Adult Tonsillectomy and / Or Sleep Apnea Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

Unilateral Tonsillar Swelling: Role and Urgency of Tonsillectomy
Journal of Otolaryngology-ENT Research Case report Open Access Unilateral tonsillar swelling: role and urgency of tonsillectomy Abstract Volume 13 Issue 1 - 2021 Unilateral tonsillar swelling is a fairly common presenting complaint in an Ear, Nose and J Kynaston, S Drever, M Shakeel, M Supriya, N Throat (ENT) department. It may or may not be associated with any other symptoms. Most McCluney of the time, the tonsil asymmetry is secondary to previous history of tonsillitis, quinsy, and Department of otolaryngology and head &neck surgery, tonsil stones. Other benign lesions to cause tonsil swelling may include a mucus retention Aberdeen Royal Infirmary, Aberdeen, UK cyst, lipoma, polyp or papilloma. Sometimes, it is the site of primary malignancy but in these situations, it is often associated with red flag symptoms like pain in the mouth, dysphagia, Correspondence: Muhammad Shakeel, FRCSED (ORL- odynophagia, referred otalgia, weight loss, night sweating, haemoptysis, haematemesis, HNS), Consultant ENT/Thyroid surgeon, Department of hoarseness or neck nodes. Most of the patients with suspected tonsillar malignancy have Otolaryngology-Head and Neck surgery, Aberdeen Royal underlying risk factors like smoking and excessive alcohol intake. However, lately, the Infirmary, Aberdeen, AB252ZN, UK, Tel 00441224552117, tonsil squamous cell carcinoma can be found in younger patients with no history of smoking Email or drinking as there is rising incidence of human papilloma virus related oropharyngeal malignancy. Sometimes, lymphoma may manifest as a tonsil enlargement. If, after detailed Received: June 24, 2020 | Published: February 25, 2021 history and examination, there remains any doubt about the underlying cause of unilateral tonsil swelling then tonsillectomy should be considered for histological analysis. -

Diseases of the Tonsil
DISEASES OF THE TONSIL Dr. Amer salih aljibori Acute Tonsillitis: acute inflammatory condition of the faucial tonsil which may involve the mucosa, crypts,follicles and /or tonsillor parenchyma. Causatve agents; -Viral:Initially starts with viral infection then followed by secondary bacterial infection.Common viruses are influenza,parainfluenza.adenovirus and rhinovirus. -Bacterial:Streptococcus hemolyticus,Hemophilus influenza,pneumococcus,M.catarrahalis. Pathology and pathogenesis: Usually it starts in the childhood when there is low immune status.Depending on the progress of the disease,this can be classified further into the following types. •Catarrhal tonsillitis:It occurs due to viral infection of the upper respiratory tract involving the mucosa of the tonsil •Cryptic tonsillitis: Following viral infection ,secondary bacterial infection supervenes and gets entrapped within the crypts leading to localized form of infection •Acute follicular tonsillitis. It is sever form of tonsillitis caused by virulent organisms like streptococcus hemolyticus and Hemophilus. It causes spread of inflammation from tonsillar crypts to the surrounding tosillar follicles. Acute parenchymal tonsillitis: The secondary bacterial infection will invade to the crypts and it is rapidly spreads into the tonsillar parenchyma.. Cryptic tonsillitis 1- Symptoms -Fever -Generalized malaise and bodyache. -Odynophagia. -Dry cough. -Sorethroat. 2- Signs -Congested and oedematous tonsils -Tonsils may be diffusely swollen in parenchymatous tonsillitis. -Crypts filled with pus in follicular tonsillitis. -Membrane cover the tonsil and termed as membranous tonsillitis. -Tender enlarged jugulodigastric lymph nodes. -Signs of upper respiratory tract infection and adenoiditis. Investigations. -Throat swab for culture and sensitivity. -Blood smear to rule out hemopoeitic disorders like leukemia,agranulocytosis. -Paul-Bunnel test may be required if membrane seen to rulr out infectious mononucleosis. -

The Surgical Plane for Lingual Tonsillectomy: an Anatomic Study Eugene L
Son et al. Journal of Otolaryngology - Head and Neck Surgery (2016) 45:22 DOI 10.1186/s40463-016-0137-3 ORIGINAL RESEARCH ARTICLE Open Access The surgical plane for lingual tonsillectomy: an anatomic study Eugene L. Son1*, Michael P. Underbrink1, Suimin Qiu2 and Vicente A. Resto1 Abstract Background: The presence of a plane between the lingual tonsils and the underlying soft tissue has not been confirmed. The objective of this study is to ascertain the presence and the characteristics about this plane for surgical use. Methods: Five cadaver heads were obtained for dissection of the lingual tonsils. Six permanent sections of previous tongue base biopsies were reviewed. Robot assisted lingual tonsillectomy was performed using the dissection technique from the cadaver dissection. Results: In each of the 5 cadavers, an avascular plane was revealed deep to the lingual tonsils. Microscopic review of the tongue base biopsies revealed a clear demarcation between the lingual tonsils and the underlying minor salivary glands and muscle tissue. This area was relatively avascular. Using the technique described above, a lingual tonsillectomy using TORS was performed with similar findings from the cadaver dissections. Conclusions: A surgical plane for lingual tonsillectomy exists and may prove to have a role with lingual tonsillectomy with TORS. Keywords: Lingual tonsil, Surgical plane, Transoral robotic surgery, Lingual tonsillectomy Background There has been an increase in the incidence of human The base of tongue had once been a difficult area for papilloma virus (HPV) related oropharyngeal squamous surgery to perform on because of problems with expos- cell carcinoma [3]. A large of number of SCCUP with ure. -
Tonsillectomy Instructions After Surgery
VALLEYVALLEY ENTENT Tonsillectomy Instructions After Surgery Tonsils are lymphatic tissue in the back of the throat. They are similar to the adenoids in the back of the nose. The tonsils can get bigger and smaller with infections just like lymph nodes. The tonsils often get smaller as people grow into adults. Why are Tonsils Removed? 1. Recurrent infections 2. Sleep disturbance especially in children and often in addition to removal of the adenoids 3. Tonsil stones that are negatively impacting quality of life 4. Severe asymmetry or suspicion for a mass or growth What is the process for Tonsil removal? The procedure is done in the operating room with anesthesia. Typically after the patient is under anesthesia a specialized retractor is used to move the tongue out of the way and the tonsils are removed using one of multiple techniques including cutting instruments, radio frequency, or electrocautery. What is expected after Tonsillectomy? 1. Tonsillectomy is a painful procedure typically worse in older children and adults. The duration of the discomfort is 1-2 weeks with days 4-7 usually being the most severe. Hydration and consistent use of medication to help with the discomfort are important 2. Children typically receive tylenol/acetominophen with or without a steroid. Older children(>7 years) and adults will often receive narcotic pain medication that is already combined with acetominophen. Discuss with your physician whether or not NSAIDS such as ibuprofen can be used in your particular case. VALLEYVALLEY ENTENT 3. Ear pain is not unexpected after tonsillectomy and rarely represents anything other than referred pain 4. -

Oral Cavity Histology Histology > Digestive System > Digestive System
Oral Cavity Histology Histology > Digestive System > Digestive System Oral Cavity LINGUAL PAPILLAE OF THE TONGUE Lingual papillae cover 2/3rds of its anterior surface; lingual tonsils cover its posterior surface. There are three types of lingual papillae: - Filiform, fungiform, and circumvallate; a 4th type, called foliate papillae, are rudimentary in humans. - Surface comprises stratified squamous epithelia - Core comprises lamina propria (connective tissue and vasculature) - Skeletal muscle lies deep to submucosa; skeletal muscle fibers run in multiple directions, allowing the tongue to move freely. - Taste buds lie within furrows or clefts between papillae; each taste bud comprises precursor, immature, and mature taste receptor cells and opens to the furrow via a taste pore. Distinguishing Features: Filiform papillae • Most numerous papillae • Their role is to provide a rough surface that aids in chewing via their keratinized, stratified squamous epithelia, which forms characteristic spikes. • They do not have taste buds. Fungiform papillae • "Fungi" refers to its rounded, mushroom-like surface, which is covered by stratified squamous epithelium. Circumvallate papillae • Are also rounded, but much larger and more bulbous. • On either side of the circumvallate papillae are wide clefts, aka, furrows or trenches; though not visible in our sample, serous Ebner's glands open into these spaces. DENTITION Comprise layers of calcified tissues surrounding a cavity that houses neurovascular structures. Key Features Regions 1 / 3 • The crown, which lies above the gums • The neck, the constricted area • The root, which lies within the alveoli (aka, sockets) of the jaw bones. • Pulp cavity lies in the center of the tooth, and extends into the root as the root canal. -

Introduction
Charles Kim, Brianne Henderson, Calvin Biddle Introduction • What is conventional imaging? List its pros/cons o Panoramic radiographs, intra-oral radiographs, lateral cephalometrics o Advantages: superior spatial resolution, low cost, easy access (readily available) o Disadvantages: 2D image of a 3D structure – vulnerable to superimpositions o Intraoral radiographs have the best spatial resolution whereas panoramics have moderate resolution, but allow us to see the whole jaw. Panoramics also have distortion in the horizontal plane • What is advanced imaging? List its pros/cons o Advantages: primary diagnosis of maxillary antrum, facial fractures, lesions in base of skull, soft tissue lesions of head and neck. More accurate measurement, and allows more refinement of the differential diagnosis o Disadvantages: poor spatial resolution • Which advanced imaging modalities most likely to contribute to the lesions of the face and jaws? o Cone beam CT, helical CT, magnetic resonance imaging o CBCT is excellent technology in assisting with diagnosis • Why should you image prior to biopsy and other surgery? o Less invasive, interpreted sooner o May not need a biopsy if diagnosis can be made on imaging o Biopsy may disrupt the tissues, nullifying possible diagnoses with imaging techniques in the future ▪ Do not rush into a biopsy until imaging is completed o Example: overzealous biopsies in patients with fibrous dysplasia disrupted the tissues. Many years later, imaging was done due to suspicion of reactivation and many artifacts were found, and -

DHE121 Lesson Objectives
Instructional Objectives for DHE121 Identify the following anatomical structures and terms: Parotid Papilla Canine Eminence Parotid Duct or Stenson’s Duct Primary Teeth Maxilla Permanent Teeth Mandible Anterior Teeth Maxillary Sinuses or Paranasal Sinuses Posterior Teeth Alveolar Process or Bone Incisors Maxillary or Mandibular Vestibule Canines Buccal, Labial, and Alveolar Mucosa Premolars Vestibular Fornix Molars Mucobuccal Fold Exostoses Labial Frenum Pulp Cavity Alveolus Torus or Tori Periodontal Ligament (PDL) Gingiva Crown of a Tooth Attached Gingiva Root of a Tooth Alveolar Mucosa Enamel Mucogingival Junction Dentin Marginal Gingiva Cementum Gingival Sulcu Maxillary or Mandibular Tuberosity Interdental Gingiva or Papilla Fordyce Spots Fauces Linea Alba Anterior and Posterior Tonsillar Pillar Retromolar Pad Palatine Tonsils Palate Hard and Soft Median Palatine Raphe Incisive Papilla Palatine Rugae Uvula of the Palate Pterygomandibular Fold or Raphe Base of the Tongue Body of the Tongue Apex of the Tongue Lingual Papillae Dorsal Surface of the Tongue Median Lingual Sulcus of the Tongue Filiform Lingual Papillae Fungiform Lingual Papillae Sulcus Terminalis of the Tongue Foramen Cecum Circumvallate Lingual Papillae Lingual Tonsil Lateral Surface of the Tongue Foliate Lingual Papillae Ventral Surface of the Tongue Plicae Fimbriata Lingual Frenum Sublingual Fold Sublingual Salivary Gland Sublingual Caruncle Submandibular Duct (Wharton’s Duct) Sublingual Duct (Bartholin’s Duct) Laryngopharynx Nasopharynx Oropharynx Facial or Labial Anterior Buccal Posterior Palatal Frenum Lingual Dorsal Vestibules Oral Mucosa or Mucous Membrane Mastication DHE121 ORAL CAVITY 1. Describe the boundaries of the oral cavity. 2. Cite the two parts of the oral cavity. 3. Define: vestibule oral cavity proper mucobuccal fold frenum alveolar mucosa gingiva exotoses palatine tori (torus palatinis) mandibular tori (torus mandibularis) 4. -

Tonsillitis and Its Yogic Cure
International Journal of Applied Research 2015; 1(6): 338-340 ISSN Print: 2394-7500 ISSN Online: 2394-5869 Impact Factor: 3.4 Tonsillitis and Its yogic cure IJAR 2015; 1(6): 338-340 www.allresearchjournal.com Received: 22-03-2015 Ashok Kumar Sharma, Surinder Singh, Kuldeep Accepted: 25-04-2015 Abstract Dr. Ashok Kumar Sharma The tonsils are part of the lymphatic system, found in oral cavity and pharynx. They are first line of Assistant Professor, defense against pathogens and they produce white blood cells which help the body to fight against CDLU, Sirsa infection. When the tonsils themselves become infected, the condition is called tonsillitis. Yoga is the Surinder Singh best exercise of internal organs and also improves our immune system. Yoga suggests a straight and Research Scholar, simple path to get rid of tonsillitis through some Yogasanas, Kriyas and Pranayamas. Various CDLU, Sirsa Yogasanas, Kriyas and Pranayamas involve a lot of muscular contractions which help in the flow of lymphatic movement throughout the body. The yogic exercises helps in maintaining tone, gives Kuldeep strength and massage to the region. Due to this, the formation of Agranulocytes in the lymph nodes Research Scholar, improves; lymph circulates throughout the lymphatic system; and the plasma cells present in the spleen P.U., Chandigarh produce antibodies, the protective proteins that provide immunity and decrease the chances of infection in tonsils i.e. tonsillitis. Yoga helps us in attaining all round development and has no side effect. If we practice Yoga regularly it eradicates the problem from our body. Whereas antibiotics has side effects on our body and they just suppress the disease instead of eradicating it. -
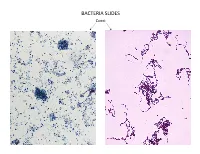
Bacteria Slides
BACTERIA SLIDES Cocci Bacillus BACTERIA SLIDES _______________ __ BACTERIA SLIDES Spirilla BACTERIA SLIDES ___________________ _____ BACTERIA SLIDES Bacillus BACTERIA SLIDES ________________ _ LUNG SLIDE Bronchiole Lumen Alveolar Sac Alveoli Alveolar Duct LUNG SLIDE SAGITTAL SECTION OF HUMAN HEAD MODEL Superior Concha Auditory Tube Middle Concha Opening Inferior Concha Nasal Cavity Internal Nare External Nare Hard Palate Pharyngeal Oral Cavity Tonsils Tongue Nasopharynx Soft Palate Oropharynx Uvula Laryngopharynx Palatine Tonsils Lingual Tonsils Epiglottis False Vocal Cords True Vocal Cords Esophagus Thyroid Cartilage Trachea Cricoid Cartilage SAGITTAL SECTION OF HUMAN HEAD MODEL LARYNX MODEL Side View Anterior View Hyoid Bone Superior Horn Thyroid Cartilage Inferior Horn Thyroid Gland Cricoid Cartilage Trachea Tracheal Rings LARYNX MODEL Posterior View Epiglottis Hyoid Bone Vocal Cords Epiglottis Corniculate Cartilage Arytenoid Cartilage Cricoid Cartilage Thyroid Gland Parathyroid Glands LARYNX MODEL Side View Anterior View ____________ _ ____________ _______ ______________ _____ _____________ ____________________ _____ ______________ _____ _________ _________ ____________ _______ LARYNX MODEL Posterior View HUMAN HEART & LUNGS MODEL Larynx Tracheal Rings Found on the Trachea Left Superior Lobe Left Inferior Lobe Heart Right Superior Lobe Right Middle Lobe Right Inferior Lobe Diaphragm HUMAN HEART & LUNGS MODEL Hilum (curvature where blood vessels enter lungs) Carina Pulmonary Arteries (Blue) Pulmonary Veins (Red) Bronchioles Apex (points -

Eponyms in Head and Neck Anatomy and Radiology
Pictorial Essay Eponyms in Head and Neck Anatomy and Radiology Fernando Martín Ferraro1*, Hernán Chaves2*, Federico Martín Olivera Plata3,4*, Luis Ariel Miquelini1,3*, Suresh K. Mukherji5 1 Imaging Service, Hospital Británico, Ciudad Autónoma de Buenos Aires, Argentina 2 Imaging Department, Dr. Raúl Carrea Institute for Neurological Research (FLENI), Ciudad Autónoma de Buenos Aires, Argentina 3Imaging Service, Hospital Italiano de Buenos Aires, Ciudad Autónoma de Buenos Aires, Argentina 4 Magnetic Resonance and Computed Tomography Service, Centro Médico Deragopyan, Ciudad Autónoma de Buenos Aires, Argentina 5 Radiology Department, Michigan State University, East Lansing, USA Abstract The use of eponyms in medical language is frequent. While it is commonly thought that eponyms are on their way to extinction, this is not entirely true. There is dissent between those who believe that their use should be abandoned and those who advocate that eponyms make unmemorable terms memorable, convey complex concepts and promote an interest in the history of medicine. We feel part of this second group, and our intention is to make a review of eight eponyms linked to head and neck anatomy and radiology. We believe that this approach can be useful for the education of medical students, residents and diagnostic imaging specialists. Keywords Radiology; Eponyms; Anatomy; Head and neck; History of medicine Introduction for which they are known. Eponyms are illustrated by figures of dissections, radiological images and pictures. We believe When we look up the word eponym in Spanish (epónimo) that this approach can be useful for the education of medical in the dictionary of the Spanish Royal Academy, we find the students, residents and diagnostic imaging specialists. -

Tonsil Stones (Tonsilliths) What They Are and How They Form the Mucosal
Tonsil Stones (Tonsilliths) What they are and how they form The mucosal epithelium (the lining tissue of the mouth and throat) naturally sloughs off, but in some people this sloughed epithelium traps into a tonsillar crypt—a space or crevice or hole within the tonsil. These crypts are natural features of the tonsil. This trapped epithelium can further accumulate, building upon itself much like an oyster builds a pearl, and then becomes colonized with bacteria typically found in the mouth. This imparts the foul odor and taste. And voila! A tonsillolith is created. This typically is a benign condition especially if there is no underlying tonsil infection and the tonsil does not look odd or suspicious for something like a tumor. Treatment 1. Daily warm salt water gargles even when not noticing the tonsil stones—this cleanses the tonsils and may prevent stone formation in the first place. 2. You can also use a Water-Pik to cleanse the tonsils daily which would blast the crypts and get them really cleaned. If there has been no significant throat pain or recurrent tonsillitis with these, a tonsillectomy is not needed unless this condition worsens in the future, causing infections or throat pain, difficulty swallowing or if it significantly impacts your quality of life. I try to dissuade patients from surgery such as a tonsillectomy otherwise; mainly with adults, postop pain can be quite severe (often the worse pain you could experience) lasting for at least a week after surgery. Coughing up a tonsil stone on a date .