Anemia and the QT Interval in Hypertensive Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The QT Interval: How Long Is Too Long?
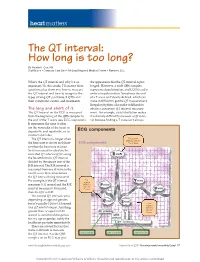
heart matters The QT interval: How long is too long? By Natalie K. Cox, RN Staff Nurse • Coronary Care Unit • McLeod Regional Medical Center • Florence, S.C. What’s the QT interval and why’s it so the appearance that the QT interval is pro- important? In this article, I’ll answer these longed. However, a wide QRS complex questions plus show you how to measure represents depolarization, and LQTS is a dis- the QT interval and how to recognize the order of repolarization. Sometimes the end types of long QT syndrome (LQTS) and of a T wave isn’t clearly defi ned, which can their symptoms, causes, and treatments. make it diffi cult to get the QT measurement. Irregular rhythms also make it diffi cult to The long and short of it obtain a consistent QT interval measure- The QT interval on the ECG is measured ment. For example, atrial fi brillation makes from the beginning of the QRS complex to it extremely diffi cult to measure a QT inter- the end of the T wave (see ECG components). val because fi nding a T wave isn’t always It represents the time it takes for the ventricles of the heart to depolarize and repolarize, or to ECG components contract and relax. The QT interval is longer when First positive deflection after the the heart rate is slower and short- ECG components P or Q wave er when the heart rate is faster. So it’s necessary to calculate the corrected QT interval (QTc) using the Bazett formula: QT interval divided by the square root of the R-R interval. -

Hemolytic Disease of the Newborn
Intensive Care Nursery House Staff Manual Hemolytic Disease of the Newborn INTRODUCTION and DEFINITION: Hemolytic Disease of the Newborn (HDN), also known as erythroblastosis fetalis, isoimmunization, or blood group incompatibility, occurs when fetal red blood cells (RBCs), which possess an antigen that the mother lacks, cross the placenta into the maternal circulation, where they stimulate antibody production. The antibodies return to the fetal circulation and result in RBC destruction. DIFFERENTIAL DIAGNOSIS of hemolytic anemia in a newborn infant: -Isoimmunization -RBC enzyme disorders (e.g., G6PD, pyruvate kinase deficiency) -Hemoglobin synthesis disorders (e.g., alpha-thalassemias) -RBC membrane abnormalities (e.g., hereditary spherocytosis, elliptocytosis) -Hemangiomas (Kasabach Merritt syndrome) -Acquired conditions, such as sepsis, infections with TORCH or Parvovirus B19 (anemia due to RBC aplasia) and hemolysis secondary to drugs. ISOIMMUNIZATION A. Rh disease (Rh = Rhesus factor) (1) Genetics: Rh positive (+) denotes presence of D antigen. The number of antigenic sites on RBCs varies with genotype. Prevalence of genotype varies with the population. Rh negative (d/d) individuals comprise 15% of Caucasians, 5.5% of African Americans, and <1% of Asians. A sensitized Rh negative mother produces anti-Rh IgG antibodies that cross the placenta. Risk factors for antibody production include 2nd (or later) pregnancies*, maternal toxemia, paternal zygosity (D/D rather than D/d), feto-maternal compatibility in ABO system and antigen load. (2) Clinical presentation of HDN varies from mild jaundice and anemia to hydrops fetalis (with ascites, pleural and pericardial effusions). Because the placenta clears bilirubin, the chief risk to the fetus is anemia. Extramedullary hematopoiesis (due to anemia) results in hepatosplenomegaly. -

Evaluation of Anemia Survey (NHANES III) Data- 9 10-28% of Patients Over 65 Years Are Anemic Mark Wurster, M.D., F.A.C.P
Anemia - Definition • National Health and Nutrition Examination Evaluation of Anemia Survey (NHANES III) data- 9 10-28% of patients over 65 years are anemic Mark Wurster, M.D., F.A.C.P. 9 One third of these are due to iron, folate, B12 The Ohio State University deficiency alone or in combination 9 One third are due to renal disease, or other chronic inflammatory response 9 One third are due to various primary marrow disorders, malignancies or other disorders Anemia Anemia - Definition Classification Schemes • A simplified approach to anemia, • Most common hematologic disorder emphasizing information already included • Decrease from normal levels of Hgb, Hct, RBC: in the CBC: 9 FlFemales – MHb14/dlMean Hgb = 14 g/dl; -2SD = 12 g /dl • Mean Cellular Volume (MCV) 9 Males – Mean Hgb = 15.5 g/dl; -2SD = 13.5 g/dl • Red Cell Distribution Width (RDW) • Caveat – Anemia is a syndrome, not a disease. • Retic count An abnormal Hgb or Hct should ALWAYS be investigated if confirmed on repeat testing. 1 Anemia Anemia Classification Schemes Classification Schemes • Mean Cellular Volume (MCV) • Red blood cell Distribution Width (RDW) • Decreased MCV (microcytic); < 80 fL 9 A numerical expression of • Normal MCV (normocytic); 80 – 99 fL anisocytosis, or variation in RBC size • Increased MCV (macrocytic); > 100 fL Anemia Anemia Classification Schemes Classification Schemes • Red blood cell Distribution Width (RDW) 9 Normal RDW - representing a uniform population • Red blood cell Distribution Width (RDW) of RBCs with respect to size (actually the standard deviation of red blood cell volume divided by the mean volume) 9 Normal; < or = to app. -

Long QT Syndrome: from Channels to Cardiac Arrhythmias
Long QT syndrome: from channels to cardiac arrhythmias Arthur J. Moss, Robert S. Kass J Clin Invest. 2005;115(8):2018-2024. https://doi.org/10.1172/JCI25537. Review Series Long QT syndrome, a rare genetic disorder associated with life-threatening arrhythmias, has provided a wealth of information about fundamental mechanisms underlying human cardiac electrophysiology that has come about because of truly collaborative interactions between clinical and basic scientists. Our understanding of the mechanisms that control the critical plateau and repolarization phases of the human ventricular action potential has been raised to new levels through these studies, which have clarified the manner in which both potassium and sodium channels regulate this critical period of electrical activity. Find the latest version: https://jci.me/25537/pdf Review series Long QT syndrome: from channels to cardiac arrhythmias Arthur J. Moss1 and Robert S. Kass2 1Heart Research Follow-up Program, Department of Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York, USA. 2Department of Pharmacology, Columbia University Medical Center, New York, New York, USA. Long QT syndrome, a rare genetic disorder associated with life-threatening arrhythmias, has provided a wealth of information about fundamental mechanisms underlying human cardiac electrophysiology that has come about because of truly collaborative interactions between clinical and basic scientists. Our understanding of the mecha- nisms that control the critical plateau and repolarization phases of the human ventricular action potential has been raised to new levels through these studies, which have clarified the manner in which both potassium and sodium channels regulate this critical period of electrical activity. -

Young Adults. Look for ST Elevation, Tall QRS Voltage, "Fishhook" Deformity at the J Point, and Prominent T Waves
EKG Abnormalities I. Early repolarization abnormality: A. A normal variant. Early repolarization is most often seen in healthy young adults. Look for ST elevation, tall QRS voltage, "fishhook" deformity at the J point, and prominent T waves. ST segment elevation is maximal in leads with tallest R waves. Note high take off of the ST segment in leads V4-6; the ST elevation in V2-3 is generally seen in most normal ECG's; the ST elevation in V2- 6 is concave upwards, another characteristic of this normal variant. Characteristics’ of early repolarization • notching or slurring of the terminal portion of the QRS wave • symmetric concordant T waves of large amplitude • relative temporal stability • most commonly presents in the precordial leads but often associated with it is less pronounced ST segment elevation in the limb leads To differentiate from anterior MI • the initial part of the ST segment is usually flat or convex upward in AMI • reciprocal ST depression may be present in AMI but not in early repolarization • ST segments in early repolarization are usually <2 mm (but have been reported up to 4 mm) To differentiate from pericarditis • the ST changes are more widespread in pericarditis • the T wave is normal in pericarditis • the ratio of the degree of ST elevation (measured using the PR segment as the baseline) to the height of the T wave is greater than 0.25 in V6 in pericarditis. 1 II. Acute Pericarditis: Stage 1 Pericarditis Changes A. Timing 1. Onset: Day 2-3 2. Duration: Up to 2 weeks B. Findings 1. -

The Relation Between Arterial Blood Pressure Variables and Ventricular Repolarization Parameters
860 International Journal of Collaborative Research on Internal Medicine & Public Health The relation between arterial blood pressure variables and ventricular repolarization parameters Ioana Mozos 1*, Corina Serban 2, Rodica Mihaescu 3 1 Department of Functional Sciences, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania, [email protected] 2 Department of Functional Sciences, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania 3 Department of Medical Semiology, “Victor Babes” University of Medicine and Pharmacy Timisoara, Romania ABSTRACT Introduction: Ventricular arrhythmia and sudden cardiac death risk are associated with prolonged electrocardiographic (ECG) QT and Tpeak-Tend intervals. Objective: To evaluate the influence of blood pressure variables on ventricular repolarization parameters, especially QT and Tpeak-Tend intervals. Method: Two groups of patients were enrolled in the study. The firs group included 77 patients, with essential hypertension, aged 62±12 years, 40% males. The control group included 56 patients, age and sex matched, with optimal, normal and high normal blood pressure. They underwent 12-lead ECG and ventricular repolarization parameters were assessed. QT intervals: QTmax (maximal QT interval duration), QTc (heart rate corrected QTmax), QTm (mean QT interval duration in all leads), QTIIc (heart rate corrected QT interval duration in lead DII), and T wave variables: T0e (maximal T wave duration), Tpe (maximal Tpeak-Tend interval) and Ta (maximal T wave amplitude) were manually measured. Arterial blood pressure variables: systolic (SBP), diastolic (DBP), mean arterial (MAP) and pulse pressure (PP), were recorded. Result: SBP was 139±24 mmHg, DBP 86±13 mmHg, MAP 103±15 mmHg, PP 53±16 mmHg, QTmax 430±51 ms, QTc 474±48 ms and Tpe 100±26 ms in the hypertensive group. -

SEED Haematology Sysmex Educational Enhancement and Development October 2012
SEED Haematology Sysmex Educational Enhancement and Development October 2012 The red blood cell indices The full blood count has been used in conjunction with the traditional red The complete blood count (CBC) is central to clinical deci- cell indices in order to narrow down the possible causes sion making. This makes it one of the commonest laboratory of anaemia in an individual patient. investigations performed worldwide. Whilst the definition of what constitutes an CBC is influenced by the number Impedance technology and type of parameters measured by different haematology The RBC, HCT and MCV are all closely interrelated as they analysers, the traditional red cell indices that are widely are derived from information obtained from the passage used to classify anaemias are common to all. of cells through the aperture of the impedance channel of an automated haematology analyser. The impedance The laboratory approach to anaemia technology is based on the principle that an electrical field, Anaemia is an extremely common global healthcare prob- created between two electrodes of opposite charge, can lem. However, anaemia is merely a symptom which can be used to count and determine the size of cells. Blood result from a multitude of causes. Effective treatment is cells are poor conductors of electricity. The diluent in which only possible if the underlying cause is correctly identified. they are suspended as they pass through the aperture To this end, several classification systems have been devis- during counting is an isotonic solution which is a good ed. The most useful and widely used classification system conductor of electricity. -

Review Article Management of Atrial Fibrillation in Critically Ill Patients
Hindawi Publishing Corporation Critical Care Research and Practice Volume 2014, Article ID 840615, 10 pages http://dx.doi.org/10.1155/2014/840615 Review Article Management of Atrial Fibrillation in Critically Ill Patients Mattia Arrigo, Dominique Bettex, and Alain Rudiger Cardiosurgical Intensive Care Unit, Institute of Anesthesiology, University Hospital Zurich, Raemistraße 100, 8091 Zurich, Switzerland Correspondence should be addressed to Alain Rudiger; [email protected] Received 29 September 2013; Revised 24 December 2013; Accepted 24 December 2013; Published 16 January 2014 AcademicEditor:MarcusJ.Schultz Copyright © 2014 Mattia Arrigo et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Atrial fibrillation (AF) is common in ICU patients and is associated with a two- to fivefold increase in mortality. This paper provides a reappraisal of the management of AF with a special focus on critically ill patients with haemodynamic instability. AF can cause hypotension and heart failure with subsequent organ dysfunction. The underlying mechanisms are the loss of atrial contraction and the high ventricular rate. In unstable patients, sinus rhythm must be rapidly restored by synchronised electrical cardioversion (ECV). If pharmacological treatment is indicated, clinicians can choose between the rate control and the rhythm control strategy. The optimal substance should be selected depending on its potential adverse effects. A beta-1 antagonist with a very short half-life (e.g., esmolol) is an advantage for ICU patients because the effect of beta-blockade on cardiovascular stability is unpredictable in those patients. -

Complete Blood Count in Primary Care
Complete Blood Count in Primary Care bpac nz better medicine Editorial Team bpacnz Tony Fraser 10 George Street Professor Murray Tilyard PO Box 6032, Dunedin Clinical Advisory Group phone 03 477 5418 Dr Dave Colquhoun Michele Cray free fax 0800 bpac nz Dr Rosemary Ikram www.bpac.org.nz Dr Peter Jensen Dr Cam Kyle Dr Chris Leathart Dr Lynn McBain Associate Professor Jim Reid Dr David Reith Professor Murray Tilyard Programme Development Team Noni Allison Rachael Clarke Rebecca Didham Terry Ehau Peter Ellison Dr Malcolm Kendall-Smith Dr Anne Marie Tangney Dr Trevor Walker Dr Sharyn Willis Dave Woods Report Development Team Justine Broadley Todd Gillies Lana Johnson Web Gordon Smith Design Michael Crawford Management and Administration Kaye Baldwin Tony Fraser Kyla Letman Professor Murray Tilyard Distribution Zane Lindon Lyn Thomlinson Colleen Witchall All information is intended for use by competent health care professionals and should be utilised in conjunction with © May 2008 pertinent clinical data. Contents Key points/purpose 2 Introduction 2 Background ▪ Haematopoiesis - Cell development 3 ▪ Limitations of reference ranges for the CBC 4 ▪ Borderline abnormal results must be interpreted in clinical context 4 ▪ History and clinical examination 4 White Cells ▪ Neutrophils 5 ▪ Lymphocytes 9 ▪ Monocytes 11 ▪ Basophils 12 ▪ Eosinophils 12 ▪ Platelets 13 Haemoglobin and red cell indices ▪ Low haemoglobin 15 ▪ Microcytic anaemia 15 ▪ Normocytic anaemia 16 ▪ Macrocytic anaemia 17 ▪ High haemoglobin 17 ▪ Other red cell indices 18 Summary Table 19 Glossary 20 This resource is a consensus document, developed with haematology and general practice input. We would like to thank: Dr Liam Fernyhough, Haematologist, Canterbury Health Laboratories Dr Chris Leathart, GP, Christchurch Dr Edward Theakston, Haematologist, Diagnostic Medlab Ltd We would like to acknowledge their advice, expertise and valuable feedback on this document. -

Red Blood Cell Morphology in Patients with Β-Thalassemia Minor
J Lab Med 2017; 41(1): 49–52 Short Communication Carolin Körber, Albert Wölfler, Manfred Neubauer and Christoph Robier* Red blood cell morphology in patients with β-thalassemia minor DOI 10.1515/labmed-2016-0052 Keywords: β-thalassemia minor; erythrocytes; red blood Received July 11, 2016; accepted October 20, 2016; previously published cells; red blood cell morphology. online December 10, 2016 Abstract In β-thalassemias, the examination of a peripheral blood (PB) smear may provide relevant clues to initial diagnosis. Background: A systematic analysis of the occurrence of Complete laboratory investigation consists of the determina- red blood cell (RBC) abnormalities in β-thalassemia minor tion of the complete blood count, assessment of red blood has not been performed to date. This study aimed to iden- cell (RBC) morphology, high performance liquid chroma- tify and quantify the frequency of RBC abnormalities in tography (HPLC), hemoglobin electrophoresis and, where patients with β-thalassemia minor. necessary, DNA analysis [1]. Especially in the clinically Methods: We examined blood smears of 33 patients with severe forms referred to as β-thalassemia major and interme- β-thalassemia minor by light microscopy for the occur- dia, RBC abnormalities are often markedly apparent [2]. In rence of 15 defined RBC abnormalities. In the case of posi- β-thalassemia minor, also called β-thalassemia trait, the car- tivity, the abnormal cells/20 high power fields (HPF) at riers are usually clinically asymptomatic, showing persistent 1000-fold magnification were counted. microcytosis and hypochromia or mild microcytic anemia [1, Results: Anisocytosis, poikilocytosis and target cells 3]. The PB smear may show microcytosis, hypochromia and, (median 42/20 HPF) were observed in all, and ovalocytes infrequently, poikilocytosis [2]. -

The Effect of Esmolol on Corrected-QT Interval, Corrected-QT
Rev Bras Anestesiol. 2015;65(1):34---40 REVISTA BRASILEIRA DE Official Publication of the Brazilian Society of Anesthesiology ANESTESIOLOGIA www.sba.com.br SCIENTIFIC ARTICLE The effect of esmolol on corrected-QT interval, corrected-QT interval dispersion changes seen during anesthesia induction in hypertensive patients taking an angiotensin-converting enzyme inhibitor ∗ Zahit C¸eker, Suna Akın Takmaz , Bülent Baltaci, Hülya Bas¸ar Department of Anesthesiolgy and Reanimation, Ankara Training and Research Hospital, Ministry of Health, Ankara, Turkey Received 16 January 2014; accepted 19 March 2014 Available online 1 May 2014 KEYWORDS Abstract Esmolol; Background and objectives: The importance of minimizing the exaggerated sympatho- adrenergic responses and QT interval and QT interval dispersion changes that may develop QT interval; due to laryngoscopy and tracheal intubation during anesthesia induction in the hypertensive QT dispersion; patients is clear. Esmolol decreases the hemodynamic response to laryngoscopy and intubation. ACE inhibitor However, the effect of esmolol in decreasing the prolonged QT interval and QT interval disper- sion as induced by laryngoscopy and intubation is controversial. We investigated the effect of esmolol on the hemodynamic, and corrected-QT interval and corrected-QT interval dispersion changes seen during anesthesia induction in hypertensive patients using angiotensin converting enzyme inhibitors. Methods: 60 ASA I---II patients, with essential hypertension using angiotensin converting enzyme inhibitors were included in the study. The esmolol group received esmolol at a bolus dose of 500 mcg/kg followed by a 100 mcg/kg/min infusion which continued until the 4th min after intubation. The control group received 0.9% saline similar to the esmolol group. -
Mechanism of Drug-Induced Qt Interval Prolongation
ABSTRACT Torsades de pointes (TdP) is a polymorphic ventricular tachycardia characterized by a distinctive pattern of undulating QRS complexes that twist around the isoelectric line. TdP is usually self-terminating or can subsequently degenerate into ventricular fibrillation, syncope, and sudden death. TdP has been associated with QT interval prolongation of the electrocardiogram; therefore, the QT interval has come to be recognized as a surrogate marker for the risk of TdP. International guidelines have been developed to harmonize both the preclinical and clinical studies for the evaluation of drug-induced TdP. However, currently preclinical in vitro and in vivo methods as well as biomarkers for proarrhythmias have been imperfect in predicting drug-induced TdP in humans. It is clear that relevant biomarkers together with appropriate models are needed to assess the arrhythmic risk of new chemical entities. The goal of the present dissertation is to create rabbit with myocardial failing heart as an in vivo animal model to predict TdP in humans and to determine mechanism(s) underlying TdP in this model. Electrocardiograms were recorded from bipolar transthoracic leads in 7 conscious healthy rabbits previously trained to rest quietly in slings. The RR and QT relationship, ii QT=2.4RR0.72 (r2=0.79, p < 0.001) was obtained by slowed the heart rate with 2.0 mg/kg zatebradine, and the algorithm for removing effect of heart rate on QT is QTc = QT/(RR)0.72. QTc lengthened significantly in all conscious rabbits given intravenous cisapride, dofetilide or haloperidol (p < 0.05), and QTc did not change with DMSO (vehicle control), propranolol or enalaprilat.