Lingual Tonsil Pseudolymphoma and Obstructive Sleep Apnea
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

Unilateral Tonsillar Swelling: Role and Urgency of Tonsillectomy
Journal of Otolaryngology-ENT Research Case report Open Access Unilateral tonsillar swelling: role and urgency of tonsillectomy Abstract Volume 13 Issue 1 - 2021 Unilateral tonsillar swelling is a fairly common presenting complaint in an Ear, Nose and J Kynaston, S Drever, M Shakeel, M Supriya, N Throat (ENT) department. It may or may not be associated with any other symptoms. Most McCluney of the time, the tonsil asymmetry is secondary to previous history of tonsillitis, quinsy, and Department of otolaryngology and head &neck surgery, tonsil stones. Other benign lesions to cause tonsil swelling may include a mucus retention Aberdeen Royal Infirmary, Aberdeen, UK cyst, lipoma, polyp or papilloma. Sometimes, it is the site of primary malignancy but in these situations, it is often associated with red flag symptoms like pain in the mouth, dysphagia, Correspondence: Muhammad Shakeel, FRCSED (ORL- odynophagia, referred otalgia, weight loss, night sweating, haemoptysis, haematemesis, HNS), Consultant ENT/Thyroid surgeon, Department of hoarseness or neck nodes. Most of the patients with suspected tonsillar malignancy have Otolaryngology-Head and Neck surgery, Aberdeen Royal underlying risk factors like smoking and excessive alcohol intake. However, lately, the Infirmary, Aberdeen, AB252ZN, UK, Tel 00441224552117, tonsil squamous cell carcinoma can be found in younger patients with no history of smoking Email or drinking as there is rising incidence of human papilloma virus related oropharyngeal malignancy. Sometimes, lymphoma may manifest as a tonsil enlargement. If, after detailed Received: June 24, 2020 | Published: February 25, 2021 history and examination, there remains any doubt about the underlying cause of unilateral tonsil swelling then tonsillectomy should be considered for histological analysis. -

The Surgical Plane for Lingual Tonsillectomy: an Anatomic Study Eugene L
Son et al. Journal of Otolaryngology - Head and Neck Surgery (2016) 45:22 DOI 10.1186/s40463-016-0137-3 ORIGINAL RESEARCH ARTICLE Open Access The surgical plane for lingual tonsillectomy: an anatomic study Eugene L. Son1*, Michael P. Underbrink1, Suimin Qiu2 and Vicente A. Resto1 Abstract Background: The presence of a plane between the lingual tonsils and the underlying soft tissue has not been confirmed. The objective of this study is to ascertain the presence and the characteristics about this plane for surgical use. Methods: Five cadaver heads were obtained for dissection of the lingual tonsils. Six permanent sections of previous tongue base biopsies were reviewed. Robot assisted lingual tonsillectomy was performed using the dissection technique from the cadaver dissection. Results: In each of the 5 cadavers, an avascular plane was revealed deep to the lingual tonsils. Microscopic review of the tongue base biopsies revealed a clear demarcation between the lingual tonsils and the underlying minor salivary glands and muscle tissue. This area was relatively avascular. Using the technique described above, a lingual tonsillectomy using TORS was performed with similar findings from the cadaver dissections. Conclusions: A surgical plane for lingual tonsillectomy exists and may prove to have a role with lingual tonsillectomy with TORS. Keywords: Lingual tonsil, Surgical plane, Transoral robotic surgery, Lingual tonsillectomy Background There has been an increase in the incidence of human The base of tongue had once been a difficult area for papilloma virus (HPV) related oropharyngeal squamous surgery to perform on because of problems with expos- cell carcinoma [3]. A large of number of SCCUP with ure. -

Tonsils and Adenoids
Tonsils and Adenoids 575 S 70th Street, Suite 440 Lincoln, NE 68510 402.484.5500 Tonsils and adenoids are masses of tissue similar to the lymph nodes or “glands” found in the neck, groin and armpits. Tonsils are the two masses at the back of the throat. Adenoids are high up in the throat, behind the nose and roof of the mouth (soft palate) and are not visible through the mouth without special instruments. Tonsils and adenoids are near the entrance to the breathing passages, where they catch incoming germs. They “sample” bacteria and viruses, but can become infected themselves. This happens primarily during the first few years of life, but less frequently with age. Children who have their tonsils and adenoids removed suffer no loss in their resistance. What affects tonsils and adenoids? The most common problems affecting the tonsils and adenoids are recurrent infections of the throat or ear and significant enlargement or obstruction that causes breathing and swallowing problems. Abscesses around the tonsils, chronic tonsillitis and infections of small pockets within the tonsils that produce foul-smelling, cheese-like formations can also affect the tonsils and adenoids, making them sore and swollen. Tumors are rare, but can grow on the tonsils. How are tonsil and adenoid diseases treated? Bacterial infections, especially those caused by streptococcus, are first treated with antibiotics. Sometimes, removal of the tonsils and/or adenoids may be recommended. The two primary reasons for removal are recurrent infection despite antibiotic therapy and difficulty breathing due to enlarged tonsils and/or adenoids. Chronic infection can affect other areas, such as the eustachian tube, the passage between the back of the nose and the inside of the ear. -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Oral Cavity Histology Histology > Digestive System > Digestive System
Oral Cavity Histology Histology > Digestive System > Digestive System Oral Cavity LINGUAL PAPILLAE OF THE TONGUE Lingual papillae cover 2/3rds of its anterior surface; lingual tonsils cover its posterior surface. There are three types of lingual papillae: - Filiform, fungiform, and circumvallate; a 4th type, called foliate papillae, are rudimentary in humans. - Surface comprises stratified squamous epithelia - Core comprises lamina propria (connective tissue and vasculature) - Skeletal muscle lies deep to submucosa; skeletal muscle fibers run in multiple directions, allowing the tongue to move freely. - Taste buds lie within furrows or clefts between papillae; each taste bud comprises precursor, immature, and mature taste receptor cells and opens to the furrow via a taste pore. Distinguishing Features: Filiform papillae • Most numerous papillae • Their role is to provide a rough surface that aids in chewing via their keratinized, stratified squamous epithelia, which forms characteristic spikes. • They do not have taste buds. Fungiform papillae • "Fungi" refers to its rounded, mushroom-like surface, which is covered by stratified squamous epithelium. Circumvallate papillae • Are also rounded, but much larger and more bulbous. • On either side of the circumvallate papillae are wide clefts, aka, furrows or trenches; though not visible in our sample, serous Ebner's glands open into these spaces. DENTITION Comprise layers of calcified tissues surrounding a cavity that houses neurovascular structures. Key Features Regions 1 / 3 • The crown, which lies above the gums • The neck, the constricted area • The root, which lies within the alveoli (aka, sockets) of the jaw bones. • Pulp cavity lies in the center of the tooth, and extends into the root as the root canal. -

Extrathymic T Cell Development in the Human Tonsil
EXTRATHYMIC T CELL DEVELOPMENT IN THE HUMAN TONSIL DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Susan Elaine McClory Graduate Program in Integrated Biomedical Science Program The Ohio State University 2012 Dissertation Committee: Professor Michael Caligiuri, MD (Advisor) Professor John Byrd, MD Professor Danilo Perrotti, MD, PhD Professor Amanda Simcox, PhD Copyright by Susan Elaine McClory 2012 Abstract Human T cells are critical mediators of an adaptive immune response, and individuals with T cell deficiencies are prone to devastating infections and disease. It is well known that the thymus, an organ in the anterior mediastinum, is indispensible for the development of a normal T cell repertoire in mammals. Likewise, individuals with poor thymic function due to congenital abnormalities, chemotherapy, or thymectomy suffer from decreased peripheral T cell counts and a subsequent immune deficiency. In murine models, there is evidence that the mucosal lymphoid tissue of the intestine contributes to extrathymic T cell development during normal homeostatic conditions, as can other peripheral lymphoid organs during situations of poor thymic output or pharmacologic intervention. However, whether or not human extrathymic lymphoid tissue, such as the bone marrow, lymph nodes, spleen or tonsil can participate in T cell development has remained unknown and controversial. Indeed, the identification of en extrathymic pathway for T cell lymphopoiesis in humans may suggest alternative pathways for the development of specific T cell subsets or may suggest methods for augmenting T cell generation in the face of thymic injury, absence, or disease. -

Tonsillitis and Enlarged Adenoids and More
Tonsils and Adenoids Insight into tonsillectomy and adenoidectomy What conditions affect the tonsils and adenoids? When should I see a doctor? Common symptoms of tonsillitis and enlarged adenoids and more... Tonsils and adenoids are the body’s first line of defense as part of the immune system. They “sample” bacteria and viruses that enter the body through the mouth or nose, but they sometimes become infected. At times, they become more of a liability than an asset and may even cause airway obstruction or repeated bacterial infections. Your ear, nose, and throat (ENT) specialist can suggest the best treatment options. What are tonsils and adenoids? Tonsils and adenoids are similar to the lymph nodes or “glands” found in the neck, groin, and armpits. Tonsils are the two round lumps in the back of the throat. Adenoids are high in the throat behind the nose and the roof of the mouth (soft palate) and are not visible through the mouth or nose without special instruments. What affects tonsils and adenoids? The two most common problems affecting the tonsils and adenoids are recurrent infections of the nose and throat, and significant enlargement that causes nasal obstruction and/or breathing, swallowing, and sleep problems. Abscesses around the tonsils, chronic tonsillitis, and infections of small pockets within the tonsils that produce foul-smelling white deposits can also affect the tonsils and adenoids, making them sore and swollen. Cancers of the tonsil, while uncommon, require early diagnosis and aggressive treatment. When should I see a doctor? You should see your doctor when you or your child experience the common symptoms of infected or enlarged tonsils or adenoids. -

DHE121 Lesson Objectives
Instructional Objectives for DHE121 Identify the following anatomical structures and terms: Parotid Papilla Canine Eminence Parotid Duct or Stenson’s Duct Primary Teeth Maxilla Permanent Teeth Mandible Anterior Teeth Maxillary Sinuses or Paranasal Sinuses Posterior Teeth Alveolar Process or Bone Incisors Maxillary or Mandibular Vestibule Canines Buccal, Labial, and Alveolar Mucosa Premolars Vestibular Fornix Molars Mucobuccal Fold Exostoses Labial Frenum Pulp Cavity Alveolus Torus or Tori Periodontal Ligament (PDL) Gingiva Crown of a Tooth Attached Gingiva Root of a Tooth Alveolar Mucosa Enamel Mucogingival Junction Dentin Marginal Gingiva Cementum Gingival Sulcu Maxillary or Mandibular Tuberosity Interdental Gingiva or Papilla Fordyce Spots Fauces Linea Alba Anterior and Posterior Tonsillar Pillar Retromolar Pad Palatine Tonsils Palate Hard and Soft Median Palatine Raphe Incisive Papilla Palatine Rugae Uvula of the Palate Pterygomandibular Fold or Raphe Base of the Tongue Body of the Tongue Apex of the Tongue Lingual Papillae Dorsal Surface of the Tongue Median Lingual Sulcus of the Tongue Filiform Lingual Papillae Fungiform Lingual Papillae Sulcus Terminalis of the Tongue Foramen Cecum Circumvallate Lingual Papillae Lingual Tonsil Lateral Surface of the Tongue Foliate Lingual Papillae Ventral Surface of the Tongue Plicae Fimbriata Lingual Frenum Sublingual Fold Sublingual Salivary Gland Sublingual Caruncle Submandibular Duct (Wharton’s Duct) Sublingual Duct (Bartholin’s Duct) Laryngopharynx Nasopharynx Oropharynx Facial or Labial Anterior Buccal Posterior Palatal Frenum Lingual Dorsal Vestibules Oral Mucosa or Mucous Membrane Mastication DHE121 ORAL CAVITY 1. Describe the boundaries of the oral cavity. 2. Cite the two parts of the oral cavity. 3. Define: vestibule oral cavity proper mucobuccal fold frenum alveolar mucosa gingiva exotoses palatine tori (torus palatinis) mandibular tori (torus mandibularis) 4. -

And Oropharynx-Associated Lymphoid Tissue of Sheep T ⁎ Vijay Kumar Saxenaa,B, Alejandra Diaza,C, Jean-Pierre Y
Veterinary Immunology and Immunopathology 208 (2019) 1–5 Contents lists available at ScienceDirect Veterinary Immunology and Immunopathology journal homepage: www.elsevier.com/locate/vetimm Identification and characterization of an M cell marker in nasopharynx- and oropharynx-associated lymphoid tissue of sheep T ⁎ Vijay Kumar Saxenaa,b, Alejandra Diaza,c, Jean-Pierre Y. Scheerlincka, a Centre for Animal Biotechnology, Faculty of Veterinary and Agricultural Sciences, University of Melbourne, Victoria, 3010, Australia b Division of Animal Physiology and Biochemistry, ICAR-Central Sheep and Wool Research Institute, Avikanagar, Tonk, Rajasthan, 304501, India c Laboratorio de Inmunología, Departamento SAMP, Centro de Investigación Veterinaria de Tandil (CIVETAN-CONICET), Facultad de Ciencias Veterinarias, Universidad Nacional del Centro de la Pcia. de Bs. As., Tandil, 7000, Buenos Aires, Argentina ARTICLE INFO ABSTRACT Keywords: M cells play a pivotal role in the induction of immune responses within the mucosa-associated lymphoid tissues. Sheep M cells exist principally in the follicle-associated epithelium (FAE) of the isolated solitary lymphoid follicles as M cells well as in the lymphoid follicles of nasopharynx-associated lymphoid tissue and gut associated lymphoid tissue NALT (GALT). Through lymphatic cannulation it is possible to investigate local immune responses induced following Mucosal immunity nasal Ag delivery in sheep. Hence, identifying sheep M cell markers would allow the targeting of M cells to offset Biomarker the problem of trans-epithelial Ag delivery associated with inducing mucosal immunity. Sheep cDNA from the GP2 tonsils of the oropharynx and nasopharynx was PCR amplified using Glycoprotein-2 (GP2)-specific primers and expressed as a poly-His-tagged recombinant sheep GP2 (56 kDa) in HEK293 cells. -

Adult Tonsillectomy and / Or Sleep Apnea Surgery
2201 Glenwood Ave., Joliet, IL 60435 ENT SURGICAL CONSULTANTS (815) 725-1191, (815) 725-1248 fax (815) 929-2262 Answer Service Thomas K. Kron, MD, FACS 1890 Silver Cross Blvd, Pavilion A, Suite 435, New Lenox, IL 60451 Michael G. Gartlan, MD, FAAP, FACS (815) 717-8768 Rajeev H. Mehta, MD, FACS 900 W. Route 6, Suite 960, Morris, IL 60450 Scott W. DiVenere, MD Sung J. Chung, MD (815) 941-1972 Ankit M. Patel, MD www.entsurgicalillinois.com ADULT TONSILLECTOMY AND/OR SLEEP APNEA SURGERY (1/16) There is a large ring of lymphoid tissue throughout the throat that provides an immune function in the upper respiratory tract during childhood. The largest components of this ring include a pair of palatine tonsils that can be seen through the mouth on each side and the pharyngeal tonsil, commonly referred to as the adenoid, which is located in the upper throat behind the nose. All these tonsil tissues and the lymph nodes in the neck work together to “catch” and trap incoming infections. Unfortunately, the tonsil and adenoid may become the source of infection itself like a plugged filter Ear, Nose & Throat Diseases or they can become so Otolaryngologylarge as to obstruct-Head the airway. & Neck Surgery Facial Plastic & Reconstructive Surgery Usually tonsils and adenoidsThyroid peak inand size P arathyroidby 8 years of Surgery age, then begin to gradually shrink and atrophy by 12 years of age. By this age near complete facial and dental growth has occurred.Pediatric Adolescents Otolaryngology and adults with persistently enlarged tonsils are considered abnormal and usually result from chronic bacteria colonization of the tonsil crypts. -
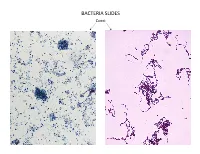
Bacteria Slides
BACTERIA SLIDES Cocci Bacillus BACTERIA SLIDES _______________ __ BACTERIA SLIDES Spirilla BACTERIA SLIDES ___________________ _____ BACTERIA SLIDES Bacillus BACTERIA SLIDES ________________ _ LUNG SLIDE Bronchiole Lumen Alveolar Sac Alveoli Alveolar Duct LUNG SLIDE SAGITTAL SECTION OF HUMAN HEAD MODEL Superior Concha Auditory Tube Middle Concha Opening Inferior Concha Nasal Cavity Internal Nare External Nare Hard Palate Pharyngeal Oral Cavity Tonsils Tongue Nasopharynx Soft Palate Oropharynx Uvula Laryngopharynx Palatine Tonsils Lingual Tonsils Epiglottis False Vocal Cords True Vocal Cords Esophagus Thyroid Cartilage Trachea Cricoid Cartilage SAGITTAL SECTION OF HUMAN HEAD MODEL LARYNX MODEL Side View Anterior View Hyoid Bone Superior Horn Thyroid Cartilage Inferior Horn Thyroid Gland Cricoid Cartilage Trachea Tracheal Rings LARYNX MODEL Posterior View Epiglottis Hyoid Bone Vocal Cords Epiglottis Corniculate Cartilage Arytenoid Cartilage Cricoid Cartilage Thyroid Gland Parathyroid Glands LARYNX MODEL Side View Anterior View ____________ _ ____________ _______ ______________ _____ _____________ ____________________ _____ ______________ _____ _________ _________ ____________ _______ LARYNX MODEL Posterior View HUMAN HEART & LUNGS MODEL Larynx Tracheal Rings Found on the Trachea Left Superior Lobe Left Inferior Lobe Heart Right Superior Lobe Right Middle Lobe Right Inferior Lobe Diaphragm HUMAN HEART & LUNGS MODEL Hilum (curvature where blood vessels enter lungs) Carina Pulmonary Arteries (Blue) Pulmonary Veins (Red) Bronchioles Apex (points