Complete Issue (PDF)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
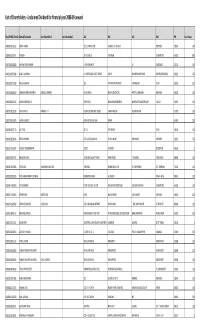
List of Share to Be Transferred to IEPF.Xlsx
List of Shareholders ‐ Unclaimed Dividend for financial year 2008‐09 onward Folio/DP‐ID & Client ID Name of Shareholder Joint Shareholder 1 Joint Shareholder 2 AD1 AD2 AD3 AD4 PIN No of shares IN30009510512622 SHANTI TOMAR 125, HUMAYUN PUR SAFDARJUNG ENCLAVE NEW DELHI 110029 100 IN30009511023704 P SURESH 28 R R LAYOUT R S PURAM COIMBATORE 641001 1000 IN30011810558083 SHIV RAJ SINGH SHARMA V P.O. MAKANPUR UP GHAZIABAD 201010 100 IN30011810706380 NAND LAL MENANI C O KASTURI BAI COLD STORAGE HAPUR BULANDSHAHAR ROAD HAPUR (GHAZIABAD) 245101 100 IN30011810772083 RAHUL AGRAWAL 362 SITA RAM APARTMENTS PATPARGANJ DELHI 110092 200 IN30011810804832 SARBINDER SINGH SAWHNEY HARLEEN SAWHNEY HOUSE NO 65 WEST AVENUE ROAD WEST PUNJABI BAGH NEW DELHI 110026 200 IN30011810878226 ASHOK KUMAR MALIK S/W 393/14 NEAR MAHABIR MANDIR MAIN BAZAR BAHADUR GARH JHAJJAR 124507 100 IN30017510122592 VIJI KANNAN. K KANNAN. K. R 4/146 A SECOND MAIN STREET SHANTHI NAGAR PALAYANKOTTAI 627002 100 IN30017510155076 SATISH KUMAR. D INDIAN OVERSEAS BANK ANNUR 641653 200 IN30020610257473 M L GOYAL QP ‐ 31 PITAMPURA DELHI 110034 100 IN30020610296246 DEEPAK SHARMA FLAT‐3, SOOD BUILDING TEL MILL MARG RAM NAGAR NEW DELHI 110055 700 IN30021413290147 GUDURU SUBRAMANYAM 10/471 K K STREET PRODDATUR 516360 1 IN30023910397325 BALAMURUGAN V 1073/133H, MILLAR PURAM ANNA NAGAR TUTUCORIN TAMIL NADU 628008 200 IN30026310156836 SUTAPA SEN SAMARESH KUMAR SEN TURI PARA DIGHIRPAR,N.C.PUR PO‐ RAMPURHAT DIST‐ BIRBHUM 731224 100 IN30034320058199 PATEL HARGOVANBHAI VELABHAI LIMDAWALO MADH JAL CHOWK -

The Monthly Hindu Review | Current Affairs | August 2021 1 Www
The Monthly Hindu Review | Current Affairs | August 2021 1 www.bankersadda.com | www.sscadda.com | www.careerpower.in | Adda247 App The Monthly Hindu Review | Current Affairs | August 2021 Contents The Most Important Current Affairs August 2021 ................................................................................................... 3 Banking and Financial Current Affairs ..................................................................................................................... 8 Economy Current Affairs ...........................................................................................................................................10 Business Current Affairs ............................................................................................................................................11 International Current Affairs ....................................................................................................................................12 National Current Affairs ............................................................................................................................................14 States Current Affairs .................................................................................................................................................16 Schemes/Committees ..................................................................................................................................................18 Agreement/Memorandum of Understanding (MoU) .............................................................................................19 -

India's Limited War Doctrine: the Structural Factor
IDSA Monograph Series No. 10 December 2012 INDIA'S LIMITED WAR DOCTRINE THE STRUCTURAL FACTOR ALI AHMED INDIA’S LIMITED WAR DOCTRINE: THE STRUCTURAL FACTOR | 1 IDSA Monograph Series No. 10 December 2012 INDIA’S LIMITED WAR DOCTRINE THE STRUCTURAL FACTOR ALI AHMED 2 | ALI AHMED Institute for Defence Studies and Analyses, New Delhi. All rights reserved. No part of this publication may be reproduced, sorted in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photo-copying, recording or otherwise, without the prior permission of the Institute for Defence Studies and Analyses (IDSA). ISBN: 978-93-82169-09-3 Disclaimer: The views expressed in this Monograph are those of the author and do not necessarily reflect those of the Institute or the Government of India. First Published: December 2012 Price: Rs. Published by: Institute for Defence Studies and Analyses No.1, Development Enclave, Rao Tula Ram Marg, Delhi Cantt., New Delhi - 110 010 Tel. (91-11) 2671-7983 Fax.(91-11) 2615 4191 E-mail: [email protected] Website: http://www.idsa.in Layout & Cover by: Vaijayanti Patankar Printed at: INDIA’S LIMITED WAR DOCTRINE: THE STRUCTURAL FACTOR | 3 To Late Maj Gen S. C. Sinha, PVSM 4 | ALI AHMED INDIA’S LIMITED WAR DOCTRINE: THE STRUCTURAL FACTOR | 5 CONTENTS ACKNOWLEDGEMENTS .......................... 7 1. INTRODUCTION .................................... 9 2. DOCTRINAL CHANGE ............................. 16 3. THE STRUCTURAL FACTOR .................. 42 4. CONCLUSION ....................................... 68 REFERENCES ......................................... 79 6 | ALI AHMED * INDIA’S LIMITED WAR DOCTRINE: THE STRUCTURAL FACTOR | 7 ACKNOWLEDGEMENTS This monograph is the outcome of my fellowship at IDSA in 2010- 12. -

Cold Start – Hot Stop? a Strategic Concern for Pakistan
79 COLD START – HOT STOP? A STRATEGIC CONCERN FOR PAKISTAN * Muhammad Ali Baig Abstract The hostile environment in South Asia is a serious concern for the international players. This volatile situation is further fuelled by escalating arms race and aggressive force postures. The Indian Cold Start Doctrine (CSD) has supplemented negatively to the South Asian strategic stability by trying to find a way in fighting a conventional limited war just below the nuclear umbrella. It was reactionary in nature to overcome the shortcomings exhibited during Operation Parakram of 2001-02, executed under the premise of Sundarji Doctrine. The Cold Start is an adapted version of German Blitzkrieg which makes it a dangerous instrument. Apart from many limitations, the doctrine remains relevant to the region, primarily due to the attestation of its presence by the then Indian Army Chief General Bipin Rawat in January 2017. This paper is an effort to probe the different aspects of Cold Start, its prerequisites in provisions of three sets; being a bluff based on deception, myth rooted in misperception, and a reality flanked by escalation; and how and why CSD is a strategic concern for Pakistan. Keywords: Cold Start Doctrine, Strategic Stability, Conventional Warfare, Pakistan, India. Introduction here is a general consensus on the single permanent aspect of international system T that has dominated the international relations ever since and its history and relevance are as old as the existence of man and the civilization itself; the entity is called war.1 This relevance was perhaps best described by Leon Trotsky who averred that “you may not be interested in war, but war may be interested in you.”2 To fight, avert and to pose credible deterrence, armed forces strive for better yet flexible doctrines to support their respective strategies in conducting defensive as well as offensive operations and to dominate in adversarial environments. -

NPRC) VIP List, 2009
Description of document: National Archives National Personnel Records Center (NPRC) VIP list, 2009 Requested date: December 2007 Released date: March 2008 Posted date: 04-January-2010 Source of document: National Personnel Records Center Military Personnel Records 9700 Page Avenue St. Louis, MO 63132-5100 Note: NPRC staff has compiled a list of prominent persons whose military records files they hold. They call this their VIP Listing. You can ask for a copy of any of these files simply by submitting a Freedom of Information Act request to the address above. The governmentattic.org web site (“the site”) is noncommercial and free to the public. The site and materials made available on the site, such as this file, are for reference only. The governmentattic.org web site and its principals have made every effort to make this information as complete and as accurate as possible, however, there may be mistakes and omissions, both typographical and in content. The governmentattic.org web site and its principals shall have neither liability nor responsibility to any person or entity with respect to any loss or damage caused, or alleged to have been caused, directly or indirectly, by the information provided on the governmentattic.org web site or in this file. The public records published on the site were obtained from government agencies using proper legal channels. Each document is identified as to the source. Any concerns about the contents of the site should be directed to the agency originating the document in question. GovernmentAttic.org is not responsible for the contents of documents published on the website. -

The Korean War
N ATIO N AL A RCHIVES R ECORDS R ELATI N G TO The Korean War R EFE R ENCE I NFO R MAT I ON P A P E R 1 0 3 COMPILED BY REBEccA L. COLLIER N ATIO N AL A rc HIVES A N D R E C O R DS A DMI N IST R ATIO N W ASHI N GTO N , D C 2 0 0 3 N AT I ONAL A R CH I VES R ECO R DS R ELAT I NG TO The Korean War COMPILED BY REBEccA L. COLLIER R EFE R ENCE I NFO R MAT I ON P A P E R 103 N ATIO N AL A rc HIVES A N D R E C O R DS A DMI N IST R ATIO N W ASHI N GTO N , D C 2 0 0 3 United States. National Archives and Records Administration. National Archives records relating to the Korean War / compiled by Rebecca L. Collier.—Washington, DC : National Archives and Records Administration, 2003. p. ; 23 cm.—(Reference information paper ; 103) 1. United States. National Archives and Records Administration.—Catalogs. 2. Korean War, 1950-1953 — United States —Archival resources. I. Collier, Rebecca L. II. Title. COVER: ’‘Men of the 19th Infantry Regiment work their way over the snowy mountains about 10 miles north of Seoul, Korea, attempting to locate the enemy lines and positions, 01/03/1951.” (111-SC-355544) REFERENCE INFORMATION PAPER 103: NATIONAL ARCHIVES RECORDS RELATING TO THE KOREAN WAR Contents Preface ......................................................................................xi Part I INTRODUCTION SCOPE OF THE PAPER ........................................................................................................................1 OVERVIEW OF THE ISSUES .................................................................................................................1 -

The Operational Role of British Corps Command on the Western Front, 1914-18
The Operational Role of British Corps Command on the Western Front, 1914-18 Andrew Simpson University College, London Submitted for the Degree of Doctor of Philosophy © Abstract British corps command having been neglected in the literature, this thesis sets out to assess what British corps did, and how they did it, on the Western Front during the Great War. It attempts to avoid anecdotal sources as much as possible, drawing its evidence instead as much as possible from contemporary official documents. It is a central argument here that Field Service Regulations, Part 1 (1909), was found by commanders in the BEF to be applicable throughout the war, because it was designed to be as flexible as possible, its broad principles being supplemented by training and manuals. Corps began the war in a minor role, as an extra level of command to help the C-in-C control the divisions of the BEF. With the growth in numbers and importance of artilleiy in 1915, divisions could not cope with the quantity of artilleiy allotted theni, and by early 1916, the corps BGRA became the corps artilleiy commander (GOCRA). In addition to its crucial role in artillery control, corps was important as the highest level of operational command, discussing attack plans with Armies and divisions and being responsible for putting Army schemes into practice. Though corps tended to be prescnptive towards divisions in 1916, and Armies towards corps, a more hands-off style of command was generally practised in 1917, within the framework of FSR and the pamphlet SS13S (and others - to be used with FSR). -

XII Corps History & Personnel
2020 www.BritishMilitaryHistory.co.uk Author: Robert PALMER, M.A. A CONCISE HISTORY OF: XII CORPS (HISTORY & PERSONNEL) A concise history of XII Corps, a higher level formation of the British Army in existence from 1940 until 1945. It saw operational service in North West Europe in 1944 and 1945. In addition, known details of the key appointments held during that period are included. Copyright ©www.BritishMilitaryHistory.co.uk (2020) 15 June 2020 [XII CORPS HISTORY & PERSONNEL] A Concise History of XII Corps (History & Personnel) Version: 1_1 This edition dated: 15 June 2020 ISBN: Not yet allocated. All rights reserved. No part of the publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means including; electronic, electrostatic, magnetic tape, mechanical, photocopying, scanning without prior permission in writing from the publishers. Author: Robert PALMER, M.A. (copyright held by author) Assisted by: Stephen HEAL Published privately by: The Author – Publishing as: www.BritishMilitaryHistory.co.uk © www.BritishMilitaryH istory.co.uk Page 1 15 June 2020 [XII CORPS HISTORY & PERSONNEL] XII Corps The XII Corps was formed in the United Kingdom circa June 1940. The first commanding officer of the Corps was Lieutenant General Andrew THORNE. XII Corps was stationed in the south east of England in the counties of Kent and Sussex, and had its headquarters located at 10, Broadwater Down in Royal Tunbridge Wells, Kent. The first formations it had under command were: • 45th Infantry Division, • 1st London Infantry Division. The 1st London Division was renamed as the 56th (1st London) Infantry Division on 18 November 1940. -

The 1 and 2D Balkan Wars
L’Armee Francaise Vol III THE 1 ST October 1 October AND2D BALKAN WARS 912 912 – September September 1913 1 L’Armee Francaise Vol III “By the grace of God, I have therefore ordered my brave army to join in the Holy War to free our brethren and to ensure a better future. In Old Serbia, my army will meet not only upon Christian Serbs, but also upon Muslim Serbs, who are equally dear to us, and in addition to them, upon Christian and Muslim Albanians with whom our people have shared joy and sorrow for thirteen centuries now. To all of them we bring freedom, brotherhood and equality.” King Peter I of Serbia, 18 October 1912 On the cover, “Na Nozh!” By Bayonet, Bulgarians over running Turkish positions, 1912, Czech painter Jaroslav Vesin, 1913 and in the Public Domain. 2 L’Armee Francaise Vol III Age of Valor Age of Eagles II Expansion Module for European Warfare by Blood and Iron, 1848 thru 1914 The 1st & 2d Balkan Wars Table of Contents SUBJECT Page SUBJECT PAGE FRANCO-PRUSSIAN WAR IMPERIAL PERIOD….…. * INTRODUCTION …………………………….….… * Battle of Borney-Colombey………... * THE CARLIST WARS ……………………….…... * FRANCO-PRUSSIAN WAR REPUBLICAN PERIOD… * Battle of Mendigorria…………….… * Battle of Colmiers……………………. * HUNGARIAN REVOLUTION ……………………... * RUSSO-TURKISH WAR…………………………… * Battle of Isaszag…………………….. * Siege of Plevna………………………. * 1ST ITALIAN WAR OF INDEPENDENCE………….. * RUSSO-JAPANESE WAR…………………………. * Battle of Novara……………………. * Battle of Telissu……………………… * 5 THE SCHLESWIG – HOLSTEIN QUESTION………. * BALKAN WARS………………………………….. 9 Battle of Isted………………………… * Battle of Lule-Burgas ….…………… THE GUNS OF AUGUST, 1914……………………. * CRIMEAN WAR………………………………….. * Western Front, Battle of Charleroi... * Battle of the Alma………………….. * Eastern Front, Battle of Kladowa…. -

World War II Operations Reports 1940-1948
Records of the Adjutant General's Office (RG407) World War II Operations Reports 1940-1948 陸軍省高級副官部文書 第二次世界大戦作戦記録 I Corps 第 1 軍団 Box 3017 – Box 3112 国立国会図書館憲政資料室 2007 年 11 月 PDF ファイル作成 2008 年 2 月書式改訂 Records of the Adjutant General's Office; World War II Operations Reports 1940-1948 (陸軍省高級副官部文書/第二次世界大戦作戦記録) Series: I Corps Box no. (Folder no.): 3017(1) Folder title: 201-0: History - Biak Operation - I Corps (15 - 27 Jun 1944) Date: 1944/?-?/? Item description: Title: "History of the Biak Operation: Beach Defense Cave, Biak Island". Includes Standard Photo. Includes Map. Note: Microfiche no.: WOR 21272-21274 Box no. (Folder no.): 3017(2) Folder title: 201-0.1: History - I Corps (1918 - 1945) Date: 1945/06-?/? Item description: Note: Microfiche no.: WOR 21275 Box no. (Folder no.): 3017(3) Folder title: 201-0.1: History - I Corps (1862 - 1948) Date: 1948/01-1948/01 Item description: 愛知 京都 兵庫 和歌山 広島 Note: Microfiche no.: WOR 21276 Box no. (Folder no.): 3017(4) Folder title: 201-0.2: History - Luzon Campaign - I Corps (9 Jan - 4 Jul 1945) Date: 1945/?-?/? Item description: [336 p.] Includes Standard Photo. Includes Map. Note: Microfiche no.: WOR 21276-21279 Box no. (Folder no.): 3017(5) Folder title: 201-0.2: (21451) I Corps - Occupation of Japan (25 Sep - 30 Nov 1945) Date: 1945/?-?/? Item description: Title: "History of the Occupation of Japan, 1945" / [200 p.] / Includes Map. / 富山 石 川 福井 岐阜 静岡 愛知 三重 Note: Microfiche no.: WOR 21279-21282 Box no. (Folder no.): 3017(6) Folder title: 201-0.2: I Corps - History of Occupation of Japan (1 Dec 1945 - 31 Jan 1946) Date: 1946/?-?/? Item description: Title: "I Corps, History of Occupation of Japan, 1 Dec 1945 - 31 Jan 1946" / [149 p.] / Includes Map. -

~*/T~HTANK Ml'846~1 13
r ., ,,.- j' '..o.t", ". /; J t.". ..:-,1,1' ! AAR#640 U i Ii AF!ER ACTION REPORT \ .:~*/t~HTANK ml'846~1 13 d) Sept 43 thru , ' \ 1 July 45 f . , . , , I . i (, ! f , ) i {: ./ J ::-\~., \ -r:His DoCm~T IS '!rlE PRqPE,RTI,'Of\"ANDi·SHOULD BE RETURNfl.l TID, ;\:-~.f' ,,' " I,,:" / .' . (. I; , 'V\Il !,nfE 'C~A$SIFIED'DPCUUENT SECTlPE, IN'f'ALLIGEUCE DIVISION, S-2, , \ ' BUI~n~G T-5, (T-1782);.· , I I 'I~, i ," ': I, " , \ ( ',~ ". ,I :<, -' i, . I f t;., I"' ' .... ,; -, AFTER ACTION REPORT,-' 95TH~"Fm.n ,/' ARTnwty,BA.TTALION FIFTH ARMORED DIVISION 1 AUGtJST~ 1944 tbru 9 -MAY, 1945 t THIS DOCUJmNT IS THE PROPERTY OF, 00 smum BE RETURNED TO " I THE CLASSIFIl!D DOOUMENT SECTION, INTELLIGENCE DIVISION, S-2, BUILDING T-5, (T-1782). / .,. ~,- o o -...,..._. • - ~- •. ---"r•. 77S1I,TANKBN.. 20 SEPTEMBER 1943 TO J- JULY 19Q5 J . , .-' ' V _J'- "-..::' _- ,'I CA.~CELLFD BY-AUTHORITY OF THE ADJUTANT GENDlAL w.....lLC....--. b T o-ft--. t .-rh r- ~".t-. DOWNGRADING COMMlll~.z ~ ~..Lj(..tbl .............................. ~ } A , .J .. J 3 O.1io~1'~. U&1" .....17 of "111. oraai_tioa.. 10lfi w. w~ .. / Major. CaT'alrr. /, _ T CbnnaDding~ . 1-Ino1. Ino1 - UD.1t,S£eto!7 with supporting doc\III.cte (loA 4yP). v '/ .. ---....-. ---If 1'.,/ '" 1· .. --.......,1 .- CHltONOlOGlCAL HISTORY " The 1st Battalion, )6th.ArIIored Regiaent, 8th A1'aorell DLTis10n was activated at Fort Knox, Kentucq on 1 April 1942. It was a licht tank organization wi~h the u1n dut7 ot tra:1Di.Dg cadres tor tlle tom 1ng of armored units . -

Indian Military's Cold Start Doctrine
1 Indian Military’s Cold Start Doctrine: Capabilities, Limitations and Possible Response from Pakistan By Masood Ur Rehman Khattak SASSI Research Paper 32 March 2011 Published by South Asian Strategic Stability Institute (SASSI), 36 Alie Street, London, E1 8DA South Asian Strategic Stability Institute (SASSI) 2011 2 List of Acronyms AWACS Airborne Warning and Control System ABM Anti Ballistic Missile AEW Airborne Early Warning BFSRs Battlefield Surveillance Radars C4ISR Command, Control, Communication, Computers, Intelligence Surveillance and Reconnaissance CSD Cold Start Doctrine C4I Command, Control, Communications, Computers and Intelligence CAG Comptroller Auditor General CDS Chief of Defense Staff DGMO Director-General of Military Operations EW Electronic Warfare FATA Federally Administered Tribal FMCP Force Multiplication Command Post FPD Fire Power Demonstration HQ-9 Hongqi-9 ISRO Indian Space Research Organisation IPKF Indian Peace Keeping Force IBGs Integrated Battle Groups IAF Indian Air Force JCSC Joint Chiefs of Staff Committee LORROS Long-Range Recce and Observation Systems MBT Main Battle Tank NCW Network Centric Warfare NBC Nuclear-Biological- Chemical NCOs Non Commissioned Officers OIC Organisation of Islamic Conference PAF Pakistan Air Force RAPID Reorganized Army Plains Infantry Division SAM Surface to Air Missiles SCO Shengai Cooperation Organisation SIPRI Stockholm International Peace Research Institute UAVs Unmanned Aerial Vehicles UN United Nations US United States WLRs Weapons Locating Radars 3 Contents List of Acronyms 02 Abstract 05 1. Introduction 06 2. Indian Military’s Cold Start Doctrine- (CSD) 06 3. Indian Military’s Capabilities for the Implementation 11 Of Cold Start Doctrine 4. Indian Military Exercise from 2004-2010 14 4.1. Exercise Divya Astra- 2004 14 4.2.