 45,500 are newly diagnosed each year. S One out of every 100,000 individuals per year develops an acoustic neurinoma (vestibular schwannoma). -
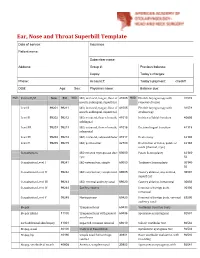
Ear, Nose and Throat Superbill Template Date of Service: Insurance: Patient Name
Ear, Nose and Throat Superbill Template Date of service: Insurance: Patient name: Subscriber name: Address: Group #: Previous balance: Copay: Today’s charges: Phone: Account #: Today’s payment: check# DOB: Age: Sex: Physician name: Balance due: MOD. Patient E/M New Est MOD. I&D, intraoral, tongue, floor of 41005 MOD. Flexible laryngoscopy with 31578 mouth, sublingual, superficial removal of lesion Level I 99201 99211 I&D, intraoral, tongue, floor of 41005 Flexible laryngoscopy with 31579 mouth, sublingual, superficial stroboscopy Level II 99202 99212 I&D, extraoral, floor of mouth, 41015 Incision of labial frenulum 40806 sublingual Level III 99203 99213 I&D, extraoral, floor of mouth, 41016 Excision lingual frenulum 41115 submental Level IV 99204 99214 I&D, extraoral, submandibular 41017 Uvulectomy 42140 Level V 99205 99215 I&D, peritonsillar 42700 Destruction of lesion, palate or 42160 uvula (thermal, cryo) Consultations I&D infected thyroglossal duct 60000 Palate Somnoplasty 42145- cyst 52 Consultation Level I 99241 I&D external ear, simple 69000 Turbinate Somnoplasty 30140- 52 Consultation Level II 99242 I&D external ear, complicated 69005 Cautery ablation, any method, 30801 superficial Consultation Level III 99243 I&D, external auditory canal 69020 Cautery ablation, intramural 30802 Consultation Level IV 99244 Ear Procedures Removal of foreign body, 30300 intranasal Consultation Level V 99245 Myringotomy 69420 Removal of foreign body, external 69200 auditory canal Biopsy Tympanostomy 69433 Vestibular Function Tests Biopsy (Skin) 11100 -

Intratympanic Membrane Cholesteotoma: an Unusual Rare Case
Central Journal of Ear, Nose and Throat Disorders Bringing Excellence in Open Access Case Report *Corresponding author Mohamad Ali El Natout, Department of Otolaryngology Head & Neck Surgery, American University of Beirut Intratympanic Membrane Medical Center, P.O.Box: 11-0236, Riad El-Solh, Beirut 1107 2020, Beirut-Lebanon, USA, Tel: 96-133-449-66; Email: Cholesteotoma: An Unusual Submitted: 11 July 2016 Accepted: 23 July 2016 Rare Case Published: 01 August 2016 Copyright 1 2 1 Hayat Adib , Tamer El Natout , and Mohamad Ali El Natout * © 2016 El Natout et al. 1Department of Otolaryngology Head & Neck Surgery, American University of Beirut Medical Center, USA OPEN ACCESS 2Faculty of Medicine, American University of Beirut, USA Keywords • Intratympanic membrane Abstract • Cholesteatoma • Acquired Intraympanic membrane cholesteotoma without a preceding ear trauma or surgery is a rare entity. Only few cases have been documented in the literature. The exact etiology of this lesion is still unclear. We report an unusual case of an intratympaniccholesteatoma in an adult patient. He is a 45-year-old male who presented with ear fullness and hearing loss six months following an acute otitis media without otorrhea or a tympanic membrane perforation. Physical exam showed a central whitish area on the tympanic membrane. CT scan demonstrated thickening of the tympanic membrane. On the audiogram, he had a 20-dB air-bone gap; tympanogram showed a B-curve. We surgically explored his middle ear and encountered a central tympanic membrane 5X3 mm cholesteatoma with intact middle ear cavity. Accordingly we performed a tympanoplasty. The gold standard for diagnosis of tympanic membrane cholesteotoma is oto-microscopy. -

Neurootological Evaluation of Tinnitus
International Tinnitus Journal 1, 93-97 (1995) Neurootological Evaluation of Tinnitus J. c. R. Seabra, M.D., H. Diamantino, M.D., J. Faria e Almeida, M.D. Ear, Nose and Throat Department, Vila Nova de Gaia, Portugal Abstract: We analyse the neurootological data of patients attended in the Ear, Nose and Throat (E.N.T.) department of the Centro Hospitalar de Vila Nova de Gaia for a tinnitus problem. We submitted these patients to our neurootological routine evaluation. This approach is justified in a tinnitus patient because the cochleovestibular system is a unit and acts as a whole. We characterise the population that came to us by sex and mean age. The profile of these patients is then analysed by our neurootological routine evaluation, which comprises the history taking and audiometric as well as equilibriometric investigations. The results of the audiovestibulometric examinations - pure tone audiometry, vocal audiometry, and Brain Evoked Response Audiometry (B.E.R.A.), Cranio-Corpo Graphy (C.C.G.), Electronystagmography (E.N.G.) - are discussed. We concluded that many tinnitus patients, even those who had no vestibular symptoms, showed some disturbances in the vestibular tests. This fact highlights the need for a complete cochleovestibular investigation in all patients complaining about tinnitus. INTRODUCTION middle ear disease, such as chronic otitis, tympanic perforations, or tympanosclerosis. innitus is a widespread symptom that mortifies We investigated 44 patients, 19 men and 25 women, with T patients and frustrates doctors. It may be the only a mean age of 48-years (standard deviation being 12). symptom complained by patients, but commonly The patients underwent our routine neurootological it is associated with neurosensory hearing loss and/or examination which comprises: vertigo. -

Myringotomy Surgery with PE Tube Placement Perioperative Instructions
Myringotomy Surgery with PE Tube Placement Perioperative Instructions Introduction What is the purpose of myringotomy surgery? This form is intended to inform you about myringotomy (meer-ing- Treats ear infections that have not responded well to other GOT-o-mee) surgery. During myringotomy surgery, a tube is placed treatments in the eardrum. Topics covered include basic function of the ear, what Improves hearing loss caused by fluid build up occurs during surgery and postop care. Improves speech development delayed by hearing loss How does the ear work? Treats recurrent Eustachian tube dysfunction Treats ear problems associated with cleft palate The outer ear collects sound. The paper-thin eardrum separates the outer ear from the middle ear, a tiny air-filled cavity. The middle ear Benefits of myringotomy surgery may include: contains the bones of hearing, which are attached to the eardrum. Fewer and less severe ear infections When sound waves strike the eardrum, it vibrates and sets the bones Hearing improvement in motion, enabling sound to be transmitted to the inner ear. The inner Improvement of speech ear converts vibrations to electrical signals and sends these signals to the brain. What are the risks of surgery? A healthy middle ear contains air, which enters through the narrow Difficulties related to anesthesia Eustachian tube that connects the back of the nose to the ear. A Failure for the incision to heal after the tube falls out normally functioning Eustachian tube opens to equalize pressure in (tympanic membrane perforation) the middle ear, allowing fluid to exist. Fluid build-up in the middle Scarring of the eardrum ear can block transmission of sound, causing hearing loss and/or Hearing loss setting the stage for recurrent ear infections (otitis media).