Dysrhythmias
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abdominal Coarctation in a Hypertensive Female Collegiate Basketball Player B Sloan, S Simons, a Stromwall
1of2 Br J Sports Med: first published as 10.1136/bjsm.2002.004176 on 23 September 2004. Downloaded from CASE REPORT Abdominal coarctation in a hypertensive female collegiate basketball player B Sloan, S Simons, A Stromwall ............................................................................................................................... Br J Sports Med 2004;38:e20 (http://www.bjsportmed.com/cgi/content/full/38/5/e20). doi: 10.1136/bjsm.2002.004176 INVESTIGATIONS The purpose of the preparticipation examination is to identify A chest radiograph was within normal limits except for rib health conditions that might adversely affect an athlete while notching. Complete blood count, electrolytes, serum urea participating in sport. Hypertension is the most common. This nitrogen and creatinine, and thyroid stimulating hormone case report details a female basketball player found to be were within normal limits. Urinalysis showed 300 mg/l hypertensive, and complaining of fatigue, at her prepartici- protein. Electrocardiography showed sinus bradycardia with pation physical examination. Presentation, diagnostics, occasional premature atrial contractions. Echocardiography treatment, and final outcome of coarctation involving the revealed mitral valve prolapse, no mitral insufficiency, and an abdominal aorta are summarised. ejection fraction of 69%. One month after the initial presentation, an aortogram was performed. It confirmed the diagnosis of abdominal coarcta- tion, which was about 10 cm in length and 6 mm in diameter reparticipation sports physical examinations have at its greatest stenotic segment. The left renal and coeliac become routine for many institutions at the high school arteries were mildly stenotic. Internal mammary and inter- Pand collegiate level. Their main purpose is to identify costal arteries were dilated. The superior and inferior health conditions that might adversely affect an athlete while mesenteric arteries were patent, and the distal abdominal participating in a particular activity. -
The QT Interval: How Long Is Too Long?
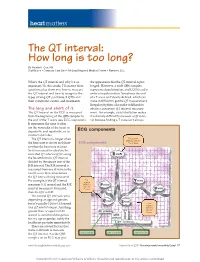
heart matters The QT interval: How long is too long? By Natalie K. Cox, RN Staff Nurse • Coronary Care Unit • McLeod Regional Medical Center • Florence, S.C. What’s the QT interval and why’s it so the appearance that the QT interval is pro- important? In this article, I’ll answer these longed. However, a wide QRS complex questions plus show you how to measure represents depolarization, and LQTS is a dis- the QT interval and how to recognize the order of repolarization. Sometimes the end types of long QT syndrome (LQTS) and of a T wave isn’t clearly defi ned, which can their symptoms, causes, and treatments. make it diffi cult to get the QT measurement. Irregular rhythms also make it diffi cult to The long and short of it obtain a consistent QT interval measure- The QT interval on the ECG is measured ment. For example, atrial fi brillation makes from the beginning of the QRS complex to it extremely diffi cult to measure a QT inter- the end of the T wave (see ECG components). val because fi nding a T wave isn’t always It represents the time it takes for the ventricles of the heart to depolarize and repolarize, or to ECG components contract and relax. The QT interval is longer when First positive deflection after the the heart rate is slower and short- ECG components P or Q wave er when the heart rate is faster. So it’s necessary to calculate the corrected QT interval (QTc) using the Bazett formula: QT interval divided by the square root of the R-R interval. -
Some Observations on the Atrial Sound*
15 Oktober 1960 S.A. TYDSKRIF VIR GENEESKUNDE 887 SOME OBSERVATIONS ON THE ATRIAL SOUND* JOHN R BARLOW, M.R, RCH., M.R.C.P., Department of Medicine, University of The WiTwaTersralld. Johallllesburg The atrial sound, also known as the fourth heart sound Emotional factors probably play a large part in this; the or. presystolic gallop, has been defined' as an audible P-G interval may quickly horten again on the introduction ibration occurring more than 0·07 second after the of an intravenous needle or imilar procedure. beginning of the P wave of the simultaneous electrocardio 3. EffeCT of respiration. Whereas re piration produce gram (ECG) but preceding the onset of the QRS complex. no effect on the P-G interval in patients with hyperten ion It has been shown' that, unrelated to any alteration in the or ischaemia. the atrial sound of cor pulmonale both in P-R interval, the position of the atrial sound varies in creases in intensity and occurs earlier in the cardiac cycle relation to the first heart sound and to the simultaneous during inspiration as compared with expiration (Fig. 4). ECG. 4. EffeCT of various procedures. Jt has already been Jt is the purpose of this paper to demonstrate this mentioned that the intravenous administration of hypo variation in the timing of the atrial sound and to discuss tensive drugs will increase the P-G interval in hypertensive some of the clinical implications resulting from this varia patients. The inhalation of amyl nitrite has a similar effect bility. in hypertension (Fig. 5), though a change in the P-G METHODS AND OBSERVATIO S interval is seldom seen in cases with ischaemic heart disease following inhalation of this drug. -

Chronotropic and Dromotropic Responses to Localized Glutamate Microinjections in the Rat $ Nucleus Ambiguus
brain research 1542 (2014) 93–103 Available online at www.sciencedirect.com www.elsevier.com/locate/brainres Research Report Chronotropic and dromotropic responses to localized glutamate microinjections in the rat $ nucleus ambiguus Karla N. Sampaio1,He´lder Mauad2, K. Michael Spyer, Timothy W. Fordn Division of Biosciences, Faculty of Life Sciences, University College London, Gower Street, London WC1E 6BT, UK article info abstract Article history: The cardioinhibitory effects of cardiac vagal motoneurons (CVMs) are mediated by Accepted 18 October 2013 activation of postganglionic neurons in the epicardial ganglia which have been shown to Available online 24 October 2013 exert functionally selective effects on heart rate and atrioventricular conduction in the rat. Here we investigate whether CVMs producing these responses may occupy different Keywords: rostrocaudal positions within the nucleus ambiguus. Excitation of CVMs was attempted Autonomic nervous system by microinjections of glutamate into the nucleus ambiguus of an arterially perfused Vagus nerve preparation in a grid extending over 2 mm in the rostrocaudal plane using the obex as a Nucleus ambiguus reference point. Microinjections were paired, one made during pacing to measure changes Heart rate in atrioventricular conduction (P-R interval) independent of changes in heart rate and the Glutamate other looking for changes in heart period (P-P interval) un-paced. Although evidence of a differential distribution was found in 7 cases, in the majority (13/20), sites producing maximal effects on both variables coincided. Maximal changes in atrioventricular conduc- tion resulted from more rostral sites in 6 cases and from a more caudal site in only one. Overall, the ratio of the change in atrioventricular conduction to the change in heart rate for a given site was significantly greater 1 mm rostral to the obex than at either end of the test grid. -

Clinical Significance of Exit Block*
Clinical Significance of Exit Block* IRANY M. DE AZEVEDO, M.D. YOSHIO WATANABE, M.D. LEONARD S. DREIFUS, M.D. From the Departments of Medicine, Physiology, and Biophysics, Hahnemann Medical College, Philadelphia, Pennsylvania The confinement of an ectopic discharge to its ily reserved for ectopic pacemakers, rather than the focus, and its consequent inability to invade the ad sinus node. jacent myocardium when falling outside of the re High Grade Atrioventricular Block. In vi rtu fractory period of the heart, is a well established ally all instances, exit block occurs in the presence phenomenon called "exit block." This cardiac ar of higher degrees of A-V block. Failure of the rhythmia was originally described by Kaufmann impulse to propagate from the subsidiary ectopic and Rothberger ( 8) to explain the failure of a para focus to either the ventricles, atria, or both is char systolic focus to activate the heart. All pacemakers acteristic of this form of exit block. Several exam are subject to exit block (9, 13, 15, 14, 11 , 16, 12, ples are illustrated. In figure 2, there is high grade 3, 10, 7, 1), however, by convention, conduction A-V block causing A-V dissociation. The atria are disturbances involving the sinus node (S-A block) under the control of the sinus node at a rate of 71 are usually excluded from this concept, and the term per minute, and the ventricles are controlled by a is reserved for ectopic pacemakers. Recent electro subsidiary ectopic pacemaker, probably originating physiological and clinical studies have shown that in the right bundle branch at a rate of approximately exit block may complicate reentrant arrhythmias and 40 per minute. -
The ECG Made Very Easy Indeed: a Beginner’S Guide
Part 1 The ECG made very easy indeed: a beginner’s guide The ECG made very easy indeed 1 What is an ECG? 1 The heart is a pump driven by intrinsic electrical When do you need an ECG? 1 impulses which make the heart beat. An ECG is a paper recording of that electrical activity. The ECG records where How to record an ECG 2 electrical impulses start and how they flow through the How to interpret an ECG: the basics 2 heart. It does not measure how well the heart is pumping. The electrical activity of the heart starts in the ‘inter- The ECG waves and what they mean 2 nal pacemaker’, which is called the sinoatrial node. This Interpretation starts here! 4 is in the right atrium. The normal rhythm is called ‘sinus rhythm’ (properly it should be called sinoatrial rhythm, Rhythms you must be able to recognize 8 but it isn’t). The way electrical impulses flow through the Patterns you must be able to recognize 10 heart is called conduction. Abnormalities in the electrical activity of the heart can The normal ECG and its variants 13 result in abnormal conduction or rhythms where the heart ECG red flags 14 may go too quickly, too slowly, or beat irregularly. Changes to the normal flow of electricity through the heart can be shown on an ECG and may indicate damaged This guide has been written for those who are just starting heart muscle. Heart muscle can be damaged by many to use ECGs in their clinical practice. -

Wide Flbs & QRS Tachycardias
Wide FLB’s and QRS Tachycardias Reading Assignment (p30-41 and 42-44) Welcome to the “5-Step Method” ECG #: Mearurements: Rhythm (s): Conduction: Waveform: Interpretation: A= V= PR= QRS= QT= Axis= 1. Compute the 5 basic measurements: HR, PR interval, QRS duration, QT interval, Axis 2. What’s the basic rhythm and other rhythm statements (e.g., PACs and PVC’s) 3. Any conduction abnormalities (SA blocks, AV blocks (Types I or II), and IV blocks 4. Waveform abnormalities beginning with P waves, QRS complexes, ST-T, and U waves 5. Final interpretations: Normal ECG or Borderline or Abnormal ECG (list final conclusions) 44 Year old man in the ER with palpitations and lightheadedness 7-1 rsR’ Mearurements: Rhythm (s): Conduction: Waveform: Interpretation: A= V=210 Wide QRS tachycardia • IVCD • rsR‘ in V1 Abnormal ECG: • Late S (rightward forces) in 1. High probability SVT with RBBB PR= I, aVL, V6 Clues: classic triphasic (rsR‘) RBBB QRS=1120 morphology in V1 is very unlikely to be VT. The most likely SVT mechanism in this QT=240 ECG is AVNRT with RBBB. 7-1 Axis= indeterminate 65 Year old man in the ICU with hypotension 7-2 qR in V1 rS in V6 Mearurements: Rhythm (s): Conduction: Waveform: Interpretation: A= V=140 Wide QRS tachycardia • IVCD • Northwest quadrant axis Abnormal ECG: (lead I and II both negative) • Left ventricular tachycardia PR= • qR pattern in V1 • rS pattern in V6 ECG Clues for VT in this case: 1) NW QRS=150 quadrant axis; 2) qR in V1; rS in V6. QT=340 Clinical clues: hypotension 7-2 Axis= -120 (NW Quadrant) I II III 7-3 75 Year old man in the ICU with recent acute coronary syndrome Mearurements: Rhythm (s): Conduction: Waveform: Interpretation: A= V= 135 Wide QRS tachycardia • IVCD • fat R in V1 (red arrows) Abnormal ECG: • Notch on downstroke of S 1. -

Long QT Syndrome: from Channels to Cardiac Arrhythmias
Long QT syndrome: from channels to cardiac arrhythmias Arthur J. Moss, Robert S. Kass J Clin Invest. 2005;115(8):2018-2024. https://doi.org/10.1172/JCI25537. Review Series Long QT syndrome, a rare genetic disorder associated with life-threatening arrhythmias, has provided a wealth of information about fundamental mechanisms underlying human cardiac electrophysiology that has come about because of truly collaborative interactions between clinical and basic scientists. Our understanding of the mechanisms that control the critical plateau and repolarization phases of the human ventricular action potential has been raised to new levels through these studies, which have clarified the manner in which both potassium and sodium channels regulate this critical period of electrical activity. Find the latest version: https://jci.me/25537/pdf Review series Long QT syndrome: from channels to cardiac arrhythmias Arthur J. Moss1 and Robert S. Kass2 1Heart Research Follow-up Program, Department of Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York, USA. 2Department of Pharmacology, Columbia University Medical Center, New York, New York, USA. Long QT syndrome, a rare genetic disorder associated with life-threatening arrhythmias, has provided a wealth of information about fundamental mechanisms underlying human cardiac electrophysiology that has come about because of truly collaborative interactions between clinical and basic scientists. Our understanding of the mecha- nisms that control the critical plateau and repolarization phases of the human ventricular action potential has been raised to new levels through these studies, which have clarified the manner in which both potassium and sodium channels regulate this critical period of electrical activity. -

Sinus Rhythm, Ectopic Beats and Tachycardia Do Ectopics Matter? the FAST-TT Protocol for Fetal Tachycardia
Sinus rhythm, ectopic beats and tachycardia Do ectopics matter? The FAST-TT protocol for fetal tachycardia London 23 January 2020 Prof Julene S Carvalho Head of Brompton Centre for Fetal Cardiology Consultant Fetal and Paediatric Cardiologist Professor of Practice, Fetal Cardiology Molecular & Clinical Sciences Research Institute, SGUL Normal and abnormal rhythm Learning objectives Normal and abnormal rhythm Learning objectives • To assess the normal cardiac rhythm Normal and abnormal rhythm Learning objectives • To assess the normal cardiac rhythm • To diagnose & manage irregular rhythm Normal and abnormal rhythm Learning objectives • To assess the normal cardiac rhythm • To diagnose & manage irregular rhythm • To diagnose & manage tachycardia Abnormal rhythm Learning objectives • To assess the normal cardiac rhythm Rhythm Sinus rhythm • regular • 1 atrial : 1 ventricular activity • constant AV timing (PR interval) Sinus rhythm Sinus rhythm Sinus rhythm Sinus rhythm ‘Eye-balling’ ‘Eye-balling’ Rhythm Study of rhythm (sinus or arrhythmia) • Based on simultaneous recording of atrial and ventricular activity Fetal arrhythmias Diagnostic modalities in the fetus Simultaneous recording Ultrasound • M-mode • Pulsed wave Doppler • Tissue Doppler Fetal magnetocardiography Fetal electrocardiography Fetal arrhythmias Diagnostic modalities in the fetus Simultaneous recording Ultrasound • M-mode • Pulsed wave Doppler • Tissue Doppler Sinus rhythm M-mode echocardiography LV V RA A Sinus rhythm Pulmonary vessels Carvalho et al. Heart 2007;93:1448-53 (Epub 2006 Dec 12) Simultaneous pulmonary artery and vein Methods • At the level of the 4-chamber view • Colour flow mapping: artery and vein • Inner 2/3 of lung parenchyma • Sample volume over artery and vein • Low velocity • (Absence of fetal breathing movement) Carvalho et al. -

Young Adults. Look for ST Elevation, Tall QRS Voltage, "Fishhook" Deformity at the J Point, and Prominent T Waves
EKG Abnormalities I. Early repolarization abnormality: A. A normal variant. Early repolarization is most often seen in healthy young adults. Look for ST elevation, tall QRS voltage, "fishhook" deformity at the J point, and prominent T waves. ST segment elevation is maximal in leads with tallest R waves. Note high take off of the ST segment in leads V4-6; the ST elevation in V2-3 is generally seen in most normal ECG's; the ST elevation in V2- 6 is concave upwards, another characteristic of this normal variant. Characteristics’ of early repolarization • notching or slurring of the terminal portion of the QRS wave • symmetric concordant T waves of large amplitude • relative temporal stability • most commonly presents in the precordial leads but often associated with it is less pronounced ST segment elevation in the limb leads To differentiate from anterior MI • the initial part of the ST segment is usually flat or convex upward in AMI • reciprocal ST depression may be present in AMI but not in early repolarization • ST segments in early repolarization are usually <2 mm (but have been reported up to 4 mm) To differentiate from pericarditis • the ST changes are more widespread in pericarditis • the T wave is normal in pericarditis • the ratio of the degree of ST elevation (measured using the PR segment as the baseline) to the height of the T wave is greater than 0.25 in V6 in pericarditis. 1 II. Acute Pericarditis: Stage 1 Pericarditis Changes A. Timing 1. Onset: Day 2-3 2. Duration: Up to 2 weeks B. Findings 1. -

Basic Rhythm Recognition
Electrocardiographic Interpretation Basic Rhythm Recognition William Brady, MD Department of Emergency Medicine Cardiac Rhythms Anatomy of a Rhythm Strip A Review of the Electrical System Intrinsic Pacemakers Cells These cells have property known as “Automaticity”— means they can spontaneously depolarize. Sinus Node Primary pacemaker Fires at a rate of 60-100 bpm AV Junction Fires at a rate of 40-60 bpm Ventricular (Purkinje Fibers) Less than 40 bpm What’s Normal P Wave Atrial Depolarization PR Interval (Normal 0.12-0.20) Beginning of the P to onset of QRS QRS Ventricular Depolarization QRS Interval (Normal <0.10) Period (or length of time) it takes for the ventricles to depolarize The Key to Success… …A systematic approach! Rate Rhythm P Waves PR Interval P and QRS Correlation QRS Rate Pacemaker A rather ill patient……… Very apparent inferolateral STEMI……with less apparent complete heart block RATE . Fast vs Slow . QRS Width Narrow QRS Wide QRS Narrow QRS Wide QRS Tachycardia Tachycardia Bradycardia Bradycardia Regular Irregular Regular Irregular Sinus Brady Idioventricular A-Fib / Flutter Bradycardia w/ BBB Sinus Tach A-Fib VT PVT Junctional 2 AVB / II PSVT A-Flutter SVT aberrant A-Fib 1 AVB 3 AVB A-Flutter MAT 2 AVB / I or II PAT PAT 3 AVB ST PAC / PVC Stability Hypotension / hypoperfusion Altered mental status Chest pain – Coronary ischemic Dyspnea – Pulmonary edema Sinus Rhythm Sinus Rhythm P Wave PR Interval QRS Rate Rhythm Pacemaker Comment . Before . Constant, . Rate 60-100 . Regular . SA Node Upright in each QRS regular . Interval =/< leads I, II, . Look . Interval .12- .10 & III alike .20 Conduction Image reference: Cardionetics/ http://www.cardionetics.com/docs/healthcr/ecg/arrhy/0100_bd.htm Sinus Pause A delay of activation within the atria for a period between 1.7 and 3 seconds A palpitation is likely to be felt by the patient as the sinus beat following the pause may be a heavy beat. -

Rhythms & Cardiac Emergencies
Rhythm & 12 Lead EKG Review March 2011 CE Condell Medical Center EMS System Site code # 107200E-1211 Prepared by: FF/PMD Michael Mounts – Lake Forest Fire Revised By: Sharon Hopkins, RN, BSN, EMT-P Objectives Upon successful completion of this module, the EMS provider will be able to: • Identify the components of a rhythm strip • Identify what the components represent on the rhythm strip • Identify criteria for sinus rhythms • Identify criteria for atrial rhythms • Identify AV/junctional rhythms Objectives cont. • Identify ventricular rhythms • Identify rhythms with AV blocks • Identify treatments for different rhythms • Identify criteria for identification of ST elevation on 12 lead EKG’s • Identify EMS treatment for patients with acute coronary syndrome (ST elevation) • Demonstrate standard & alternate placement of ECG electrodes for monitoring Objectives cont. • Demonstrate placement of electrodes for obtaining a 12 lead EKG • Demonstrate the ability to identify a variety of static or dynamic EKG rhythm strips • Demonstrate the ability to identify the presence or absence of ST elevation when presented with a 12 lead EKG • Review department’s process to transmit 12 lead EKG to hospital, if capable • Successfully complete the post quiz with a score of 80% or better. ECG Paper • What do the boxes represent? • How do you measure time & amplitude? Components of the Rhythm Strip • ECG Paper • Wave forms • Wave complexes • Wave segments • Wave intervals Wave Forms, Complexes, Segments & Intervals • P wave – atrial depolarization • QRS – Ventricular