Factors Potentially Affecting the Hearing of Petroleum Industry Workers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: a Clinical Study
Int Adv Otol 2014; 10(2): 102-6 • DOI: 10.5152/iao.2014.40 Original Article A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: A Clinical Study Can Özbay, Rıza Dündar, Erkan Kulduk, Kemal Fatih Soy, Mehmet Aslan, Hüseyin Katılmış Department of Otorhinolaryngology, Şifa University Faculty of Medicine, İzmir, Turkey (CÖ) Department of Otorhinolaryngology, Mardin State Hospital, Mardin, Turkey (RD, EK, KFS, MA) Department of Otorhinolaryngology, Katip Çelebi University Atatürk Training and Research Hospital, İzmir, Turkey (HK) OBJECTIVE: Myringosclerosis (MS) is a pathological condition characterized by hyaline degeneration and calcification of the collagenous structure of the fibrotic layer of the tympanic membrane, which may develop after trauma, infection, or inflammation as myringotomy, insertion of a ventila- tion tube, or myringoplasty. The aim of our study was to both reveal and evaluate the impact of the factors that might be effective on the post-tym- panoplasty development of myringosclerosis in the graft. MATERIALS and METHODS: In line with this objective, a total of 108 patients (44 males and 64 females) aged between 11 and 66 years (mean age, 29.5 years) who had undergone type 1 tympanoplasty (TP) with an intact canal wall technique and type 2 TP, followed up for an average of 38.8 months, were evaluated. In the presence of myringosclerosis, in consideration of the tympanic membrane (TM) quadrants involved, the influential factors were analyzed in our study, together with the development of myringosclerosis, including preoperative factors, such as the presence of myringosclerosis in the residual and also contralateral tympanic membrane, extent and location of the perforation, and perioperative factors, such as tympanosclerosis in the middle ear and mastoid cavity, cholesteatoma, granulation tissue, and type of the operation performed. -

Common Urgent ENT Problems APRIL 4, 2019 GERARD MACDONALD MD FRCS
3/21/2019 Common Urgent ENT Problems APRIL 4, 2019 GERARD MACDONALD MD FRCS 1 Course Objectives A review of common Urgent ENT problems presenting to office and ER Clinical Pearls to help you manage in a timely fashion Knowing when to refer 2 1 3/21/2019 I do not have any Conflicts of Interest 3 Top Ten List Of Urgent Calls 1.Acute Otitis Externa 2. Sudden Hearing Loss 3.Facial Palsy 4.Salivary Gland Stone /Infection 5.Peritonsillar Abscess 6.Neck Abscess 7.Nosebleeds 8.Hoarseness 9.Foreign Bodies Ear/Nose 10. Acute Vertigo 4 2 3/21/2019 Acute Otitis Externa Commonly associated with swimming ( swimmer’s ear) Common in diabetics and habitual Q-tip Users Usual presenting symptoms are itching, discharge, pain and swelling. More severe symptoms can include severe pain, parotid swelling,trismus and cellulitiis Most common organism is Pseudomonas Aeruginosa May go on to develop secondary otomycosis if frequent use of topical antibiotics. Malignant External Otitis rare but serious 5 Acute Otitis Externa 6 3 3/21/2019 Acute Otitis Externa - Treatment Debridement/Suctioning ? Culture Avoid syringing Ototopicals : Tobradex, Sofracort, Ciprodex Otowick if canal swollen shut Oral Antibiotic ( Cipro ) and single dose Steroid if severe When to refer : Unrelenting pain and swelling, facial nerve weakness,dysphagia , fever 7 Sudden hearing Loss UNEXPLAINED sudden sensorineural hearing loss occurring over 3 days Not AOM, trauma, acoustic trauma , ototoxicity Often confused with ETD , “fluid” Poorer outcome if not recognized -

UPDATE VOLUME 20 • ISSUE 3 the Newsletter of the Council for Accreditation in Occupational Hearing Conservation
Fall 2008 UPDATE VOLUME 20 • ISSUE 3 The Newsletter of the Council for Accreditation in Occupational Hearing Conservation Hearing noise-induced hearing loss and further degradation of communication. If too much hearing protection is provided, Conservation the combined effects of the hearing loss and the attenuation provided by the hearing protector may result in critical sounds for the Hearing- and communication signals becoming inaudible. I’m often asked what type of hearing protector is best for Impaired Worker workers with hearing impairment. Considering that there is no ‘best’ HPD for all workers in any hearing category, it Introduction by Ted Madison should come as no surprise that no single type of device will The prevalence of hearing loss among persons enrolled meet the needs of all those with hearing loss. What seems in occupational hearing conservation programs (HCPs) is to be consistent, however, is that each case is unique, and difficult to determine. Recently, Tak and Calvert (2008) that extra time and effort is required to help these workers estimated that 11.4% of the overall US workforce reports find the right combination of protection, having hearing difficulty of varying communication and auditory awareness. degrees and that approximately ¼ of Consultation with an audiologist or other the hearing difficulty reported can hearing health care professional is also be attributed to employment. These an important step in most cases. estimates are based on analysis of data One valuable resource is the OSHA from the US National Health Interview Safety & Health Information Bulletin Survey (NHIS) that were collected (SHIB) titled “Hearing Conservation from 1997 to 2003. -
Tympanic Membrane Perforations: the Safe Versus the Unsafe
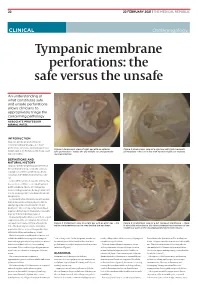
TMR_210222_22 2021-02-12T14:56:54+11:00 22 22 FEBRUARY 2021 | THE MEDICAL REPUBLIC CLINICAL Otolaryngology Tympanic membrane perforations: the safe versus the unsafe An understanding of what constitutes safe and unsafe perforations allows clinicians to appropriately triage the concerning pathology ASSOCIATE PROFESSOR NIRMAL PATEL INTRODUCTION Tympanic membrane perforations are seen frequently in general practice. Some perforations can be associated with significant Figure 1: Endoscopic view of right ear with an anterior Figure 2: Endoscopic view of a right ear with twin traumatic disease, such as cholesteatoma which may cause safe perforation – notice the dry middle ear and posterior perforations – the ear is dry with normal middle ear mucosa. major morbidity. myringosclerosis DEFINITIONS AND NATURAL HISTORY Tympanic membrane perforations are holes in the ear drum that most commonly occur as a consequence of either ear infections, chronic eustachian tube dysfunction or trauma to the ear. Acute middle ear infection (acute otitis media) is a common condition occurring at least once in 80% of children. Most acute otitis media resolves with spontaneous discharge of infected secretions through the eustachian tube into the nasopharynx. Occasionally when the infections are frequent, there is extensive scarring (tympanosclerosis and myringosclerosis) of the ear drum and middle ear . This scarring compromises blood supply to the healing ear drum and occasionally stops the hole from healing. (Figure 1) Traumatically induced holes occur from a rapid compression of the air column in the external ear canal, most commonly from a blow to the Figure 3: Endoscopic view of a right ear with an attic wax – the Figure 4: Endoscopic view of a left tympanic membrane – there white cholesteatoma can be seen behind the ear drum. -
Instruction Sheet: Otitis Externa
University of North Carolina Wilmington Abrons Student Health Center INSTRUCTION SHEET: OTITIS EXTERNA The Student Health Provider has diagnosed otitis externa, also known as external ear infection, or swimmer's ear. Otitis externa is a bacterial/fungal infection in the ear canal (the ear canal goes from the outside opening of the ear to the eardrum). Water in the ear, from swimming or bathing, makes the ear canal prone to infection. Hot and humid weather also predisposes to infection. Symptoms of otitis externa include: ear pain, fullness or itching in the ear, ear drainage, and temporary loss of hearing. These symptoms are similar to those caused by otitis media (middle ear infection). To differentiate between external ear infection and middle ear infection, the provider looks in the ear with an instrument called an otoscope. It is important to distinguish between the two infections, as they are treated differently: External otitis is treated with drops in the ear canal, while middle ear infection is sometimes treated with an antibiotic by mouth. MEASURES YOU SHOULD TAKE TO HELP TREAT EXTERNAL EAR INFECTION: 1. Use the ear drops regularly, as directed on the prescription. 2. The key to treatment is getting the drops down into the canal and keeping the medicine there. To accomplish this: Lie on your side, with the unaffected ear down. Put three to four drops in the infected ear canal, then gently pull the outer ear back and forth several times, working the medicine deeper into the ear canal. Remain still, good-ear-side-down for about 15 minutes. -

The Ear, Nose, and Throat Exam Jeffrey Texiera, MD and Joshua Jabaut, MD CPT, MC, USA LT, MC, USN
The Ear, Nose, and Throat Exam Jeffrey Texiera, MD and Joshua Jabaut, MD CPT, MC, USA LT, MC, USN Midatlantic Regional Occupational and Environmental Medicine Conference Sept. 23, 2017 Disclosures ●We have no funding or financial interest in any product featured in this presentation. The items included are for demonstration purposes only. ●We have no conflicts of interest to disclose. Overview ● Overview of clinically oriented anatomy - presented in the format of the exam ● The approach ● The examination ● Variants of normal anatomy ● ENT emergencies ● Summary/highlights ● Questions Anatomy ● The head and neck exam consists of some of the most comprehensive and complicated anatomy in the human body. ● The ear, nose, and throat comprise a portion of that exam and a focused clinical encounter for an acute ENT complaint may require only this portion of the exam. Ears www.Medscape.com www.taqplayer.info Ear – Vestibular organ www.humanantomylibrary.com Nose/Sinus Anatomy Inferior Middle Turbinate Turbinate Septum Dorsum Sidewalls Ala Floor Tip www.ENT4Students.blogspot.com Columella Vestibule www.beautyepic.com Oral cavity and oropharynx (throat) www.apsubiology.org Neck www.rdhmag.com The Ear, Nose, and Throat exam Perform in a standardized systematic way that works for you Do it the same way every time, this mitigates risk of missing a portion of the exam Practice the exam to increase comfort with performance and familiarize self with variants of normal Describe what you are doing to the patient, describe what you see in your documentation Use your PPE as appropriate A question to keep in mind… ●T/F: The otoscope is the optimal tool for examining the tympanic membrane. -

BMC Ear, Nose and Throat Disorders Biomed Central
BMC Ear, Nose and Throat Disorders BioMed Central Case report Open Access Acute unilateral hearing loss as an unusual presentation of cholesteatoma Daniel Thio*1, Shahzada K Ahmed2 and Richard C Bickerton3 Address: 1Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK, 2Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK and 3Department of Otorhinolaryngology, South Warwickshire General Hospitals NHS Trust Warwick CV34 5BW UK Email: Daniel Thio* - [email protected]; Shahzada K Ahmed - [email protected]; Richard C Bickerton - [email protected] * Corresponding author Published: 18 September 2005 Received: 10 July 2005 Accepted: 18 September 2005 BMC Ear, Nose and Throat Disorders 2005, 5:9 doi:10.1186/1472-6815-5-9 This article is available from: http://www.biomedcentral.com/1472-6815/5/9 © 2005 Thio et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Cholesteatomas are epithelial cysts that contain desquamated keratin. Patients commonly present with progressive hearing loss and a chronically discharging ear. We report an unusual presentation of the disease with an acute hearing loss suffered immediately after prolonged use of a pneumatic drill. Case presentation: A 41 year old man with no previous history of ear problems presented with a sudden loss of hearing in his right ear immediately following the prolonged use of a pneumatic drill on concrete. -

Acoustic Trauma and Hyperbaric Oxygen Treatment
Acoustic Trauma and Hyperbaric Oxygen Treatment Mesut MUTLUOGLU Department of Underwater and Hyperbaric Medicine Gulhane Military Medical Academy Haydarpasa Teaching Hospital 34668, Uskudar, Istanbul TURKEY [email protected] ABSTRACT As stated in the conclusions of the HFM-192 report on hyperbaric oxygen therapy (HBOT) in military medical setting, acoustic trauma is a frequent consequence of military activity in operation. Acoustic trauma refers to an acute hearing loss following a single sudden and very intense noise exposure. It differs from chronic noise induced hearing (NIHL) loss in that it is usually unilateral and causes sudden profound hearing loss. Acoustic trauma is a type of sensorineural hearing loss affecting inner ear structures; particularly the inner and outer hair cells of the organ of Corti within the cochlea. Exposure to noise levels above 85 decibel (dB) may cause hearing loss. While long-term exposure to repetitive or continuous noise above 85 dB may cause chronic NIHL, a single exposure above 130-140 dB, as observed in acoustic trauma, may cause acute NIHL. The loudest sound a human ear may tolerate without pain varies individually, but is usually around 120dB. Military personnel are especially at increased risk for acoustic trauma due to fire arm use in the battle zone. While a machine gun generates around 145dB sound, a rifle generates 157- 163dB, a 105 mm towed howitzer 183dB and an improvised explosive device around 180dB sound. Acoustic trauma displays a gradually down-slopping pattern in the audiogram, particularly after 3000Hz and is therefore described as high-frequency hearing loss. Tinnitus is almost always associated with acoustic trauma. -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Bedside Neuro-Otological Examination and Interpretation of Commonly
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.054478 on 24 November 2004. Downloaded from BEDSIDE NEURO-OTOLOGICAL EXAMINATION AND INTERPRETATION iv32 OF COMMONLY USED INVESTIGATIONS RDavies J Neurol Neurosurg Psychiatry 2004;75(Suppl IV):iv32–iv44. doi: 10.1136/jnnp.2004.054478 he assessment of the patient with a neuro-otological problem is not a complex task if approached in a logical manner. It is best addressed by taking a comprehensive history, by a Tphysical examination that is directed towards detecting abnormalities of eye movements and abnormalities of gait, and also towards identifying any associated otological or neurological problems. This examination needs to be mindful of the factors that can compromise the value of the signs elicited, and the range of investigative techniques available. The majority of patients that present with neuro-otological symptoms do not have a space occupying lesion and the over reliance on imaging techniques is likely to miss more common conditions, such as benign paroxysmal positional vertigo (BPPV), or the failure to compensate following an acute unilateral labyrinthine event. The role of the neuro-otologist is to identify the site of the lesion, gather information that may lead to an aetiological diagnosis, and from there, to formulate a management plan. c BACKGROUND Balance is maintained through the integration at the brainstem level of information from the vestibular end organs, and the visual and proprioceptive sensory modalities. This processing takes place in the vestibular nuclei, with modulating influences from higher centres including the cerebellum, the extrapyramidal system, the cerebral cortex, and the contiguous reticular formation (fig 1). -

Hearing Loss, Vertigo and Tinnitus
HEARING LOSS, VERTIGO AND TINNITUS Jonathan Lara, DO April 29, 2012 Hearing Loss Facts S Men are more likely to experience hearing loss than women. S Approximately 17 percent (36 million) of American adults report some degree of hearing loss. S About 2 to 3 out of every 1,000 children in the United States are born deaf or hard-of-hearing. S Nine out of every 10 children who are born deaf are born to parents who can hear. Hearing Loss Facts S The NIDCD estimates that approximately 15 percent (26 million) of Americans between the ages of 20 and 69 have high frequency hearing loss due to exposure to loud sounds or noise at work or in leisure activities. S Only 1 out of 5 people who could benefit from a hearing aid actually wears one. S Three out of 4 children experience ear infection (otitis media) by the time they are 3 years old. Hearing Loss Facts S There is a strong relationship between age and reported hearing loss: 18 percent of American adults 45-64 years old, 30 percent of adults 65-74 years old, and 47 percent of adults 75 years old or older have a hearing impairment. S Roughly 25 million Americans have experienced tinnitus. S Approximately 4,000 new cases of sudden deafness occur each year in the United States. Hearing Loss Facts S Approximately 615,000 individuals have been diagnosed with Ménière's disease in the United States. Another 45,500 are newly diagnosed each year. S One out of every 100,000 individuals per year develops an acoustic neurinoma (vestibular schwannoma). -

Older Adult Hearing Loss and Screening Key Points • Eighty Percent of Older American Adults Have Untreated Hearing Loss. •
Older Adult Hearing Loss and Screening Key Points Eighty percent of older American adults have untreated hearing loss. Hearing loss is associated with decreased quality of life, depression, communication disorders, social withdrawal and cognitive impairment. Overview Definition Presbycusis is another term for age-related sensorineural hearing loss (ARHL). o Damage to the cochlea, Cranial Nerve VIII, or Internal Auditory canal o Bilateral, symmetric, high-frequency sensorineural hearing loss Noise-induced hearing loss (NIHL) o Direct mechanical injury to sensory hair cells in the cochlea o Continuous noise exposure Aging and hearing loss Cell reduction in auditory cortex Acoustic nerve (CN VIII) fiber degeneration Inner ear sensory cell loss and membrane calcification Risk Factors Advancing Age (ARHI) Exposure to loud noises or ototoxic agents (i.e. loud machinery) (NIHL) Other External ear or middle ear conductive hearing loss risk factors include: o Cerumen impaction o Middle ear fluid o Perforated tympanic membrane Assessment Recommendations for hearing assessments: Screening all older adults over the age of 65 years. Screening should be conducted in a primary care setting. Obtain history of chronic medical conditions (diabetes mellitus, CAD), ear infections, ear trauma, occupation Medication review assessing for use of diuretics (loop), aspirin, antineoplastic (cisplatin, 5- fluorouracil), antimalarial (chloroquine, quinine), and antibiotic (aminoglycosides, erythromycin, tetracycline, vancomycin) Assessment Instruments available include: o Hearing Handicap Inventory for the Elderly Screening (HHIE-S) https://www.audiology.org/sites/default/files/PracticeManagement/Medicare_HHI.pdf . 10 question questionnaire . Score greater than 10 points should be referred to an audiologist o Audio Scope (Welch Allyn, Inc.) . Otoscope examination . Test hearing o Whispered Voice Test, finger rub or a watch tick test o Ask the question - “Do you have a hearing problem now?” If any of the above four are positive – referral to an Audiologist is indicated.