Observation of Novel COX20 Mutations Related to Autosomal Recessive Axonal Neuropathy and Static Encephalopathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Supl Table 1 for Pdf.Xlsx
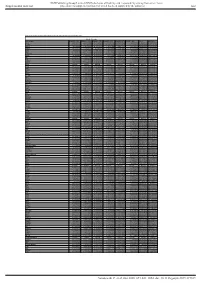
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Gut Table S1. Proteomic analysis of liver tissues from 4-months old control and LPTENKO mice. Soluble Fraction Gene names LOG2FC CTL1 LOG2FC CTL2 LOG2FC CTL3 LOG2FC KO1 LOG2FC KO2 LOG2FC KO3 t-test adj Pvalue Aass 0.081686519 -0.097912098 0.016225579 -1.135271836 -0.860535624 -1.263037541 0.0011157 1.206072068 Acsm5 -0.125220746 0.071090866 0.054129881 -0.780692107 -0.882155692 -1.158378647 0.00189031 1.021713016 Gstm2 -0.12707966 0.572554941 -0.445475281 1.952813994 1.856518122 1.561376671 0.00517664 1.865316016 Gstm1 -0.029147714 0.298593425 -0.26944571 0.983159098 0.872028945 0.786125509 0.00721356 1.949464926 Fasn 0.08403202 -0.214149498 0.130117478 1.052480559 0.779734519 1.229308218 0.00383637 0.829422353 Upb1 -0.112438784 -0.137014769 0.249453553 -1.297732445 -1.181999331 -1.495303666 0.00102373 0.184442034 Selenbp2 0.266508271 0.084791964 -0.351300235 -2.040647809 -2.608780781 -2.039865739 0.00107121 0.165425127 Thrsp -0.15001075 0.177999342 -0.027988592 1.54283307 1.603048661 0.927443822 0.00453549 0.612858263 Hyi 0.142635733 -0.183013091 0.040377359 1.325929636 1.119934412 1.181313897 0.00044587 0.053553518 Eci1 -0.119041811 -0.014846366 0.133888177 -0.599970385 -0.555547972 -1.191875541 0.02292305 2.477981171 Aldh1a7 -0.095682449 -0.017781922 0.113464372 0.653424862 0.931724091 1.110750381 0.00356922 0.350756574 Pebp1 -0.06292058 -

Mutation in the COX4I1 Gene Is Associated with Short Stature, Poor Weight Gain and Increased Chromosomal Breaks, Simulating Fanconi Anemia
European Journal of Human Genetics (2017) 25, 1142–1146 & 2017 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 1018-4813/17 www.nature.com/ejhg ARTICLE Mutation in the COX4I1 gene is associated with short stature, poor weight gain and increased chromosomal breaks, simulating Fanconi anemia Bassam Abu-Libdeh*,1,4, Liza Douiev2,3,4, Sarah Amro1, Maher Shahrour1, Asaf Ta-Shma2, Chaya Miller2,3, Orly Elpeleg2 and Ann Saada*,2,3 We describe a novel autosomal recessive form of mitochondrial disease in a child with short stature, poor weight gain, and mild dysmorphic features with highly suspected Fanconi anemia due to a mutation in COX4I1 gene. Whole Exome Sequencing was performed then followed by Sanger confirmation, identified a K101N mutation in COX4I1, segregating with the disease. This nuclear gene encodes the common isoform of cytochrome c oxidase (COX) subunit 4 (COX 4-1), an integral regulatory part of COX (respiratory chain complex IV) the terminal electron acceptor of the mitochondrial respiratory chain. The patient’s fibroblasts disclosed decreased COX activity, impaired ATP production, elevated ROS production, decreased expression of COX4I1 mRNA and undetectable (COX4) protein. COX activity and ATP production were restored by lentiviral transfection with the wild-type gene. Our results demonstrate the first human mutation in the COX4I1 gene linked to diseases and confirm its role in the pathogenesis. Thus COX4I1 mutations should be considered in any patient with features suggestive of this diagnosis. European Journal of Human Genetics (2017) 25, 1142–1146; doi:10.1038/ejhg.2017.112; published online 2 August 2017 INTRODUCTION normal vaginal delivery with birth weight of 2.8 kg after an uneventful Mitochondrial cytochrome c oxidase (COX, complex IV) is the terminal pregnancy. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Structure of the Intact 14-Subunit Human Cytochrome C Oxidase
www.nature.com/cr www.cell-research.com ARTICLE Structure of the intact 14-subunit human cytochrome c oxidase Shuai Zong 1, Meng Wu1, Jinke Gu1, Tianya Liu1, Runyu Guo1 and Maojun Yang1,2 Respiration is one of the most basic features of living organisms, and the electron transport chain complexes are probably the most complicated protein system in mitochondria. Complex-IV is the terminal enzyme of the electron transport chain, existing either as randomly scattered complexes or as a component of supercomplexes. NDUFA4 was previously assumed as a subunit of complex-I, but recent biochemical data suggested it may be a subunit of complex-IV. However, no structural evidence supporting this notion was available till now. Here we obtained the 3.3 Å resolution structure of complex-IV derived from the human supercomplex I1III2IV1 and assigned the NDUFA4 subunit into complex-IV. Intriguingly, NDUFA4 lies exactly at the dimeric interface observed in previously reported crystal structures of complex-IV homodimer which would preclude complex- IV dimerization. Combining previous structural and biochemical data shown by us and other groups, we propose that the intact complex-IV is a monomer containing 14 subunits. Cell Research (2018) 28:1026–1034; https://doi.org/10.1038/s41422-018-0071-1 INTRODUCTION states under physiological conditions, either being assembled into Mitochondria are critical to many cellular activities. Respiration is supercomplexes or freely scattered on mitochondrial inner the central function of mitochondria, and is exquisitely regulated membrane.36 NDUFA4 was originally considered as a subunit of in multiple ways in response to varying cell conditions.1–3 The Complex-I37 but was proposed to belong to Complex-IV recently.38 assembly of respiratory chain complexes, Complex I–IV (CI, NADH: However, the precise location of NDUFA4 in CIV remains unknown, ubiquinone oxidoreductase; CII, succinate:ubiquinone oxidoreduc- and thus this notion still lacks structural support. -

A High-Resolution Genome-Wide CRISPR/Cas9 Viability Screen
RESEARCH ARTICLE crossm A High-Resolution Genome-Wide CRISPR/Cas9 Viability Screen Reveals Structural Features and Contextual Diversity of the Human Cell-Essential Proteome Downloaded from Thierry Bertomeu,a Jasmin Coulombe-Huntington,a Andrew Chatr-aryamontri,a Karine G. Bourdages,a Etienne Coyaud,b Brian Raught,b Yu Xia,c Mike Tyersa aInstitute for Research in Immunology and Cancer, Department of Medicine, University of Montreal, Montreal, Quebec, Canada bPrincess Margaret Cancer Centre, University Health Network, Toronto, Ontario, Canada cDepartment of Bioengineering, McGill University, Montreal, Quebec, Canada ABSTRACT To interrogate genes essential for cell growth, proliferation and survival http://mcb.asm.org/ in human cells, we carried out a genome-wide clustered regularly interspaced short palindromic repeat (CRISPR)/Cas9 screen in a B-cell lymphoma line using a custom extended-knockout (EKO) library of 278,754 single-guide RNAs (sgRNAs) that tar- geted 19,084 RefSeq genes, 20,852 alternatively spliced exons, and 3,872 hypotheti- cal genes. A new statistical analysis tool called robust analytics and normalization for knockout screens (RANKS) identified 2,280 essential genes, 234 of which were unique. Individual essential genes were validated experimentally and linked to ribo- some biogenesis and stress responses. Essential genes exhibited a bimodal distribu- on December 15, 2018 by guest tion across 10 different cell lines, consistent with a continuous variation in essential- ity as a function of cell type. Genes essential in more lines had more severe fitness defects and encoded the evolutionarily conserved structural cores of protein com- plexes, whereas genes essential in fewer lines formed context-specific modules and encoded subunits at the periphery of essential complexes. -

Mitochondrial Dysfunction and Its Role in Tissue-Specific Cellular Stress
Review www.cell-stress.com Mitochondrial dysfunction and its role in tissue-specific cellular stress David Pacheu-Grau1,*, Robert Rucktäschel1 and Markus Deckers1,* 1 Department of Cellular Biochemistry, University Medical Center Göttingen, Germany. * Corresponding Authors: David Pacheu-Grau, University Medical Center Göttingen, Department of Cellular Biochemistry, Humboldtallee 23, 37073 Göttingen, Germany. Phone: +49-(0)551-394571; E-mail: [email protected]; Markus Deckers, University Medical Center Göttingen, Department of Cellular Biochemistry, Humboldtallee 23, 37073 Göttingen, Germany. Phone: +49-(0)551-395983; E-mail: [email protected] ABSTRACT Mitochondrial bioenergetics require the coordination of two dif- doi: 10.15698/cst2018.07.147 ferent and independent genomes. Mutations in either genome will affect mi- Received originally: 26.04.2018 tochondrial functionality and produce different sources of cellular stress. De- in revised form: 13.06.2018, Accepted 14.06.2018, pending on the kind of defect and stress, different tissues and organs will be Published 13.07.2018. affected, leading to diverse pathological conditions. There is no curative ther- apy for mitochondrial diseases, nevertheless, there are strategies described that fight the various stress forms caused by the malfunctioning organelles. Keywords: mitochondrial dysfunction, Here, we will revise the main kinds of stress generated by mutations in mito- cellular stress, mitochondrial chondrial genes and outline several ways of fighting this stress. pathology, therapy. Abbreviations: ADOA – autosomal dominant optic atrophy, AROA – autosomal recessive optic atrophy, ARS – aminoacyl-tRNA synthetase, CL – cardiolipin, CRISPR – clustered regularly interspaced short palindromic repeats, LHON – Leber’s hereditary optic neuropathy, mt - mitochondrial OXPHOS – oxidative phosphorylation, ROS – reactive oxygen species. -

Impact of Disseminated Neuroblastoma Cells on the Identification of the Relapse-Seeding Clone
Author Manuscript Published OnlineFirst on February 22, 2017; DOI: 10.1158/1078-0432.CCR-16-2082 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Impact of disseminated neuroblastoma cells on the identification of the relapse-seeding clone M. Reza Abbasi1, Fikret Rifatbegovic1, Clemens Brunner1, Georg Mann2, Andrea Ziegler1, Ulrike Pötschger1, Roman Crazzolara3, Marek Ussowicz4, Martin Benesch5, Georg Ebetsberger-Dachs6, Godfrey C.F. Chan7, Neil Jones8, Ruth Ladenstein1,9, Inge M. Ambros1, Peter F. Ambros1,9 1CCRI, Children’s Cancer Research Institute, Vienna, Austria; 2St. Anna Children’s Hospital, Vienna, Austria; 3Department of Pediatrics, Medical University of Innsbruck, Innsbruck, Austria; 4Department of Pediatric Hematology and Oncology, Wroclaw Medical University, Wroclaw, Poland; 5Department of Pediatrics and Adolescent Medicine, Medical University of Graz, Graz, Austria; 6Department of Pediatrics, Kepler University Clinic Linz, Linz, Austria; 7Department of Pediatrics and Adolescent Medicine, University of Hong Kong, Hong Kong; 8Department of Pediatrics and Adolescent Medicine, Paracelsus Medical University, Salzburg, Austria; 9Department of Pediatrics, Medical University of Vienna, Vienna, Austria. Running title: Genomics of disseminated neuroblastoma cells Keywords: Neuroblastoma, disseminated tumor cells, bone marrow, tumor evolution, tumor heterogeneity Financial Support: St. Anna Kinderkrebsforschung; Austrian National Bank (ÖNB), Grant Nos. 15114, 16611; Austrian Science -

Exome Sequencing Reveals SCO2 Mutations in a Family Presented with Fatal Infantile Hyperthermia
Journal of Human Genetics (2013) 58, 226–228 & 2013 The Japan Society of Human Genetics All rights reserved 1434-5161/13 www.nature.com/jhg SHORT COMMUNICATION Exome sequencing reveals SCO2 mutations in a family presented with fatal infantile hyperthermia Nyamkhishig Sambuughin1, Xinyue Liu2, Sunita Bijarnia3, Tarina Wallace1, Ishwar C Verma3, Susan Hamilton4, Sheila Muldoon1, Luke J Tallon2 and Shuishu Wang5 We applied whole-exome sequencing (WES) for identification of an underlying genetic cause of a disease in a family presented with fatal infantile hyperthermia. Analysis of WES results revealed novel, deleterious compound missense mutations, Val160Ala and Pro233Thr, in the synthesis of cytochrome C oxidase 2 gene (SCO2) encoding a mitochondrial protein, Sco2, which is important for cytochrome C oxidase (COX) synthesis. Autosomal recessive mutations in SCO2 are known to be associated with COX deficiency recognized as fatal infantile cardio-encephalomyopathy (604272, OMIM). The Val160Ala and Pro233Thr mutations occurred in the conserved thioredoxin domain of Sco2 and predicted to disrupt protein folding and interaction of Sco2 with other proteins. Our results show applicability of WES in identification of disease-causing mutations and in establishing molecular diagnosis of severe, infantile onset disorder with a challenging diagnosis. Journal of Human Genetics (2013) 58, 226–228; doi:10.1038/jhg.2012.156; published online 31 January 2013 Keywords: exome sequencing; fatal infantile cardio-encephalomyopathy; malignant hyperthermia; recessive mutation; synthesis of cytochrome C oxidase 2 INTRODUCTION persistent hyperthermia in a hot environment. The marriage was non- Whole-exome sequencing (WES) has proven to be an extremely consanguineous, pregnancy was normal and neonatal complications were valuable and cost-effective tool for uncovering disease genes and denied (Supplementary Table S1). -

2014-Platform-Abstracts.Pdf
American Society of Human Genetics 64th Annual Meeting October 18–22, 2014 San Diego, CA PLATFORM ABSTRACTS Abstract Abstract Numbers Numbers Saturday 41 Statistical Methods for Population 5:30pm–6:50pm: Session 2: Plenary Abstracts Based Studies Room 20A #198–#205 Featured Presentation I (4 abstracts) Hall B1 #1–#4 42 Genome Variation and its Impact on Autism and Brain Development Room 20BC #206–#213 Sunday 43 ELSI Issues in Genetics Room 20D #214–#221 1:30pm–3:30pm: Concurrent Platform Session A (12–21): 44 Prenatal, Perinatal, and Reproductive 12 Patterns and Determinants of Genetic Genetics Room 28 #222–#229 Variation: Recombination, Mutation, 45 Advances in Defining the Molecular and Selection Hall B1 Mechanisms of Mendelian Disorders Room 29 #230–#237 #5-#12 13 Genomic Studies of Autism Room 6AB #13–#20 46 Epigenomics of Normal Populations 14 Statistical Methods for Pedigree- and Disease States Room 30 #238–#245 Based Studies Room 6CF #21–#28 15 Prostate Cancer: Expression Tuesday Informing Risk Room 6DE #29–#36 8:00pm–8:25am: 16 Variant Calling: What Makes the 47 Plenary Abstracts Featured Difference? Room 20A #37–#44 Presentation III Hall BI #246 17 New Genes, Incidental Findings and 10:30am–12:30pm:Concurrent Platform Session D (49 – 58): Unexpected Observations Revealed 49 Detailing the Parts List Using by Exome Sequencing Room 20BC #45–#52 Genomic Studies Hall B1 #247–#254 18 Type 2 Diabetes Genetics Room 20D #53–#60 50 Statistical Methods for Multigene, 19 Genomic Methods in Clinical Practice Room 28 #61–#68 Gene Interaction -

Regulation of COX Assembly and Function by Twin CX9C Proteins—Implications for Human Disease
cells Review Regulation of COX Assembly and Function by Twin CX9C Proteins—Implications for Human Disease Stephanie Gladyck 1, Siddhesh Aras 1,2, Maik Hüttemann 1 and Lawrence I. Grossman 1,2,* 1 Center for Molecular Medicine and Genetics, Wayne State University School of Medicine, Detroit, MI 48201, USA; [email protected] (S.G.); [email protected] (S.A.); [email protected] (M.H.) 2 Perinatology Research Branch, Division of Obstetrics and Maternal-Fetal Medicine, Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, U.S. Department of Health and Human Services, Bethesda, Maryland and Detroit, MI 48201, USA * Correspondence: [email protected] Abstract: Oxidative phosphorylation is a tightly regulated process in mammals that takes place in and across the inner mitochondrial membrane and consists of the electron transport chain and ATP synthase. Complex IV, or cytochrome c oxidase (COX), is the terminal enzyme of the electron transport chain, responsible for accepting electrons from cytochrome c, pumping protons to contribute to the gradient utilized by ATP synthase to produce ATP, and reducing oxygen to water. As such, COX is tightly regulated through numerous mechanisms including protein–protein interactions. The twin CX9C family of proteins has recently been shown to be involved in COX regulation by assisting with complex assembly, biogenesis, and activity. The twin CX9C motif allows for the import of these proteins into the intermembrane space of the mitochondria using the redox import machinery of Mia40/CHCHD4. Studies have shown that knockdown of the proteins discussed in this review results in decreased or completely deficient aerobic respiration in experimental models ranging from yeast to human cells, as the proteins are conserved across species. -

Role of Cytochrome C Oxidase Nuclear-Encoded Subunits in Health and Disease
Physiol. Res. 69: 947-965, 2020 https://doi.org/10.33549/physiolres.934446 REVIEW Role of Cytochrome c Oxidase Nuclear-Encoded Subunits in Health and Disease Kristýna ČUNÁTOVÁ1, David PAJUELO REGUERA1, Josef HOUŠTĚK1, Tomáš MRÁČEK1, Petr PECINA1 1Department of Bioenergetics, Institute of Physiology, Czech Academy of Sciences, Prague, Czech Republic Received February 2, 2020 Accepted September 13, 2020 Epub Ahead of Print November 2, 2020 Summary [email protected] and Tomáš Mráček, Department of Cytochrome c oxidase (COX), the terminal enzyme of Bioenergetics, Institute of Physiology CAS, Vídeňská 1083, 142 mitochondrial electron transport chain, couples electron transport 20 Prague 4, Czech Republic. E-mail: [email protected] to oxygen with generation of proton gradient indispensable for the production of vast majority of ATP molecules in mammalian Cytochrome c oxidase cells. The review summarizes current knowledge of COX structure and function of nuclear-encoded COX subunits, which may Energy demands of mammalian cells are mainly modulate enzyme activity according to various conditions. covered by ATP synthesis carried out by oxidative Moreover, some nuclear-encoded subunits possess tissue-specific phosphorylation apparatus (OXPHOS) located in the and development-specific isoforms, possibly enabling fine-tuning central bioenergetic organelle, mitochondria. OXPHOS is of COX function in individual tissues. The importance of nuclear- composed of five multi-subunit complexes embedded in encoded subunits is emphasized by recently discovered the inner mitochondrial membrane (IMM). Electron pathogenic mutations in patients with severe mitopathies. In transport from reduced substrates of complexes I and II to addition, proteins substoichiometrically associated with COX were cytochrome c oxidase (COX, complex IV, CIV) is found to contribute to COX activity regulation and stabilization of achieved by increasing redox potential of individual the respiratory supercomplexes. -

Human Mitochondrial Pathologies of the Respiratory Chain and ATP Synthase: Contributions from Studies of Saccharomyces Cerevisiae
life Review Human Mitochondrial Pathologies of the Respiratory Chain and ATP Synthase: Contributions from Studies of Saccharomyces cerevisiae Leticia V. R. Franco 1,2,* , Luca Bremner 1 and Mario H. Barros 2 1 Department of Biological Sciences, Columbia University, New York, NY 10027, USA; [email protected] 2 Department of Microbiology,Institute of Biomedical Sciences, Universidade de Sao Paulo, Sao Paulo 05508-900, Brazil; [email protected] * Correspondence: [email protected] Received: 27 October 2020; Accepted: 19 November 2020; Published: 23 November 2020 Abstract: The ease with which the unicellular yeast Saccharomyces cerevisiae can be manipulated genetically and biochemically has established this organism as a good model for the study of human mitochondrial diseases. The combined use of biochemical and molecular genetic tools has been instrumental in elucidating the functions of numerous yeast nuclear gene products with human homologs that affect a large number of metabolic and biological processes, including those housed in mitochondria. These include structural and catalytic subunits of enzymes and protein factors that impinge on the biogenesis of the respiratory chain. This article will review what is currently known about the genetics and clinical phenotypes of mitochondrial diseases of the respiratory chain and ATP synthase, with special emphasis on the contribution of information gained from pet mutants with mutations in nuclear genes that impair mitochondrial respiration. Our intent is to provide the yeast mitochondrial specialist with basic knowledge of human mitochondrial pathologies and the human specialist with information on how genes that directly and indirectly affect respiration were identified and characterized in yeast. Keywords: mitochondrial diseases; respiratory chain; yeast; Saccharomyces cerevisiae; pet mutants 1.