Blueprint Genetics SCO1 Single Gene Test
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Supl Table 1 for Pdf.Xlsx
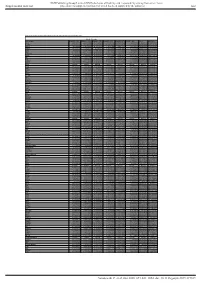
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Gut Table S1. Proteomic analysis of liver tissues from 4-months old control and LPTENKO mice. Soluble Fraction Gene names LOG2FC CTL1 LOG2FC CTL2 LOG2FC CTL3 LOG2FC KO1 LOG2FC KO2 LOG2FC KO3 t-test adj Pvalue Aass 0.081686519 -0.097912098 0.016225579 -1.135271836 -0.860535624 -1.263037541 0.0011157 1.206072068 Acsm5 -0.125220746 0.071090866 0.054129881 -0.780692107 -0.882155692 -1.158378647 0.00189031 1.021713016 Gstm2 -0.12707966 0.572554941 -0.445475281 1.952813994 1.856518122 1.561376671 0.00517664 1.865316016 Gstm1 -0.029147714 0.298593425 -0.26944571 0.983159098 0.872028945 0.786125509 0.00721356 1.949464926 Fasn 0.08403202 -0.214149498 0.130117478 1.052480559 0.779734519 1.229308218 0.00383637 0.829422353 Upb1 -0.112438784 -0.137014769 0.249453553 -1.297732445 -1.181999331 -1.495303666 0.00102373 0.184442034 Selenbp2 0.266508271 0.084791964 -0.351300235 -2.040647809 -2.608780781 -2.039865739 0.00107121 0.165425127 Thrsp -0.15001075 0.177999342 -0.027988592 1.54283307 1.603048661 0.927443822 0.00453549 0.612858263 Hyi 0.142635733 -0.183013091 0.040377359 1.325929636 1.119934412 1.181313897 0.00044587 0.053553518 Eci1 -0.119041811 -0.014846366 0.133888177 -0.599970385 -0.555547972 -1.191875541 0.02292305 2.477981171 Aldh1a7 -0.095682449 -0.017781922 0.113464372 0.653424862 0.931724091 1.110750381 0.00356922 0.350756574 Pebp1 -0.06292058 -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Human Mitochondrial Pathologies of the Respiratory Chain and ATP Synthase: Contributions from Studies of Saccharomyces Cerevisiae
life Review Human Mitochondrial Pathologies of the Respiratory Chain and ATP Synthase: Contributions from Studies of Saccharomyces cerevisiae Leticia V. R. Franco 1,2,* , Luca Bremner 1 and Mario H. Barros 2 1 Department of Biological Sciences, Columbia University, New York, NY 10027, USA; [email protected] 2 Department of Microbiology,Institute of Biomedical Sciences, Universidade de Sao Paulo, Sao Paulo 05508-900, Brazil; [email protected] * Correspondence: [email protected] Received: 27 October 2020; Accepted: 19 November 2020; Published: 23 November 2020 Abstract: The ease with which the unicellular yeast Saccharomyces cerevisiae can be manipulated genetically and biochemically has established this organism as a good model for the study of human mitochondrial diseases. The combined use of biochemical and molecular genetic tools has been instrumental in elucidating the functions of numerous yeast nuclear gene products with human homologs that affect a large number of metabolic and biological processes, including those housed in mitochondria. These include structural and catalytic subunits of enzymes and protein factors that impinge on the biogenesis of the respiratory chain. This article will review what is currently known about the genetics and clinical phenotypes of mitochondrial diseases of the respiratory chain and ATP synthase, with special emphasis on the contribution of information gained from pet mutants with mutations in nuclear genes that impair mitochondrial respiration. Our intent is to provide the yeast mitochondrial specialist with basic knowledge of human mitochondrial pathologies and the human specialist with information on how genes that directly and indirectly affect respiration were identified and characterized in yeast. Keywords: mitochondrial diseases; respiratory chain; yeast; Saccharomyces cerevisiae; pet mutants 1. -

Output Results of CLIME (Clustering by Inferred Models of Evolution)
Output results of CLIME (CLustering by Inferred Models of Evolution) Dataset: Num of genes in input gene set: 81 Total number of genes: 20834 Prediction LLR threshold: 0 The CLIME PDF output two sections: 1) Overview of Evolutionarily Conserved Modules (ECMs) Top panel shows the predefined species tree. Bottom panel shows the partition of input genes into Evolutionary Conserved Modules (ECMs), ordered by ECM strength (shown at right), and separated by horizontal lines. Each row show one gene, where the phylogenetic profile indicates presence (blue) or absence (gray) of homologs in each species (column). Gene symbols are shown at left. Gray color indicates that the gene is a paralog to a higher scoring gene within the same ECM (based on BLASTP E < 1e-3). 2) Details of each ECM and its expansion ECM+ Top panel shows the inferred evolutionary history on the predefined species tree. Branch color shows the gain event (blue) and loss events (red color, with brighter color indicating higher confidence in loss). Branches before the gain or after a loss are shown in gray. Bottom panel shows the input genes that are within the ECM (blue/white rows) as well as all genes in the expanded ECM+ (green/gray rows). The ECM+ includes genes likely to have arisen under the inferred model of evolution relative to a background model, and scored using a log likelihood ratio (LLR). PG indicates "paralog group" and are labeled alphabetically (i.e., A, B). The first gene within each paralog group is shown in black color. All other genes sharing sequence similarity (BLAST E < 1e-3) are assigned to the same PG label and displayed in gray. -

Novel Pathogenic COX20 Variants Causing Dysarthria, Ataxia, and Sensory Neuropathy
UCLA UCLA Previously Published Works Title Novel pathogenic COX20 variants causing dysarthria, ataxia, and sensory neuropathy. Permalink https://escholarship.org/uc/item/3s51m3n7 Journal Annals of clinical and translational neurology, 6(1) ISSN 2328-9503 Authors Otero, Maria G Tiongson, Emmanuelle Diaz, Frank et al. Publication Date 2019 DOI 10.1002/acn3.661 Peer reviewed eScholarship.org Powered by the California Digital Library University of California BRIEF COMMUNICATION Novel pathogenic COX20 variants causing dysarthria, ataxia, and sensory neuropathy Maria G. Otero1,a, Emmanuelle Tiongson2,a, Frank Diaz3, Katrina Haude4, Karin Panzer5, Ashley Collier6, Jaemin Kim1, David Adams7,8, Cynthia J. Tifft7,8, Hong Cui4, Francisca Millian Zamora4, Margaret G. Au9, John M. Graham Jr9, David J. Buckley10, Richard Lewis3, Camilo Toro7,8, Renkui Bai4, Lesley Turner11, Katherine D. Mathews6,12, William Gahl7,8 & Tyler Mark Pierson1,3,9 1Board of Governors Regenerative Medicine Institute, Cedars-Sinai Medical Center, Los Angeles, California 2Division of Neurology, Children’s Hospital of Los Angeles, Los Angeles, California 3Department of Neurology, Cedars-Sinai Medical Center, Los Angeles, California 4GeneDx, Gaithersburg, Maryland 5Department of Pediatrics, University of Iowa Stead Family Children’s Hospital, Iowa City, Iowa 6Provincial Medical Genetics Program, Eastern Health, St. John’s, Newfoundland and Labrador, Canada 7NIH Undiagnosed Diseases Program, NIH Office of Rare Diseases Research and NHGRI, Bethesda, Maryland 8Office of the Clinical Director, NHGRI, NIH, Bethesda, Maryland 9Department of Pediatrics, Cedars-Sinai Medical Center, Los Angeles, California 10Department of Pediatrics, Janeway Health Centre, St. John’s, Newfoundland and Labrador, Canada 11Faculty of Medicine, Memorial University of Newfoundland, St. John’s, Newfoundland, Canada 12Department of Neurology, University of Iowa Stead Family Children’s Hospital, Iowa City, Iowa Correspondence Abstract Tyler M. -

Structural Models and Considerations on the COA6, COX18 and COX20 Factors That Assist Assembly of Human Cytochrome C Oxidase Subunit II
bioRxiv preprint doi: https://doi.org/10.1101/123349; this version posted April 9, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Modeling bulletins Structural models and considerations on the COA6, COX18 and COX20 factors that assist assembly of human cytochrome c oxidase subunit II Luciano A. Abriata Laboratory for Biomolecular Modeling, École Polytechnique Fédérale de Lausanne and Swiss Institute of Bioinformatics, 1015 Lausanne, Switzerland [email protected] Abstract. The soluble domain of cytochrome c oxidase subunit II (COX2), located in the outer side of the inner mitochondrial membrane, contains a binuclear copper site (CuA) through which electrons flow from cytochrome c to the core of the oxidase where oxygen reduction takes place. Being COX2 encoded in the mitochondrial genome, newly synthesized protein undergoes maturation steps in which it is translocated through and inserted into the inner mitochondrial membrane, and copper ions are loaded to form the CuA site. These steps are ensured by several protein factors in a complex pathway that is not fully understood, including copper-loading and disulfide-reduction proteins plus chaperones that assist proper membrane insertion. While the structure and function of copper-loading and disulfide-reducing proteins Sco1 and Sco2 have been quite studied at atomistic level, the latest biological studies have uncovered roles for other proteins that are not yet much understood at the structural level. In particular, recent experiments showed that membrane protein COX18 is a membrane-protein insertase for COX2, whereas membrane protein COX20 is a chaperone that stabilizes COX2 during translocation through the inner mitochondrial membrane, and soluble protein COA6 is part of the copper-loading pathway in conjunction with Sco1 and Sco2. -

Observation of Novel COX20 Mutations Related to Autosomal Recessive Axonal Neuropathy and Static Encephalopathy
Human Genetics (2019) 138:749–756 https://doi.org/10.1007/s00439-019-02026-4 ORIGINAL INVESTIGATION Observation of novel COX20 mutations related to autosomal recessive axonal neuropathy and static encephalopathy Hongliang Xu1 · Tuo Ji1 · Yajun Lian1 · Shuya Wang2 · Xin Chen1 · Shuang Li1 · Yuhui Yin3 · Xiubing Dong4 Received: 21 February 2019 / Accepted: 7 May 2019 / Published online: 11 May 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Cytochrome c oxidase 20 (COX20)/FAM36A encodes a conserved protein that is important for the assembly of COX, com- plex IV of the mitochondrial respiratory chain. A homozygous mutation (p.Thr52Pro) in COX20 gene has been previously described to cause muscle hypotonia and ataxia. In this study, we describe two patients from a non-consanguineous family exhibiting autosomal recessive sensory-dominant axonal neuropathy and static encephalopathy. The whole-exome sequencing analysis revealed that both patients harbored compound heterozygous mutations (p.Lys14Arg and p.Trp74Cys) of COX20 gene. The pathogenicity of the variants was further supported by morphological alternations of mitochondria observed in sural nerve and decreased COX20 protein level of peripheral blood leucocytes derived from the patients. In conclusion, COX20 might be considered as a candidate gene for the complex inherited disease. This observation broadens the clinical and genetic spectrum of COX20-related disease. However, due to the limitation of a single-family study, additional cases and studies are defnitely needed to further confrm the association. Introduction a frequent cause of oxidative phosphorylation disorders in humans. Patients sufering from COX-related mitochondrial Cytochrome c oxidase 20 (COX20, also known as FAM36A) diseases present with heterogeneous clinical phenotypes encodes a conserved protein that is important for the assem- ranging from encephalomyopathy, hypertrophic cardio- bly of COX, complex IV of the mitochondrial respiratory myopathy and liver disease to Leigh’s syndrome (Bourens chain (Bourens et al. -

030626 Mitochondrial Respiratory-Chain Diseases
The new england journal of medicine review article mechanisms of disease Mitochondrial Respiratory-Chain Diseases Salvatore DiMauro, M.D., and Eric A. Schon, Ph.D. From the Departments of Neurology (S.D., ore than a billion years ago, aerobic bacteria colonized E.A.S.) and Genetics and Development primordial eukaryotic cells that lacked the ability to use oxygen metabolical- (E.A.S.), Columbia University College of m Physicians and Surgeons, New York. Ad- ly. A symbiotic relationship developed and became permanent. The bacteria dress reprint requests to Dr. DiMauro at evolved into mitochondria, thus endowing the host cells with aerobic metabolism, a 4-420 College of Physicians and Surgeons, much more efficient way to produce energy than anaerobic glycolysis. Structurally, mito- 630 W. 168th St., New York, NY 10032, or at [email protected]. chondria have four compartments: the outer membrane, the inner membrane, the inter- membrane space, and the matrix (the region inside the inner membrane). They perform N Engl J Med 2003;348:2656-68. numerous tasks, such as pyruvate oxidation, the Krebs cycle, and metabolism of amino Copyright © 2003 Massachusetts Medical Society. acids, fatty acids, and steroids, but the most crucial is probably the generation of energy as adenosine triphosphate (ATP), by means of the electron-transport chain and the ox- idative-phosphorylation system (the “respiratory chain”) (Fig. 1). The respiratory chain, located in the inner mitochondrial membrane, consists of five multimeric protein complexes (Fig. 2B): reduced nicotinamide adenine dinucleotide (NADH) dehydrogenase–ubiquinone oxidoreductase (complex I, approximately 46 sub- units), succinate dehydrogenase–ubiquinone oxidoreductase (complex II, 4 subunits), ubiquinone–cytochrome c oxidoreductase (complex III, 11 subunits), cytochrome c oxi- dase (complex IV, 13 subunits), and ATP synthase (complex V, approximately 16 sub- units). -

Elesclomol Restores Mitochondrial Function in Genetic Models of Copper Deficiency
Elesclomol restores mitochondrial function in genetic models of copper deficiency Shivatheja Somaa, Andrew J. Latimerb, Haarin Chunc, Alison C. Vicarya, Shrishiv A. Timbaliaa, Aren Bouletd, Jennifer J. Rahne, Sherine S. L. Chane, Scot C. Learyd, Byung-Eun Kimc, Jonathan D. Gitlinb, and Vishal M. Gohila,1 aDepartment of Biochemistry and Biophysics, Texas A&M University, College Station, TX 77843; bEugene Bell Center for Regenerative Biology and Tissue Engineering, Marine Biological Laboratory, Woods Hole, MA 02543; cDepartment of Animal and Avian Sciences, University of Maryland, College Park, MD 20742; dDepartment of Biochemistry, University of Saskatchewan, Saskatoon, SK S7N 5E5, Canada; and eDepartment of Drug Discovery and Biomedical Sciences, Medical University of South Carolina, Charleston, SC 29425 Edited by Amy C. Rosenzweig, Northwestern University, Evanston, IL, and approved July 3, 2018 (received for review April 11, 2018) Copper is an essential cofactor of cytochrome c oxidase (CcO), the other proteins, Coa6 and Cox19, have also been shown to be part of terminal enzyme of the mitochondrial respiratory chain. Inherited this copper delivery pathway in the IMS (10–13). loss-of-function mutations in several genes encoding proteins re- In humans, inherited partial loss-of-function mutations in quired for copper delivery to CcO result in diminished CcO activity SCO1, SCO2, and COA6 result in a CcO deficiency and are as- and severe pathologic conditions in affected infants. Copper sup- sociated with hepatopathy, metabolic acidosis, cardiomyopathy, plementation restores CcO function in patient cells with mutations and neurological defects in affected patients (14–16). Copper in two of these genes, COA6 and SCO2, suggesting a potential supplementation rescues CcO deficiency in myoblasts from pa- therapeutic approach. -

Loop Recognition and Copper-Mediated Disulfide Reduction Underpin Metal Site Assembly of Cua in Human Cytochrome Oxidase
Loop recognition and copper-mediated disulfide reduction underpin metal site assembly of CuA in human cytochrome oxidase Marcos N. Morgadaa, Luciano A. Abriataa,1, Chiara Cefarob, Karolina Gajdac,d, Lucia Bancib,c,d,2, and Alejandro J. Vilaa,e,2 aInstituto de Biología Molecular y Celular de Rosario, Consejo Nacional de Investigaciones Científicas y Técnicas, Facultad de Ciencias Bioquímicasy Farmacéuticas, Universidad Nacional de Rosario, 2000 Rosario, Argentina; bFondazione Farmacogenomica FiorGen Onlus, 50019 Sesto Fiorentino, Florence, Italy; cMagnetic Resonance Center, University of Florence, 50019 Sesto Fiorentino, Florence, Italy; dDepartment of Chemistry, University of Florence, 50019 Sesto Fiorentino, Florence, Italy; and ePlataforma Argentina de Biología Estructural y Metabolómica, 2000 Rosario, Argentina Edited by Harry B. Gray, California Institute of Technology, Pasadena, CA, and approved August 12, 2015 (received for review March 12, 2015) Maturation of cytochrome oxidases is a complex process requiring in thioredoxins (24–27). This CX3CXnH motif allows Sco pro- assembly of several subunits and adequate uptake of the metal teins either to bind Cu(I) with high affinity or to act as thiol- cofactors. Two orthologous Sco proteins (Sco1 and Sco2) are essential oxidoreductases (27–29). Both Sco1 and Sco2 are essential for for the correct assembly of the dicopper CuA site in the human CuA biogenesis in humans, but their specific roles are unknown, oxidase, but their function is not fully understood. Here, we report and a detailed mechanism for CuA assembly in mammalian ox- an in vitro biochemical study that shows that Sco1 is a metallocha- idases is still lacking. The fact that metal site assembly requires perone that selectively transfers Cu(I) ions based on loop recogni- the involvement of two orthologous, essential proteins, remains tion, whereas Sco2 is a copper-dependent thiol reductase of the puzzling. -

Functions of Cytochrome C Oxidase Assembly Factors
International Journal of Molecular Sciences Review Functions of Cytochrome c Oxidase Assembly Factors Shane A. Watson and Gavin P. McStay * Department of Biological Sciences, Faculty of School of Life Sciences and Education, Staffordshire University, Science Centre, Leek Road, Stoke-on-Trent ST4 2DF, UK; [email protected]ffs.ac.uk * Correspondence: gavin.mcstay@staffs.ac.uk; Tel.: +44-01782-295741 Received: 17 September 2020; Accepted: 23 September 2020; Published: 30 September 2020 Abstract: Cytochrome c oxidase is the terminal complex of eukaryotic oxidative phosphorylation in mitochondria. This process couples the reduction of electron carriers during metabolism to the reduction of molecular oxygen to water and translocation of protons from the internal mitochondrial matrix to the inter-membrane space. The electrochemical gradient formed is used to generate chemical energy in the form of adenosine triphosphate to power vital cellular processes. Cytochrome c oxidase and most oxidative phosphorylation complexes are the product of the nuclear and mitochondrial genomes. This poses a series of topological and temporal steps that must be completed to ensure efficient assembly of the functional enzyme. Many assembly factors have evolved to perform these steps for insertion of protein into the inner mitochondrial membrane, maturation of the polypeptide, incorporation of co-factors and prosthetic groups and to regulate this process. Much of the information about each of these assembly factors has been gleaned from use of the single cell eukaryote Saccharomyces cerevisiae and also mutations responsible for human disease. This review will focus on the assembly factors of cytochrome c oxidase to highlight some of the outstanding questions in the assembly of this vital enzyme complex. -

Copper Chaperones for Cytochrome C Oxidase and Human Disease
P1: GXB Journal of Bioenergetics and Biomembranes (JOBB) pp677-jobb-455350 November 21, 2002 13:44 Style file version June 22, 2002 Journal of Bioenergetics and Biomembranes, Vol. 34, No. 5, October 2002 (C 2002) Copper Chaperones for Cytochrome c Oxidase and Human Disease Iqbal Hamza1 and Jonathan D. Gitlin1,2 Biological processes in living cells are compartmentalized between lipid membranes. Integral mem- brane proteins often confer specific functions to these compartments and as such have a critical role in cellular metabolism and function. Cytochrome c oxidase is a macromolecular metalloprotein com- plex essential for the respiratory function of the cell. Elucidating the mechanisms of assembly of cytochrome c oxidase within the inner mitochondrial membrane represents a unique challenge for understanding metalloprotein biosynthesis. Elegant genetic experiments in yeast have defined several proteins required for copper delivery to cytochrome c oxidase. While the precise role of each of these proteins in copper incorporation remains unclear, recent studies have revealed that inherited mutations in two of these proteins can result in severe pathology in human infants in association with cytochrome c oxidase deficiency. Characterization of the molecular pathogenesis of these disorders offers new insights into the mechanisms of cellular copper metabolism and the role of these cytochrome c oxidase copper chaperones in human disease. KEY WORDS: copper; metallo chaperone; mitochondria; genetic disease. INTRODUCTION useful cofactor in these metabolic pathways also accounts for the toxicity of this metal in circumstances where cop- Copper is an essential trace element that plays a per homeostasis is impaired (Harris and Gitlin, 1996). For critical role in the biochemistry of aerobic organisms.