Mutation Screening in Patients with Isolated Cytochrome C Oxidase Deficiency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

COX10 (NM 001303) Human Untagged Clone Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for SC119292 COX10 (NM_001303) Human Untagged Clone Product data: Product Type: Expression Plasmids Product Name: COX10 (NM_001303) Human Untagged Clone Tag: Tag Free Symbol: COX10 Synonyms: MC4DN3 Vector: pCMV6-XL5 E. coli Selection: Ampicillin (100 ug/mL) Cell Selection: None Fully Sequenced ORF: >NCBI ORF sequence for NM_001303, the custom clone sequence may differ by one or more nucleotides ATGGCCGCATCTCCGCACACTCTCTCCTCACGCCTCCTGACAGGTTGCGTAGGAGGCTCTGTCTGGTATC TTGAAAGAAGAACTATACAGGACTCCCCTCACAAGTTCTTACATCTTCTCAGGAATGTCAATAAGCAGTG GATTACATTTCAGCACTTTAGCTTCCTCAAACGCATGTATGTCACACAGCTGAACAGAAGCCACAACCAG CAAGTAAGACCCAAGCCAGAACCAGTAGCATCTCCTTTCCTTGAAAAAACATCTTCAGGTCAAGCCAAAG CAGAAATATATGAGATGAGACCTCTCTCACCGCCCAGCCTATCTTTGTCCAGAAAGCCAAATGAAAAGGA ATTGATAGAACTAGAGCCAGACTCAGTAATTGAAGACTCAATAGATGTAGGGAAAGAGACAAAAGAGGAA AAGCGGTGGAAAGAGATGAAGCTGCAAGTGTATGATTTGCCAGGAATTTTGGCTCGACTATCCAAAATCA AACTCACAGCTCTGGTTGTAAGTACCACTGCAGCTGGATTTGCATTGGCTCCGGGCCCTTTTGACTGGCC CTGTTTCCTGCTTACTTCTGTTGGGACAGGCCTTGCATCCTGTGCTGCCAACTCCATCAATCAGTTTTTT GAGGTGCCATTTGACTCAAACATGAATAGGACAAAGAACAGACCGCTGGTTCGTGGACAGATCAGCCCAT TGCTAGCTGTGTCCTTTGCCACTTGTTGTGCTGTTCCGGGAGTTGCCATTCTGACCTTGGGGGTGAATCC ACTCACAGGAGCCCTGGGGCTCTTCAACATTTTCCTGTATACCTGCTGCTACACACCACTGAAAAGGATC AGCATTGCCAACACATGGGTCGGAGCTGTGGTTGGGGCCATCCCGCCTGTCATGGGCTGGACAGCGGCCA CGGGCAGCCTCGATGCTGGCGCATTTCTCCTGGGAGGAATCCTCTACTCCTGGCAGTTTCCTCATTTCAA -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

COX17 (NM 005694) Human Tagged ORF Clone Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for RC210756 COX17 (NM_005694) Human Tagged ORF Clone Product data: Product Type: Expression Plasmids Product Name: COX17 (NM_005694) Human Tagged ORF Clone Tag: Myc-DDK Symbol: COX17 Vector: pCMV6-Entry (PS100001) E. coli Selection: Kanamycin (25 ug/mL) Cell Selection: Neomycin ORF Nucleotide >RC210756 representing NM_005694 Sequence: Red=Cloning site Blue=ORF Green=Tags(s) TTTTGTAATACGACTCACTATAGGGCGGCCGGGAATTCGTCGACTGGATCCGGTACCGAGGAGATCTGCC GCCGCGATCGCC ATGCCGGGTCTGGTTGACTCAAACCCTGCCCCGCCTGAGTCTCAGGAGAAGAAGCCGCTGAAGCCCTGCT GCGCTTGCCCGGAGACCAAGAAGGCGCGCGATGCGTGTATCATCGAGAAAGGAGAAGAACACTGTGGACA TCTAATTGAGGCCCACAAGGAATGCATGAGAGCCCTAGGATTTAAAATA ACGCGTACGCGGCCGCTCGAGCAGAAACTCATCTCAGAAGAGGATCTGGCAGCAAATGATATCCTGGATT ACAAGGATGACGACGATAAGGTTTAA Protein Sequence: >RC210756 representing NM_005694 Red=Cloning site Green=Tags(s) MPGLVDSNPAPPESQEKKPLKPCCACPETKKARDACIIEKGEEHCGHLIEAHKECMRALGFKI TRTRPLEQKLISEEDLAANDILDYKDDDDKV Chromatograms: https://cdn.origene.com/chromatograms/mk8114_f02.zip Restriction Sites: SgfI-MluI This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 4 COX17 (NM_005694) Human Tagged ORF Clone – RC210756 Cloning Scheme: Plasmid Map: ACCN: NM_005694 ORF Size: 189 bp This product is -

Ncomms8214.Pdf
ARTICLE Received 20 Feb 2015 | Accepted 17 Apr 2015 | Published 26 May 2015 DOI: 10.1038/ncomms8214 OPEN Comprehensive survey of condition-specific reproductive isolation reveals genetic incompatibility in yeast Jing Hou1, Anne Friedrich1, Jean-Sebastien Gounot1 & Joseph Schacherer1 Genetic variation within a species could cause negative epistasis leading to reduced hybrid fitness and post-zygotic reproductive isolation. Recent studies in yeasts revealed chromo- somal rearrangements as a major mechanism dampening intraspecific hybrid fertility on rich media. Here, by analysing a large number of Saccharomyces cerevisiae crosses on different culture conditions, we show environment-specific genetic incompatibility segregates readily within yeast and contributes to reproductive isolation. Over 24% (117 out of 481) of cases tested show potential epistasis, among which 6.7% (32 out of 481) are severe, with at least 20% of progeny loss on tested conditions. Based on the segregation patterns, we further characterize a two-locus Dobzhansky–Mu¨ller incompatibility case leading to offspring respiratory deficiency caused by nonsense mutation in a nuclear-encoding mitochondrial gene and tRNA suppressor. We provide evidence that this precise configuration could be adaptive in fluctuating environments, highlighting the role of ecological selection in the onset of genetic incompatibility and reproductive isolation in yeast. 1 Department of Genetics, Genomics and Microbiology, University of Strasbourg/CNRS, UMR7156, 28 rue Goethe, 67083 Strasbourg, France. Correspondence -

Alterations of Genetic Variants and Transcriptomic Features of Response to Tamoxifen in the Breast Cancer Cell Line
Alterations of Genetic Variants and Transcriptomic Features of Response to Tamoxifen in the Breast Cancer Cell Line Mahnaz Nezamivand-Chegini Shiraz University Hamed Kharrati-Koopaee Shiraz University https://orcid.org/0000-0003-2345-6919 seyed taghi Heydari ( [email protected] ) Shiraz University of Medical Sciences https://orcid.org/0000-0001-7711-1137 Hasan Giahi Shiraz University Ali Dehshahri Shiraz University of Medical Sciences Mehdi Dianatpour Shiraz University of Medical Sciences Kamran Bagheri Lankarani Shiraz University of Medical Sciences Research Keywords: Tamoxifen, breast cancer, genetic variants, RNA-seq. Posted Date: August 17th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-783422/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/33 Abstract Background Breast cancer is one of the most important causes of mortality in the world, and Tamoxifen therapy is known as a medication strategy for estrogen receptor-positive breast cancer. In current study, two hypotheses of Tamoxifen consumption in breast cancer cell line (MCF7) were investigated. First, the effect of Tamoxifen on genes expression prole at transcriptome level was evaluated between the control and treated samples. Second, due to the fact that Tamoxifen is known as a mutagenic factor, there may be an association between the alterations of genetic variants and Tamoxifen treatment, which can impact on the drug response. Methods In current study, the whole-transcriptome (RNA-seq) dataset of four investigations (19 samples) were derived from European Bioinformatics Institute (EBI). At transcriptome level, the effect of Tamoxifen was investigated on gene expression prole between control and treatment samples. -
Supl Table 1 for Pdf.Xlsx
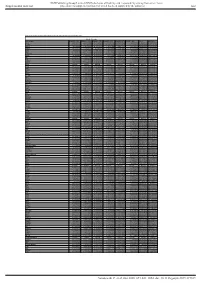
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Gut Table S1. Proteomic analysis of liver tissues from 4-months old control and LPTENKO mice. Soluble Fraction Gene names LOG2FC CTL1 LOG2FC CTL2 LOG2FC CTL3 LOG2FC KO1 LOG2FC KO2 LOG2FC KO3 t-test adj Pvalue Aass 0.081686519 -0.097912098 0.016225579 -1.135271836 -0.860535624 -1.263037541 0.0011157 1.206072068 Acsm5 -0.125220746 0.071090866 0.054129881 -0.780692107 -0.882155692 -1.158378647 0.00189031 1.021713016 Gstm2 -0.12707966 0.572554941 -0.445475281 1.952813994 1.856518122 1.561376671 0.00517664 1.865316016 Gstm1 -0.029147714 0.298593425 -0.26944571 0.983159098 0.872028945 0.786125509 0.00721356 1.949464926 Fasn 0.08403202 -0.214149498 0.130117478 1.052480559 0.779734519 1.229308218 0.00383637 0.829422353 Upb1 -0.112438784 -0.137014769 0.249453553 -1.297732445 -1.181999331 -1.495303666 0.00102373 0.184442034 Selenbp2 0.266508271 0.084791964 -0.351300235 -2.040647809 -2.608780781 -2.039865739 0.00107121 0.165425127 Thrsp -0.15001075 0.177999342 -0.027988592 1.54283307 1.603048661 0.927443822 0.00453549 0.612858263 Hyi 0.142635733 -0.183013091 0.040377359 1.325929636 1.119934412 1.181313897 0.00044587 0.053553518 Eci1 -0.119041811 -0.014846366 0.133888177 -0.599970385 -0.555547972 -1.191875541 0.02292305 2.477981171 Aldh1a7 -0.095682449 -0.017781922 0.113464372 0.653424862 0.931724091 1.110750381 0.00356922 0.350756574 Pebp1 -0.06292058 -

Supplementary Table S1. Correlation Between the Mutant P53-Interacting Partners and PTTG3P, PTTG1 and PTTG2, Based on Data from Starbase V3.0 Database
Supplementary Table S1. Correlation between the mutant p53-interacting partners and PTTG3P, PTTG1 and PTTG2, based on data from StarBase v3.0 database. PTTG3P PTTG1 PTTG2 Gene ID Coefficient-R p-value Coefficient-R p-value Coefficient-R p-value NF-YA ENSG00000001167 −0.077 8.59e-2 −0.210 2.09e-6 −0.122 6.23e-3 NF-YB ENSG00000120837 0.176 7.12e-5 0.227 2.82e-7 0.094 3.59e-2 NF-YC ENSG00000066136 0.124 5.45e-3 0.124 5.40e-3 0.051 2.51e-1 Sp1 ENSG00000185591 −0.014 7.50e-1 −0.201 5.82e-6 −0.072 1.07e-1 Ets-1 ENSG00000134954 −0.096 3.14e-2 −0.257 4.83e-9 0.034 4.46e-1 VDR ENSG00000111424 −0.091 4.10e-2 −0.216 1.03e-6 0.014 7.48e-1 SREBP-2 ENSG00000198911 −0.064 1.53e-1 −0.147 9.27e-4 −0.073 1.01e-1 TopBP1 ENSG00000163781 0.067 1.36e-1 0.051 2.57e-1 −0.020 6.57e-1 Pin1 ENSG00000127445 0.250 1.40e-8 0.571 9.56e-45 0.187 2.52e-5 MRE11 ENSG00000020922 0.063 1.56e-1 −0.007 8.81e-1 −0.024 5.93e-1 PML ENSG00000140464 0.072 1.05e-1 0.217 9.36e-7 0.166 1.85e-4 p63 ENSG00000073282 −0.120 7.04e-3 −0.283 1.08e-10 −0.198 7.71e-6 p73 ENSG00000078900 0.104 2.03e-2 0.258 4.67e-9 0.097 3.02e-2 Supplementary Table S2. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Supplementary Materials
Supplementary materials Supplementary Table S1: MGNC compound library Ingredien Molecule Caco- Mol ID MW AlogP OB (%) BBB DL FASA- HL t Name Name 2 shengdi MOL012254 campesterol 400.8 7.63 37.58 1.34 0.98 0.7 0.21 20.2 shengdi MOL000519 coniferin 314.4 3.16 31.11 0.42 -0.2 0.3 0.27 74.6 beta- shengdi MOL000359 414.8 8.08 36.91 1.32 0.99 0.8 0.23 20.2 sitosterol pachymic shengdi MOL000289 528.9 6.54 33.63 0.1 -0.6 0.8 0 9.27 acid Poricoic acid shengdi MOL000291 484.7 5.64 30.52 -0.08 -0.9 0.8 0 8.67 B Chrysanthem shengdi MOL004492 585 8.24 38.72 0.51 -1 0.6 0.3 17.5 axanthin 20- shengdi MOL011455 Hexadecano 418.6 1.91 32.7 -0.24 -0.4 0.7 0.29 104 ylingenol huanglian MOL001454 berberine 336.4 3.45 36.86 1.24 0.57 0.8 0.19 6.57 huanglian MOL013352 Obacunone 454.6 2.68 43.29 0.01 -0.4 0.8 0.31 -13 huanglian MOL002894 berberrubine 322.4 3.2 35.74 1.07 0.17 0.7 0.24 6.46 huanglian MOL002897 epiberberine 336.4 3.45 43.09 1.17 0.4 0.8 0.19 6.1 huanglian MOL002903 (R)-Canadine 339.4 3.4 55.37 1.04 0.57 0.8 0.2 6.41 huanglian MOL002904 Berlambine 351.4 2.49 36.68 0.97 0.17 0.8 0.28 7.33 Corchorosid huanglian MOL002907 404.6 1.34 105 -0.91 -1.3 0.8 0.29 6.68 e A_qt Magnogrand huanglian MOL000622 266.4 1.18 63.71 0.02 -0.2 0.2 0.3 3.17 iolide huanglian MOL000762 Palmidin A 510.5 4.52 35.36 -0.38 -1.5 0.7 0.39 33.2 huanglian MOL000785 palmatine 352.4 3.65 64.6 1.33 0.37 0.7 0.13 2.25 huanglian MOL000098 quercetin 302.3 1.5 46.43 0.05 -0.8 0.3 0.38 14.4 huanglian MOL001458 coptisine 320.3 3.25 30.67 1.21 0.32 0.9 0.26 9.33 huanglian MOL002668 Worenine -

Supplementary Data Table 1. Genes Upregulated in N-Myc-Overexpressing Mouse Mac1+/Gr1+ BM Cells
Supplementary Data Table 1. Genes upregulated in N-Myc-overexpressing mouse Mac1+/Gr1+ BM cells Probeset C-myc / N-myc / N-myc / C- Gene Title Representative 430v2 Vector Fold Vector Fold myc Fold Public ID Change Change Change 1435368_a_at 2.3 4.6 2.1 poly (ADP-ribose) polymerase family, member 1 BB767586 1455648_at 1.3 3.0 2.1 similar to reduced expression 2 /// similar to reduced expression 2 BG244780 1438973_x_at 2.5 9.8 4.0 gap junction membrane channel protein alpha 1 BB043407 1419915_at 2.0 3.0 2.1 DNA segment, Chr 10, ERATO Doi 438, expressed AW538011 1454842_a_at 1.6 4.0 2.3 UDP-GalNAc:betaGlcNAc beta 1,3-galactosaminyltransferase, AI853240 polypeptide 2 1436704_x_at 2.1 9.2 3.2 methylenetetrahydrofolate dehydrogenase (NADP+ dependent), AV215673 methenyltetrahydrofolate cyclohydrolase, formyltetrahydrofolate synthase 1423142_a_at 2.0 2.5 2.1 GTP binding protein 4 AI987834 1420043_s_at 2.5 5.7 2.8 THO complex 1 AW107924 1439444_x_at 1.5 4.3 2.5 transmembrane emp24-like trafficking protein 10 (yeast) /// similar to AV213456 transmembrane trafficking protein 1438610_a_at 1.9 4.9 2.3 Crystallin, zeta BB793369 1434291_a_at 2.5 4.3 2.8 small EDRK-rich factor 1 AA709993 1422716_a_at 2.8 6.5 2.6 acid phosphatase 1, soluble AW554436 1447895_x_at -1.3 2.3 2.6 PAN3 polyA specific ribonuclease subunit homolog (S. cerevisiae) AV368189 1434097_at 1.5 3.2 2.5 Transcribed locus BM218328 1420982_at 1.1 3.5 2.6 RNA-binding region (RNP1, RRM) containing 2 NM_133242 1433853_at 2.6 7.5 2.6 mindbomb homolog 1 (Drosophila) BG063791 1419824_a_at 1.6 4.0 2.1 RIKEN cDNA A230062G08 gene AI875121 1453797_at 7.5 14.9 2.1 phosphatase, orphan 2 AK010147 1440803_x_at 2.3 4.0 2.3 tachykinin receptor 3 BB498416 1455737_at -2.0 1.1 2.8 RIKEN cDNA C030002B11 gene AU040848 1450954_at -1.5 2.8 4.6 YME1-like 1 (S. -

Supplementary Methods
Supplementary methods Human lung tissues and tissue microarray (TMA) All human tissues were obtained from the Lung Cancer Specialized Program of Research Excellence (SPORE) Tissue Bank at the M.D. Anderson Cancer Center (Houston, TX). A collection of 26 lung adenocarcinomas and 24 non-tumoral paired tissues were snap-frozen and preserved in liquid nitrogen for total RNA extraction. For each tissue sample, the percentage of malignant tissue was calculated and the cellular composition of specimens was determined by histological examination (I.I.W.) following Hematoxylin-Eosin (H&E) staining. All malignant samples retained contained more than 50% tumor cells. Specimens resected from NSCLC stages I-IV patients who had no prior chemotherapy or radiotherapy were used for TMA analysis by immunohistochemistry. Patients who had smoked at least 100 cigarettes in their lifetime were defined as smokers. Samples were fixed in formalin, embedded in paraffin, stained with H&E, and reviewed by an experienced pathologist (I.I.W.). The 413 tissue specimens collected from 283 patients included 62 normal bronchial epithelia, 61 bronchial hyperplasias (Hyp), 15 squamous metaplasias (SqM), 9 squamous dysplasias (Dys), 26 carcinomas in situ (CIS), as well as 98 squamous cell carcinomas (SCC) and 141 adenocarcinomas. Normal bronchial epithelia, hyperplasia, squamous metaplasia, dysplasia, CIS, and SCC were considered to represent different steps in the development of SCCs. All tumors and lesions were classified according to the World Health Organization (WHO) 2004 criteria. The TMAs were prepared with a manual tissue arrayer (Advanced Tissue Arrayer ATA100, Chemicon International, Temecula, CA) using 1-mm-diameter cores in triplicate for tumors and 1.5 to 2-mm cores for normal epithelial and premalignant lesions. -

Mitochondrial Dysfunction and Its Role in Tissue-Specific Cellular Stress
Review www.cell-stress.com Mitochondrial dysfunction and its role in tissue-specific cellular stress David Pacheu-Grau1,*, Robert Rucktäschel1 and Markus Deckers1,* 1 Department of Cellular Biochemistry, University Medical Center Göttingen, Germany. * Corresponding Authors: David Pacheu-Grau, University Medical Center Göttingen, Department of Cellular Biochemistry, Humboldtallee 23, 37073 Göttingen, Germany. Phone: +49-(0)551-394571; E-mail: [email protected]; Markus Deckers, University Medical Center Göttingen, Department of Cellular Biochemistry, Humboldtallee 23, 37073 Göttingen, Germany. Phone: +49-(0)551-395983; E-mail: [email protected] ABSTRACT Mitochondrial bioenergetics require the coordination of two dif- doi: 10.15698/cst2018.07.147 ferent and independent genomes. Mutations in either genome will affect mi- Received originally: 26.04.2018 tochondrial functionality and produce different sources of cellular stress. De- in revised form: 13.06.2018, Accepted 14.06.2018, pending on the kind of defect and stress, different tissues and organs will be Published 13.07.2018. affected, leading to diverse pathological conditions. There is no curative ther- apy for mitochondrial diseases, nevertheless, there are strategies described that fight the various stress forms caused by the malfunctioning organelles. Keywords: mitochondrial dysfunction, Here, we will revise the main kinds of stress generated by mutations in mito- cellular stress, mitochondrial chondrial genes and outline several ways of fighting this stress. pathology, therapy. Abbreviations: ADOA – autosomal dominant optic atrophy, AROA – autosomal recessive optic atrophy, ARS – aminoacyl-tRNA synthetase, CL – cardiolipin, CRISPR – clustered regularly interspaced short palindromic repeats, LHON – Leber’s hereditary optic neuropathy, mt - mitochondrial OXPHOS – oxidative phosphorylation, ROS – reactive oxygen species.