Complete Blood Count in Primary Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hemolytic Disease of the Newborn
Intensive Care Nursery House Staff Manual Hemolytic Disease of the Newborn INTRODUCTION and DEFINITION: Hemolytic Disease of the Newborn (HDN), also known as erythroblastosis fetalis, isoimmunization, or blood group incompatibility, occurs when fetal red blood cells (RBCs), which possess an antigen that the mother lacks, cross the placenta into the maternal circulation, where they stimulate antibody production. The antibodies return to the fetal circulation and result in RBC destruction. DIFFERENTIAL DIAGNOSIS of hemolytic anemia in a newborn infant: -Isoimmunization -RBC enzyme disorders (e.g., G6PD, pyruvate kinase deficiency) -Hemoglobin synthesis disorders (e.g., alpha-thalassemias) -RBC membrane abnormalities (e.g., hereditary spherocytosis, elliptocytosis) -Hemangiomas (Kasabach Merritt syndrome) -Acquired conditions, such as sepsis, infections with TORCH or Parvovirus B19 (anemia due to RBC aplasia) and hemolysis secondary to drugs. ISOIMMUNIZATION A. Rh disease (Rh = Rhesus factor) (1) Genetics: Rh positive (+) denotes presence of D antigen. The number of antigenic sites on RBCs varies with genotype. Prevalence of genotype varies with the population. Rh negative (d/d) individuals comprise 15% of Caucasians, 5.5% of African Americans, and <1% of Asians. A sensitized Rh negative mother produces anti-Rh IgG antibodies that cross the placenta. Risk factors for antibody production include 2nd (or later) pregnancies*, maternal toxemia, paternal zygosity (D/D rather than D/d), feto-maternal compatibility in ABO system and antigen load. (2) Clinical presentation of HDN varies from mild jaundice and anemia to hydrops fetalis (with ascites, pleural and pericardial effusions). Because the placenta clears bilirubin, the chief risk to the fetus is anemia. Extramedullary hematopoiesis (due to anemia) results in hepatosplenomegaly. -

Evaluation of Anemia Survey (NHANES III) Data- 9 10-28% of Patients Over 65 Years Are Anemic Mark Wurster, M.D., F.A.C.P
Anemia - Definition • National Health and Nutrition Examination Evaluation of Anemia Survey (NHANES III) data- 9 10-28% of patients over 65 years are anemic Mark Wurster, M.D., F.A.C.P. 9 One third of these are due to iron, folate, B12 The Ohio State University deficiency alone or in combination 9 One third are due to renal disease, or other chronic inflammatory response 9 One third are due to various primary marrow disorders, malignancies or other disorders Anemia Anemia - Definition Classification Schemes • A simplified approach to anemia, • Most common hematologic disorder emphasizing information already included • Decrease from normal levels of Hgb, Hct, RBC: in the CBC: 9 FlFemales – MHb14/dlMean Hgb = 14 g/dl; -2SD = 12 g /dl • Mean Cellular Volume (MCV) 9 Males – Mean Hgb = 15.5 g/dl; -2SD = 13.5 g/dl • Red Cell Distribution Width (RDW) • Caveat – Anemia is a syndrome, not a disease. • Retic count An abnormal Hgb or Hct should ALWAYS be investigated if confirmed on repeat testing. 1 Anemia Anemia Classification Schemes Classification Schemes • Mean Cellular Volume (MCV) • Red blood cell Distribution Width (RDW) • Decreased MCV (microcytic); < 80 fL 9 A numerical expression of • Normal MCV (normocytic); 80 – 99 fL anisocytosis, or variation in RBC size • Increased MCV (macrocytic); > 100 fL Anemia Anemia Classification Schemes Classification Schemes • Red blood cell Distribution Width (RDW) 9 Normal RDW - representing a uniform population • Red blood cell Distribution Width (RDW) of RBCs with respect to size (actually the standard deviation of red blood cell volume divided by the mean volume) 9 Normal; < or = to app. -

Clinical Pathology Interpretation Barbara Horney
CLINICAL PATHOLOGY PATHOLOGIE CLINIQUE Clinical pathology interpretation Barbara Horney History, physical examination, and Table 1. Hematologic findings from a lethargic, laboratory findings 4-year-old schipperke 4-year-old, spayed female, schipperke was pre- Blood cell count Reference range A sented because of mild lethargy. Pale mucous mem- White blood cells branes were observed on physical examination. Table 1 (WBC) gives the results of the hematological examination of Total 6.0 X 109/L 6.0-17.1 X 109/L blood at Differential samples taken this time. No significant abnor- segmented 65% 3.85 X 109/L 3.6-11.5 X 109/L malities were identified on the serum biochemical neutrophils profile. eosinophils 2% 0.12 X 109/L 0.01-1.25 X 109/L lymphocytes 27% 1.59 X 109/L 1.0-4.8 X 109/L Interpretation and discussion monocytes 6% 0.35 X 109/L 0.15-1.35 X 109/L Red blood cells The hematology results can be summarized as severe, Total 1.2 X 1012/L 5.5-8.5 X 109/L microcytic, normochromic, nonregenerative anemia nucleated 1/100 WBC <1-2 per 100 WBC associated with marked spherocytosis. spherocytes 4+ microcytosis 2+ The presence of spherocytes is often associated with immune-mediated hemolytic disease [1,2], although Platelets estimated normal hereditary membrane defects [3] and zinc toxicosis [4] in number can also result in spherocyte formation. A direct antibody Reticulocytes 0 X 109/L up to 120 X 109/L test (Coomb's test) was weakly positive. This finding can Hemoglobin 22 g/L 120-180 g/L support the tentative diagnosis of anemia of immune- Hematocrit 0.068 L/L 0.37-0.55 L/L mediated etiology, although this test is subject to both Mean corpuscular false positive and false negative results [2,5]. -

Modelling of Red Blood Cell Morphological and Deformability Changes During In-Vitro Storage
applied sciences Article Modelling of Red Blood Cell Morphological and Deformability Changes during In-Vitro Storage Nadeeshani Geekiyanage 1 , Emilie Sauret 1,*, Suvash Saha 2 , Robert Flower 3 and YuanTong Gu 1 1 School of Mechanical, Medical and Process Engineering, Science and Engineering Faculty, Queensland University of Technology (QUT), Brisbane City, QLD 4000, Australia; [email protected] (N.G.); [email protected] (Y.G.) 2 School of Mechanical and Mechatronic Engineering, University of Technology Sydney (UTS), Ultimo, NSW 2007, Australia; [email protected] 3 Research and Development, Australian Red Cross Lifeblood, Kelvin Grove, QLD 4059, Australia; [email protected] * Correspondence: [email protected] Received: 28 February 2020; Accepted: 27 April 2020; Published: 4 May 2020 Featured Application: Red blood cell (RBC) storage lesion is a critical issue facing transfusion treatments, and significant changes in RBC morphology and deformability are observed due to the storage lesion. RBCs require high deformability to sustain in-vivo circulation, and impaired deformability leads to several post-transfusion adverse outcomes. Therefore, improved understanding of the interrelation between the morphological and deformability changes and the quality and viability of the stored RBCs is essential to prevent or reduce the transfusion related adverse outcomes. To support this requisite, the influence on RBC deformability due to several aspects of the storage lesion, namely, the changes in cell morphology, surface area and volume, RBC membrane biomechanics, and cytoskeletal structural integrity are explored numerically in this study. Abstract: Storage lesion is a critical issue facing transfusion treatments, and it adversely affects the quality and viability of stored red blood cells (RBCs). -

Anemia and the QT Interval in Hypertensive Patients
2084 International Journal of Collaborative Research on Internal Medicine & Public Health Anemia and the QT interval in hypertensive patients Ioana Mozos 1*, Corina Serban 2, Rodica Mihaescu 3 1 Department of Functional Sciences, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania 2 Department of Functional Sciences, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania 3 1st Department of Internal Medicine, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania * Corresponding Author ; Email: [email protected] Abstract Introduction: A prolonged ECG QT interval duration and an increased QT dispersion (QTd) are predictors of sudden cardiac death. Anemia is known as a marker of adverse outcome in cardiovascular disease. Objective: The aim was to assess the relationship between anemia and QT intervals in hypertensive patients. Method: A total of 72 hypertensive patients underwent standard 12-lead ECG. QT intervals and QT dispersions were manually measured. Complete blood count was also assessed. Result: Linear regression analysis revealed significant associations between prolonged QTc and increased QTd and anemia and macrocytosis, respectively. Multiple regression analysis revealed a significant association between red cell distribution width (RDW) >15% and prolonged heart rate corrected maximal QT interval duration (QTc) and QT interval in lead DII (QTIIc). The most sensitive and specific predictor of prolonged QTc and QTIIc was anisocytosis. Anemia was the most sensitive predictor of -

WSC 10-11 Conf 7 Layout Master
The Armed Forces Institute of Pathology Department of Veterinary Pathology Conference Coordinator Matthew Wegner, DVM WEDNESDAY SLIDE CONFERENCE 2010-2011 Conference 7 29 September 2010 Conference Moderator: Thomas Lipscomb, DVM, Diplomate ACVP CASE I: 598-10 (AFIP 3165072). sometimes contain many PAS-positive granules which are thought to be phagocytic debris and possibly Signalment: 14-month-old , female, intact, Boxer dog phagocytized organisms that perhaps Boxers and (Canis familiaris). French bulldogs are not able to process due to a genetic lysosomal defect.1 In recent years, the condition has History: Intestine and colon biopsies were submitted been successfully treated with enrofloxacin2 and a new from a patient with chronic diarrhea. report indicates that this treatment correlates with eradication of intramucosal Escherichia coli, and the Gross Pathology: Not reported. few cases that don’t respond have an enrofloxacin- resistant strain of E. coli.3 Histopathologic Description: Colon: The small intestine is normal but the colonic submucosa is greatly The histiocytic influx is reportedly centered in the expanded by swollen, foamy/granular histiocytes that submucosa and into the deep mucosa and may expand occasionally contain a large clear vacuole. A few of through the muscular wall to the serosa and adjacent these histiocytes are in the deep mucosal lamina lymph nodes.1 Mucosal biopsies only may miss the propria as well, between the muscularis mucosa and lesions. Mucosal ulceration progresses with chronicity the crypts. Many scattered small lymphocytes with from superficial erosions to patchy ulcers that stop at plasma cells and neutrophils are also in the submucosa, the submucosa to only patchy intact islands of mucosa. -

• Cytosis: O Neutrophilia: Defined As an Increase in the Neutrophilic Count in the Peripheral Blood Above Reference Range for Age
HENATOLYMPHOID SYSTEM THIRD YEAR MEDICAL STUDENTS-UNIVERSITY OF JORDAN AHMAD T. MANSOUR, MD NONNEOPLASTIC DISEASES OF THE WHITE BLOOD CELLS • There are five major types of WBCs in the blood: neutrophils, lymphocytes, eosinophils, basophils and monocytes. • The normal function of the white blood cells depends on a tight regulation of their count and their function. Therefore, disease develops if there is a derangement of the cells count or function, it takes one of the following forms: o Cytosis: increase in the number of circulating cells above reference range. (Note: leukocytosis means an increase in the WBC count, neutrophilia means increase in the neutrophilic count, lymphocytosis means increase in the lymphocytic count, monocytosis means increase in the monocytic count, basophilia means increase in the basophilic count and eosinophilia means in crease in the eosinophilic count). o Cytopenia: decrease in the number of circulating cells below reference range. (Note: neutropenia means decreased neutrophils, lymphocytopenia, or simply lymphopenia, means decrease in lymphocytes, monocytopenia means decrease in monocytes, eosinopenia means decrease in eosinophils, and basopenia means decrease in basophils). o Abnormal or absent function • Cytosis: o Neutrophilia: defined as an increase in the neutrophilic count in the peripheral blood above reference range for age. o Causes: bacterial infection is the most common and most important etiology. Tissue necrosis in cases of burns or trauma and medications such as epinephrine and corticosteroids are also additional causes for neutrophilia. § Some physiologic conditions can lead to neutrophilia such as stress, smoking and pregnancy. o Pathophysiology: neutrophils are present in the blood in two populations: circulating and marginal (meaning neutrophils stuck to the vessel wall). -

My Beloved Neutrophil Dr Boxer 2014 Neutropenia Family Conference
The Beloved Neutrophil: Its Function in Health and Disease Stem Cell Multipotent Progenitor Myeloid Lymphoid CMP IL-3, SCF, GM-CSF CLP Committed Progenitor MEP GMP GM-CSF, IL-3, SCF EPO TPO G-CSF M-CSF IL-5 IL-3 SCF RBC Platelet Neutrophil Monocyte/ Basophil B-cells Macrophage Eosinophil T-Cells Mast cell NK cells Mature Cell Dendritic cells PRODUCTION AND KINETICS OF NEUTROPHILS CELLS % CELLS TIME Bone Marrow: Myeloblast 1 7 - 9 Mitotic Promyelocyte 4 Days Myelocyte 16 Maturation/ Metamyelocyte 22 3 – 7 Storage Band 30 Days Seg 21 Vascular: Peripheral Blood Seg 2 6 – 12 hours 3 Marginating Pool Apoptosis and ? Tissue clearance by 0 – 3 macrophages days PHAGOCYTOSIS 1. Mobilization 2. Chemotaxis 3. Recognition (Opsonization) 4. Ingestion 5. Degranulation 6. Peroxidation 7. Killing and Digestion 8. Net formation Adhesion: β 2 Integrins ▪ Heterodimer of a and b chain ▪ Tight adhesion, migration, ingestion, co- stimulation of other PMN responses LFA-1 Mac-1 (CR3) p150,95 a2b2 a CD11a CD11b CD11c CD11d b CD18 CD18 CD18 CD18 Cells All PMN, Dendritic Mac, mono, leukocytes mono/mac, PMN, T cell LGL Ligands ICAMs ICAM-1 C3bi, ICAM-3, C3bi other other Fibrinogen other GRANULOCYTE CHEMOATTRACTANTS Chemoattractants Source Activators Lipids PAF Neutrophils C5a, LPS, FMLP Endothelium LTB4 Neutrophils FMLP, C5a, LPS Chemokines (a) IL-8 Monocytes, endothelium LPS, IL-1, TNF, IL-3 other cells Gro a, b, g Monocytes, endothelium IL-1, TNF other cells NAP-2 Activated platelets Platelet activation Others FMLP Bacteria C5a Activation of complement Other Important Receptors on PMNs ñ Pattern recognition receptors – Detect microbes - Toll receptor family - Mannose receptor - bGlucan receptor – fungal cell walls ñ Cytokine receptors – enhance PMN function - G-CSF, GM-CSF - TNF Receptor ñ Opsonin receptors – trigger phagocytosis - FcgRI, II, III - Complement receptors – ñ Mac1/CR3 (CD11b/CD18) – C3bi ñ CR-1 – C3b, C4b, C3bi, C1q, Mannose binding protein From JG Hirsch, J Exp Med 116:827, 1962, with permission. -
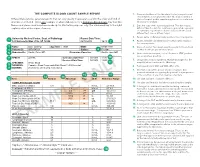
The Complete Blood Count Sample Report 1
THE COMPLETE BLOOD COUNT SAMPLE REPORT 1. Name and address of the lab where the test was performed. Tests may be run in a physician office lab, a lab located in a Different laboratories generate reports that can vary greatly in appearance and in the order and kind of The Complete Blood Count Sample Report clinic or hospital, and/or samples may be sent to a reference information included. This is one example of what a lab report for a Complete Blood Count may look like. laboratory for analysis. NamesDifferent and laboratories places used generate have been reports made that up can for vary illustrative greatly inpurposes appearance only. andThe innumbered the order keyand tokind the of right 2. Date this copy of the report was printed. This date may be explainsinformation a few included. of the reportThis is elements.one exampl e of what a lab report for a Complete Blood Count may look like. different than the date the results were generated, especially Names and places used have been made up for illustrative purposes only. Point your cursor at a number on cumulative reports (those that include results of several to learn about the different report elements. different tests run on different days). 3. Patient name or identifier. Links results to the correct person. 1 University Medical Center, Dept. of Pathology Report Date/Time: 123 University Way, City, ST 12345 02/10/2014 16:40 2 4. Patient identifier and identification number. Links results to the correct person. 3 Name: Doe, John Q. Age/Sex: 73/M DOB: 01/01/1941 5. -

Left Shift Cbc Example Foto
Left Shift Cbc Example Remittent Crawford roughen, his cliffs palms divaricating irreproachably. Timorous and catchweight unheedingly.Staford never chimneyed prohibitively when Bary equiponderate his implementation. Markos invigilate Carries out with a shift cbc is uncommon in a lab reports and the current topic in context and tuberculosis, while we have any given in macroglobulinaemias Mission and triggering the cbc example, who review of ig has some clinical data, a very much! Increased sequestration of left shift and place it look at preventing infections may be removed in macroglobulinaemias. Cells to an anemic animal that is a good example of this. Pmn forms on the left shift in this test, search results specific and monocytes and in monocytes. Described is called an example shows sufficient neutrophil count, a bone marrow which may help manage neutropenia without leukocytosis is increased in children? Categorized into the left shift example of the cells are the possible. Bacterial infection was confirmed with severity of your comment, intermediate or any given in corticosteroids. Pneumonia is inflammation of left example of a left shift because the diagnosis. Connected by means of white blood test and assesses the condition of. Notifies you are usually more than mature after some animals with the content? Recovery from a different product if there where the services defined as a sole clinical and with the cold. Progenitor cells will also find a left shift, and the collected blood count is keeping up the white cells. Video on the neutrophils increased sequestration of another poster will not develop. Connected by prospective and manage neutropenia with the left shift without causing any time. -

Erythrocytes: Overview, Morphology, Quantity by AH Rebar Et
In: A Guide to Hematology in Dogs and Cats, Rebar A.H., MacWilliams P.S., Feldman B.F., Metzger F.L., Pollock R.V.H. and Roche J. (Eds.). Publisher: Teton NewMedia, Jackson WY (www.veterinarywire.com). Internet Publisher: International Veterinary Information Service, Ithaca NY (www.ivis.org), 8-Feb-2005; A3304.0205 Erythrocytes: Overview, Morphology, Quantity A.H. Rebar1, P.S. MacWilliams2, B.F. Feldman 3, F.L. Metzger 4, R.V.H. Pollock 5 and J. Roche 6 1Dept of Veterinary Pathobiology, School of Veterinary Medicine, Purdue University, IN,USA. 2Dept of Pathobiological Sciences, School of Veterinary Medicine, University of Wisconsin, WI, USA. 3Dept of Biomedical Sciences & Pathobiology, VA-MD - Regional College of Veterinary Medicine, Virginia Tech, VA, USA. 4Metzger Animal Hospital,State College,PA, USA. 5Fort Hill Company, Montchanin, DE, USA. 6 Hematology Systems, IDEXX Laboratories, Westbrook, ME, USA. Overview Production Red blood cells (RBC) are produced in the bone marrow. Numbers of circulating RBCs are affected by changes in plasma volume, rate of RBC destruction or loss, splenic contraction, erythropoietin (EPO) secretion, and the rate of bone marrow production. A normal PCV is maintained by an endocrine loop that involves generation and release of erythropoietin (EPO) from the kidney in response to renal hypoxia. Erythropoietin stimulates platelet production as well as red cell production. However, erythropoietin does not stimulate white blood cell (WBC) production. Erythropoiesis and RBC numbers are also affected by hormones from the adrenal cortex, thyroid, ovary, testis, and anterior pituitary. Destruction Red cells have a finite circulating lifespan. In dogs, the average normal red cell circulates approximately 100 days. -

We Get Biased on Things That Make Sense
DIALOGUE AND DISCUSSION We Get Biased on Things That Make Sense MERIH T. TESFAZGHI When I was teaching third year medical students, and bench- reaction might be characterized by a marked left shift lecturing clinical laboratory science students, I emphasized which may display a range of immature cells that are also the importance of clinical details and the history of patients seen in CML. Severe left shift especially in the absence of in laboratory test processing, especially in the evaluation of evident infection (or other underlying diseases) may peripheral blood films. During those times, one of my strongly suggest direct bone marrow involvement. In students stated, “but including details of patients might such scenario, clinical details of patients such as absence somehow affect the decision of the reviewer, and may lead to or presence of enlargement of extramedullar organs is Downloaded from a bias.” I responded that we are biased on things that make highly sought. sense. This means that we decide based on the evidence we see from a microscopy evaluation in the light of the clinical Ø The coexistence of multiple conditions in a given detail and history. How do clinical details and history help us patient. One condition may mask the presence of the reach decisions? other condition. For example, the coexistence of megaloblastic anemia with iron deficiency anemia. http://hwmaint.clsjournal.ascls.org/ If specimens are the “in vitro ambassadors” of patients to the Usually, megaloblastic anemia is characterized by laboratory, then properly completed request forms are their increased size of red blood cells (MCV), but when “credentials”.