ISSUE XXI May-Jun 2007
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Erythrocytes: Overview, Morphology, Quantity by AH Rebar Et
In: A Guide to Hematology in Dogs and Cats, Rebar A.H., MacWilliams P.S., Feldman B.F., Metzger F.L., Pollock R.V.H. and Roche J. (Eds.). Publisher: Teton NewMedia, Jackson WY (www.veterinarywire.com). Internet Publisher: International Veterinary Information Service, Ithaca NY (www.ivis.org), 8-Feb-2005; A3304.0205 Erythrocytes: Overview, Morphology, Quantity A.H. Rebar1, P.S. MacWilliams2, B.F. Feldman 3, F.L. Metzger 4, R.V.H. Pollock 5 and J. Roche 6 1Dept of Veterinary Pathobiology, School of Veterinary Medicine, Purdue University, IN,USA. 2Dept of Pathobiological Sciences, School of Veterinary Medicine, University of Wisconsin, WI, USA. 3Dept of Biomedical Sciences & Pathobiology, VA-MD - Regional College of Veterinary Medicine, Virginia Tech, VA, USA. 4Metzger Animal Hospital,State College,PA, USA. 5Fort Hill Company, Montchanin, DE, USA. 6 Hematology Systems, IDEXX Laboratories, Westbrook, ME, USA. Overview Production Red blood cells (RBC) are produced in the bone marrow. Numbers of circulating RBCs are affected by changes in plasma volume, rate of RBC destruction or loss, splenic contraction, erythropoietin (EPO) secretion, and the rate of bone marrow production. A normal PCV is maintained by an endocrine loop that involves generation and release of erythropoietin (EPO) from the kidney in response to renal hypoxia. Erythropoietin stimulates platelet production as well as red cell production. However, erythropoietin does not stimulate white blood cell (WBC) production. Erythropoiesis and RBC numbers are also affected by hormones from the adrenal cortex, thyroid, ovary, testis, and anterior pituitary. Destruction Red cells have a finite circulating lifespan. In dogs, the average normal red cell circulates approximately 100 days. -

Complete Blood Count in Primary Care
Complete Blood Count in Primary Care bpac nz better medicine Editorial Team bpacnz Tony Fraser 10 George Street Professor Murray Tilyard PO Box 6032, Dunedin Clinical Advisory Group phone 03 477 5418 Dr Dave Colquhoun Michele Cray free fax 0800 bpac nz Dr Rosemary Ikram www.bpac.org.nz Dr Peter Jensen Dr Cam Kyle Dr Chris Leathart Dr Lynn McBain Associate Professor Jim Reid Dr David Reith Professor Murray Tilyard Programme Development Team Noni Allison Rachael Clarke Rebecca Didham Terry Ehau Peter Ellison Dr Malcolm Kendall-Smith Dr Anne Marie Tangney Dr Trevor Walker Dr Sharyn Willis Dave Woods Report Development Team Justine Broadley Todd Gillies Lana Johnson Web Gordon Smith Design Michael Crawford Management and Administration Kaye Baldwin Tony Fraser Kyla Letman Professor Murray Tilyard Distribution Zane Lindon Lyn Thomlinson Colleen Witchall All information is intended for use by competent health care professionals and should be utilised in conjunction with © May 2008 pertinent clinical data. Contents Key points/purpose 2 Introduction 2 Background ▪ Haematopoiesis - Cell development 3 ▪ Limitations of reference ranges for the CBC 4 ▪ Borderline abnormal results must be interpreted in clinical context 4 ▪ History and clinical examination 4 White Cells ▪ Neutrophils 5 ▪ Lymphocytes 9 ▪ Monocytes 11 ▪ Basophils 12 ▪ Eosinophils 12 ▪ Platelets 13 Haemoglobin and red cell indices ▪ Low haemoglobin 15 ▪ Microcytic anaemia 15 ▪ Normocytic anaemia 16 ▪ Macrocytic anaemia 17 ▪ High haemoglobin 17 ▪ Other red cell indices 18 Summary Table 19 Glossary 20 This resource is a consensus document, developed with haematology and general practice input. We would like to thank: Dr Liam Fernyhough, Haematologist, Canterbury Health Laboratories Dr Chris Leathart, GP, Christchurch Dr Edward Theakston, Haematologist, Diagnostic Medlab Ltd We would like to acknowledge their advice, expertise and valuable feedback on this document. -

Red Blood Cell Morphology in Patients with Β-Thalassemia Minor
J Lab Med 2017; 41(1): 49–52 Short Communication Carolin Körber, Albert Wölfler, Manfred Neubauer and Christoph Robier* Red blood cell morphology in patients with β-thalassemia minor DOI 10.1515/labmed-2016-0052 Keywords: β-thalassemia minor; erythrocytes; red blood Received July 11, 2016; accepted October 20, 2016; previously published cells; red blood cell morphology. online December 10, 2016 Abstract In β-thalassemias, the examination of a peripheral blood (PB) smear may provide relevant clues to initial diagnosis. Background: A systematic analysis of the occurrence of Complete laboratory investigation consists of the determina- red blood cell (RBC) abnormalities in β-thalassemia minor tion of the complete blood count, assessment of red blood has not been performed to date. This study aimed to iden- cell (RBC) morphology, high performance liquid chroma- tify and quantify the frequency of RBC abnormalities in tography (HPLC), hemoglobin electrophoresis and, where patients with β-thalassemia minor. necessary, DNA analysis [1]. Especially in the clinically Methods: We examined blood smears of 33 patients with severe forms referred to as β-thalassemia major and interme- β-thalassemia minor by light microscopy for the occur- dia, RBC abnormalities are often markedly apparent [2]. In rence of 15 defined RBC abnormalities. In the case of posi- β-thalassemia minor, also called β-thalassemia trait, the car- tivity, the abnormal cells/20 high power fields (HPF) at riers are usually clinically asymptomatic, showing persistent 1000-fold magnification were counted. microcytosis and hypochromia or mild microcytic anemia [1, Results: Anisocytosis, poikilocytosis and target cells 3]. The PB smear may show microcytosis, hypochromia and, (median 42/20 HPF) were observed in all, and ovalocytes infrequently, poikilocytosis [2]. -

10 11 Cyto Slides 81-85
NEW YORK STATE CYTOHEMATOLOGY PROFICIENCY TESTING PROGRAM Glass Slide Critique ~ November 2010 Slide 081 Diagnosis: MDS to AML 9 WBC 51.0 x 10 /L 12 Available data: RBC 3.39 x 10 /L 72 year-old female Hemoglobin 9.6 g/dL Hematocrit 29.1 % MCV 86.0 fL Platelet count 16 x 109 /L The significant finding in this case of Acute Myelogenous Leukemia (AML) was the presence of many blast forms. The participant median for blasts, all types was 88. The blast cells in this case (Image 081) are large, irregular in shape and contain large prominent nucleoli. It is difficult to identify a blast cell as a myeloblast without the presence of an Auer rod in the cytoplasm. Auer rods were reported by three participants. Two systems are used to classify AML into subtypes, the French- American-British (FAB) and the World Health Organization (WHO). Most are familiar with the FAB classification. The WHO classification system takes into consideration prognostic factors in classifying AML. These factors include cytogenetic test results, patient’s age, white blood cell count, pre-existing blood disorders and a history of treatment with chemotherapy and/or radiation therapy for a prior cancer. The platelet count in this case was 16,000. Reduced number of platelets was correctly reported by 346 (94%) of participants. Approximately eight percent of participants commented that the red blood cells in this case were difficult to evaluate due to the presence of a bluish hue around the red blood cells. Comments received included, “On slide 081 the morphology was difficult to evaluate since there was a large amount of protein surrounding RBC’s”, “Slide 081 unable to distinguish red cell morphology due to protein” and “Unable to adequately assess morphology on slide 081 due to poor stain”. -

Research Article
z Available online at http://www.journalcra.com INTERNATIONAL JOURNAL OF CURRENT RESEARCH International Journal of Current Research Vol. 9, Issue, 12, pp.62497-62502, December, 2017 ISSN: 0975-833X RESEARCH ARTICLE INCLUSION BODIES - A REVIEW 1Dr. Mrunalini Mahesh Dadpe, 2, *Dr. Sourab Kumar, 3Dr. Mahesh Dadpe, 4Dr. Payoshnee Bhalinge Jadhav, 5Dr. Abhishek Jadhav and 6Dr. Shilpi Suman 1, 4Department of Oral Pathology, M A Rangoonwala Dental College, Aazam Campus, Camp, Pune 411001, India 2, 5, 6Department of oral Pathology, D.Y. Patil School of Dentistry, Nerul, Navi Mumbai 400706, India 3MIDSR Dental College, Vishwanathpuram, Amba Jogai Road, Latur 413531, India ARTICLE INFO ABSTRACT Article History: The word inclusion means incorporation. Inclusion bodies are nuclear or cytoplasmic aggregates of Received 16th September, 2017 stainable substances which are usually ‘proteins’. They typically represent sites of viral multiplication Received in revised form in bacteria or in a eukaryotic cell and usually consist of viral capsid proteins. Inclusion bodies are 17th October, 2017 typically identified within a cell by their different appearance. Accepted 25th November, 2017 Published online 27th December, 2017 Key words: Proteins, Viral, Types, Structures Copyright © 2017, Mrunalini Mahesh Dadpe et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Citation: Dr. Mrunalini Mahesh Dadpe, Dr. Sourab Kumar, Dr. Mahesh Dadpe, Dr. Payoshnee Bhalinge Jadhav, Dr. Abhishek Jadhav and Dr. Shilpi Suman, 2017. “Inclusion Bodies - A Review”, International Journal of Current Research, 9, (12), 62497-62502. Classification INTRODUCTION Viral inclusion bodies Inclusion bodies (IB) can also be hallmarks of genetic diseases, as in the case of Neuronal Inclusion bodies in neural disorders, A. -
Blood Lab First Week
Blood Lab First Week This is a self propelled powerpoint study atlas of blood cells encountered in examination of the peripheral blood smear. It is a requirement of this course that you begin review of these slides with the first day of class in order to familiarize yourself with terms used in describing peripheral blood morphology. Laboratory final exam questions are derived directly from these slides. The content of these slides may duplicate slides (1-37) listed on the Hematopathology Website. You must familiarize yourself with both sets of slides in order to have the best learning opportunity. Before Beginning This Slide Review • Please read the Laboratory information PDF under Laboratory Resources file to learn about – Preparation of a blood smear – How to select an area of the blood smear for review of morphology and how to perform a white blood cell differential – Platelet estimation – RBC morphology descriptors • Anisocytosis • Poikilocytosis • Hypochromia • Polychromatophilia Normal blood smear. Red blood cells display normal orange pink cytoplasm with central pallor 1/3-1/2 the diameter of the red cell. There is mild variation in size (anisocytosis) but no real variation in shape (poikilocytosis). To the left is a lymphocyte. To the right is a typical neutrophil with the usual 3 segmentations of the nucleus. Med. Utah pathology Normal blood: thin area Ref 2 Normal peripheral blood smear. This field is good for exam of cell morphology, although there are a few minor areas of overlap of red cells. Note that most cells are well dispersed and the normal red blood cell central pallor is noted throughout the smear. -

E-Learn LAB — RCD 1708
e-Learn LAB — Hemoglobinopathy Based on IQMH Centre for Proficiency Testing Survey RCD-1708-WB Confidence. Elevated. © Institute for Quality Management in Healthcare 1 Disclaimer and Copyright Disclaimer This document contains content developed by IQMH. IQMH’s work is guided by the current best available evidence at the time of publication. The application and use of this document is the responsibility of the user, and IQMH assumes no liability resulting from any such application or use. This document may be reproduced without permission for non-commercial purposes only and provided that appropriate credit is given to IQMH. Copyright The reader is cautioned not to take any single item, or part thereof, of this document out of context. Information presented in this document is the sole property and copyright of the Institute for Quality Management in Healthcare (IQMH). The logos and/or symbols used are the property of IQMH or other third parties. © Institute for Quality Management in Healthcare. All rights reserved. Confidence. Elevated. © Institute for Quality Management in Healthcare 2 Focus of this Presentation • This is a case study of a hemoglobinopathy investigation to familiarize participants with the laboratory features of the unstable hemoglobins, as well as the pathophysiology of common red cell inclusions. • You will be presented with clinical information, images, and laboratory results and will be prompted with self- learning questions. Confidence. Elevated. © Institute for Quality Management in Healthcare 3 Credits Case and discussion provided by members of the 2017 IQMH Hematology Scientific Committee, and the IQMH Consultant Technologist. Confidence. Elevated. © Institute for Quality Management in Healthcare 4 Clinical Information A 14-year-old female is being assessed for gall stones. -
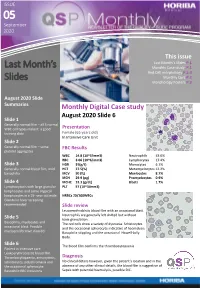
Last Month's Slides
ISSUE 05ISSUE September 2020 This issue Last Month’s Slides P.1 Last Month’s Monthly Case study P.1 Red Cell morphology P.2-3 Slides Monthly Quiz P.2 Morphology Posters P.3 August 2020 Slide Summaries Monthly Digital Case study August 2020 Slide 6 Slide 1 Generally normal film – all 5 normal WBC cell types make it a good Presentation training slide Female (65 years old) In Intensive Care Unit Slide 2 Generally normal film – some FBC Results platelet aggregates WBC 14.8 (10^3/mm3) Neutrophils 53.0% RBC 3.06 (10^6/mm3) Lymphocytes 17.4% Slide 3 HGB 91(g/L) Monocytes 6.1% Generally normal blood film, mild HCT 27.5(%) Metamyelocytes 12.2% basophilia MCV 90 (fL) Myelocytes 8.7% MCH 29.9 (pg) Promyelocytes 0.9% Slide 4 MCHC 33.3 (g/dL) Blasts 1.7% Lymphocytosis with large granular PLT 57 (10^3/mm3) lymphocytes and some atypical lymphocytes in a 19- year old male. NRBCs 20/100WBCs Glandular fever screening recommended Slide review Leucoerythroblstic blood film with an occasional blast. Neutrophils are generally left shifted but without Slide 5 toxic granulation. Basophilia, myelocytes and The red cells show a variety of dyscrasia. Schistocytes occasional blast. Possible and the occasional spherocyte indicative of haemolysis. myeloproliferative disorder Basophilic stippling and the occasional Howell-Jolly Body. Slide 6 The blood film confirms the thrombocytopaenia Patient in intensive care Leukoerythroblastic blood film. Thrombocytopaenia, anisocytosis, Diagnosis schistocytes, polychromasia and No clinical details however, given the patient’s location and in the the occasional spherocyte. -

Hematology Assignment
Hematology Assignment This unit is big, and mastery of the material requires a combination of reading the book, reviewing lecture notes and especially attention to the online exercises. It covers RBC and WBC disorders, problems of coagulation and diseases of the lymph nodes. Do not wait until week before the exam to try and do the reading. All of the material in this unit will be covered on the second exam, and it’s a bunch. You’ll be sunk if you put reading and online assignments off until the just few weeks before the exam. Here’s the scoop on just the hematology unit, the immunopathology comes later. Big Robbins: chapters 13 and 14. Little Robbins: Chapter 11 Wheater: Hematopoietic Slides: For the blood smears, the entire set is online. There are no slides in your box. For the lymph nodes, there are slides in your box and online. There are four online exercises for hematology unit, two cases and two tutorials. The tutorials are rather large but absolutely necessary. Don’t flush these or try to rush through them. Online stuff: Case 11, Mr. Herbert: A man complaining of lethargy. Module 24, Coagulation tutorial Module 19, Leukemia review Case 17, Mrs. Talbot: Woman with a neck mass. Slides and TBL stuff: There are no formal TBLs for this unt. Rather the blood smear section of the slides will serve that purpose. Approach of these cases as if you will see them, their histories and lab values in case studies on the written exam. The reason is, you will. -

Peripheral Blood Smear Examination
Board Review- Part 1: Benign HemePath Peripheral Blood Smear Examination Elevated MCV = Macrocytosis MCV > 100um3 • B12/Folate deficiency, aplastic anemia, MDS • Autoimmune hemolytic anemia • Liver disease, hypothyroidism, alcoholism • Cold agglutinin disease Decreased MCV = Microcytosis MCV < 80um3 • Iron deficiency • Thalassemias • Anemia of chronic disease • Hemoglobinopathies – C, E, S, D Iron Panel Interpretation Cause of Serum TIBC Percent anemia iron saturation Iron ↓ ↑ ↓ deficiency Thalassemias ↑ / N ↓ / N ↑ / N Sideroblastic ↑ ↓ / N ↑ anemia Chronic N/↓ ↓ N disease Pathologic Red Blood Cells in Peripheral Blood Smears Type of Cell Underlying Change Disease States Acanthocyte (spur cell) Altered cell membrane lipids Abetalipoproteinemia, liver disease, postsplenectomy, McLeod phenotype Bite Cell (degmacyte) Heinz body pitting by spleen G6PD deficiency, drug-induced oxidant hemolysis Ovalocyte (elliptocyte) Abnormal cytoskeletal proteins Hereditary elliptocytosis Rouleaux Circulating paraprotein Paraproteinemia Schistocyte (helmet cell) Mechanical destruction in DIC, TTP, HUS, prosthetic heart microvasculature valves Spherocyte Decreased membrane Hereditary sphereocytosis, redundancy immunohemolytic anemia (warm Ab) Stomatocyte Membrane defect with Hereditary stomatocytosis, liver abnormal cation permeation disease Target Cell (codocyte) Increased redundancy of cell Liver disease, beta thalassemia membrane postsplenectomy, Hgb C/D/E/S Burr Cell (ecchinocyte) Altered membrane lipids Usually artifactual but maybe uremia Tear Drop -
Hematology for Family Practice When to Treat and When to Refer
Hematology for Family Practice When to treat and when to refer Karen deGenevieve MSN, FNP,BC OCN Objectives: 1. Identify types of anemia's by analyzing indices, and appropriate tests. 2. Understand manual differential and terminology. 3. Discuss abnormalities in platelets and white cells, and determine appropriate testing. Objectives continued: 4. Discuss treatment options for hematologic conditions and medication management. 5. Know when to refer. 1. Anemia's and Erythrocytosis 2. Low platelets and High platelets 3. Leukopenia's and Leukocytosis How long do cells live? • Red blood cells live approximately 120 days. • Platelets live 8 -11 days. • White blood cells live about 4 days. There are millions of RBCs in just one drop of blood. People who live at higher altitudes have more (like in the mountains of Peru). They are produced in the bone marrow of large bones at a rate of 2 million per second. In the minute it took you to read this, you made 120 million of them! Anemia’s And Erythrocytosis First thing to do with an abnormal CBC is to repeat it and get a smear to pathology, manual diff, and reticulocyte count. MICROCYTOSIS: Low MCV (mean corpuscular volume) under 80. Low MCH (mean corpuscular hemoglobin) under 27. Low MCHC (mean corpuscular hemoglobin concentration) under 30. MACROCYTOSIS: High MCV over 93 High MCH over 33 High MCHC over 37 NORMOCYTIC ANEMIA: NOMAL INDICIES DEFINITIONS Reticulocyte: The youngest of the circulating red cells, normally they comprise about 1% of the red cell population. They are increased in response to bleeding, or hemolysis, or in response to treatment with B 12, iron, of folic acid. -
A Laboratory Guide to Clinical Hematology
A Laboratory Guide to Clinical Hematology A Laboratory Guide to Clinical Hematology A Laboratory Guide to Clinical Hematology VALENTIN VILLATORO AND MICHELLE TO EDMONTON A Laboratory Guide to Clinical Hematology by Michelle To is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, except where otherwise noted. Please be aware that the content for the entirety of this eBook is subject to a creative common license: Attribution-NonCommercial 4.0 International (CC BY-NC 4.0) You are free to: Share — copy and redistribute the material in any medium or format Adapt — remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms. Under the following terms: Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use. NonCommercial — You may not use the material for commercial purposes. No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits. Contents Authors & Editors ................................................................................................................................... xii Creative Commons License and Citation ............................................................................................... xiii Contact Information and Feedback ........................................................................................................